INTRODUCTION
The purpose of CPR is to temporarily provide effective oxygenation of vital organs, especially the brain and heart, through artificial circulation of oxygenated blood until the restoration of normal cardiac and respiratory activity occurs. The intended effect is to stop the degenerative processes of ischemia and anoxia caused by inadequate circulation and inadequate oxygenation.1 A key component of the 2005 American Heart Association guidelines was the recognition that immediate high-quality CPR is crucial for optimal patient outcome after sudden cardiac arrest.2 However, the 2010 American Heart Association guidelines identify several barriers to providing immediate high-quality CPR and address them.3 Furthermore, even after defibrillation, most victims demonstrate asystole or pulseless electrical activity for several minutes, and high-quality CPR immediately following defibrillation can convert nonperfusing rhythms to perfusing rhythms.2,3 The time sensitivity of CPR in sudden cardiac death is emphasized in the American Heart Association “Chain of Survival” (Table 22-1).
| Links in Chain | Comment |
|---|---|
| Immediate recognition/early access | Phone 911 (or local emergency medical telephone number).* Early recognition of the emergency and activation of the EMS or local emergency response system. |
| Early CPR | Immediate bystander CPR can double or triple the victim’s chance of survival from ventricular fibrillation. |
| Early defibrillation | CPR plus defibrillation within 3 to 5 min of collapse can produce survival rates as high as 49%–75%. |
| Early advanced care | Postresuscitation care delivered by healthcare providers. |
| Postarrest care | High-quality, integrated post–cardiac arrest clinical care. |
This chapter reviews basic CPR for adults and children ≥8 years old, including the approach to an unresponsive patient; the physiology and mechanics of closed chest compression techniques; and basic airway opening procedures, including initial management of an obstructed airway. This chapter is specifically directed toward healthcare providers, although key updates for lay rescuers are noted, given the healthcare provider’s role in layperson education.
SUMMARY OF KEY UPDATES TO PREVIOUS ALGORITHMS
“Look, listen, and feel” has been removed from all algorithms.3 Simply put, subjectivity plays too large a role in this step and has been shown to lead to delays. Immediate high-quality CPR is strongly emphasized, and should begin in any person who is unresponsive without respirations or with abnormal breathing.
Lone rescuers no longer follow the “ABCs.” The sequence “CAB” has been adopted instead. Two rescue breaths are no longer recommended prior to initiating chest compressions.
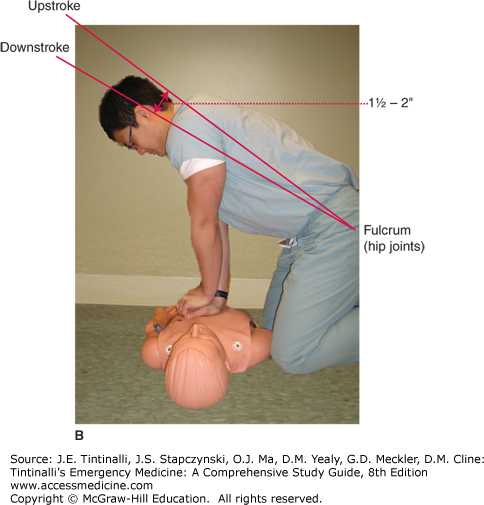
Compression rate should be at least 100/minute, not approximately 100/minute.
Compression depth should be at least 2 inches, not 1½ to 2 inches.
Untrained bystanders should begin “compression only” CPR, “hard and fast” in the center of the chest. They may be directed to do so by EMS or by a healthcare provider. This effectively removes the barrier of lack of training or fear of having to perform mouth-to-mouth resuscitation on a stranger.
Pulse checks are deemphasized for all rescuers, with a maximum of 10 seconds allowable for a pulse check. End-tidal carbon dioxide monitoring, when available, is superior to pulse checks, showing an abrupt rise in end-tidal carbon dioxide when spontaneous circulation has returned.
For trained rescuers delivering breaths, cricoid pressure is no longer recommended.
Postresuscitation care, including therapeutic hypothermia, consideration of cardiac catheterization, and hemodynamic optimization, is emphasized.
Table 22-2 outlines the sequence of steps to be taken when someone is found unresponsive.
| CPR Steps | Comments |
|---|---|
| Step 1: Recognition | Assess for responsiveness, lack of breathing, or presence of abnormal breathing/gasping. Continue to step 2. |
| Step 2: Phone 911 and get an automatic external defibrillator | If possible, call for an assistant to do so. If no assistant is available and underlying etiology is asphyxia (e.g., drowning), call 911.* Automatic external defibrillator may be delayed to provide five cycles (or 2 min) of CPR. |
| Step 3: Assess circulation (healthcare provider only) | If no pulse after 10-second maximum check, go to step 4. (Pulse checks are for healthcare providers only.) |
| Step 4: Begin cycle of 30 closed chest compressions and two breaths | Compressions: “Push hard and fast.” At least 100 compressions/min. Compress at least 5 cm (at least 2 in.). Allow for complete chest recoil, and minimize frequency and duration of interruptions. Ratio of 30 compressions to two breaths. |
| Step 5: Use the defibrillator when available and indicated | Healthcare provider to consider providing five cycles (or 2 min) of CPR before defibrillation for unwitnessed arrest. This recommendation is especially important when the interval from the call to scene response is >4 min. Provide five cycles (or 2 min) of CPR between rhythm checks during treatment of pulseless arrest. |
| Step 6: Rescue breathing | Rescue breaths can be initiated once chest compressions have been started. Deliver each breath over 1 second with sufficient tidal volume to see a visible chest rise. Continue 30 closed chest compressions and two breaths, minimizing interruptions. |
Before approaching a collapsed individual, assess the scene for risks to healthcare providers. Potential risks include the presence of hazardous materials, an unstable physical environment, or personal violence. Once the patient is reached, determine the patient’s level of responsiveness to noxious stimuli. If the patient is without normal breathing, get help first before starting chest compressions. In a hospital, this may mean calling for the arrest team and requesting the arrest cart. Outside the hospital, this is likely to mean asking a bystander to activate the local EMS system. Look around to see if an automatic external defibrillator is nearby. Rapid application of defibrillation for unstable ventricular tachycardia or ventricular fibrillation is critical for patient survival.
The carotid artery is generally the most reliable and accessible location to palpate a pulse. The artery is located by placing two fingers on the trachea and then sliding them down to the groove between the trachea and the sternocleidomastoid muscle. Simultaneous palpation of both carotid arteries should not be performed because, in low-pressure states, this could obstruct cerebral blood flow and may interfere with the ability to detect a pulse. The femoral artery may be used as an alternative site to palpate a pulse. This can be found just below the inguinal ligament approximately halfway between the anterior superior iliac spine and the pubic tubercle. If no definite pulse is felt within 10 seconds, chest compression should begin.
There has been an active debate as to the exact mechanism that causes blood flow since the technique of closed chest compressions was put forth in the 1960s.4,5 In a closed system, liquid flows when pressure gradients develop. There are three basic theories for how pressure gradients and flow are produced during closed chest cardiac massage.6,7 The conventional theory of blood flow during compressions is called the cardiac pump theory. The pump theory postulates that direct compression of the heart between the spine and the sternum leads to increased pressure in the ventricles. This causes closure of the mitral and tricuspid valves, leading to blood flow into the aorta and the pulmonary arteries. The thoracic pump theory postulates that compressions lead to an increase in pressure throughout the thoracic cavity, leading to a pressure gradient from intrathoracic to extrathoracic arteries. The third mechanism described is the abdominal pump theory, which has both an arterial and a venous component. The arterial component postulates blood flow into the peripheral arterial system from increased arterial pressure caused by abdominal compressions that forces blood from the abdominal aorta against the closed aortic valve. The venous component leads to blood return via the inferior vena cava from abdominal pressure. However, regardless of the mechanism, conventional chest compressions generate one fourth to one third of physiologic cardiac output. Lower ratios can be expected with delays in initiating compressions. The techniques of closed chest compression are detailed in Table 22-3.
| Closed chest compressions | Depth: At least 5 cm (at least 2 in.). Rate: At least 100/min. Allow complete recoil of the chest between compressions, with approximately equal compression and relaxation times. Minimize interruptions. |
| Ventilations | Single rescuer or two rescuers, nonintubated patient: give two breaths after every 30 compressions. Two rescuers, intubated patient: give breaths at a rate of 8–10 breaths/min. Do not pause chest compressions during ventilations. |
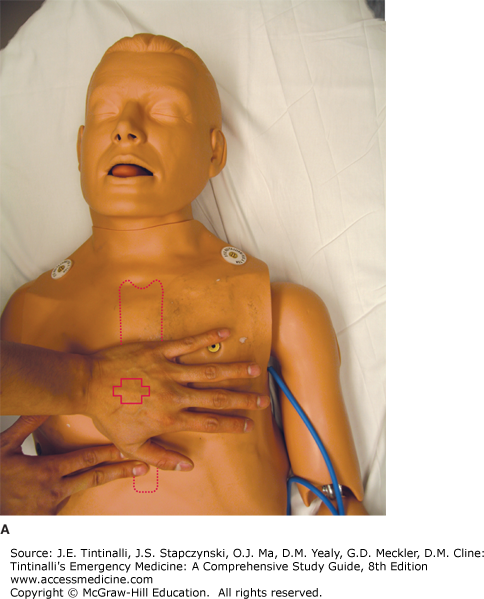
When the lack of a pulse is confirmed, begin serial rhythmic closed chest compressions. Place the victim supine on a firm surface, with the rescuer at the victim’s side. Place the heel of one hand midline on the lower half of the sternum, 4 to 5 cm (~2 in.) cephalad of the xiphoid process (Figure 22-1). The heel of the hand should be parallel with the long axis of the patient’s body. Then place the second hand on top of the first hand, so the hands are parallel with each other. The fingers of the two hands may be interlaced if desired, but they should not be touching the chest. Keep the arms straight and the elbows locked. The vector of the compression force should start from the rescuer’s shoulders and be directed downward. Lateral compressive forces will decrease the efficiency of the compressions and increase the likelihood of complications. Depress the sternum at least 5 cm (at least 2 in.) in an adult, at a rate of at least 100 compressions per minute. Rates lower than this are inadequate. The compression-release phases should be roughly equal in length. With a single rescuer or with two rescuers if the patient is not intubated, give two ventilations after every 30 compressions. With two rescuers assisting an intubated patient, ventilate at a rate of 8 to 10 per minute, without interrupting chest compressions. Of note, although assisting ventilation is important, not everyone is willing to perform mouth-to-mouth breathing due to concerns over infectious disease transmission. Chest compressions alone can be effective and should be provided even if rescue breathing is not being performed.8,9
Open chest cardiac massage is an alternative to standard CPR and improves blood flow in animal models. Although there are no data showing improved clinical outcomes with the use of open chest cardiac massage versus closed chest cardiac massage, this technique may be considered in a number of situations, including (1) after penetrating chest trauma; (2) the perioperative period before or after cardiothoracic surgery; (3) cardiac arrest caused by hypothermia, pulmonary embolism, pericardial tamponade, or abdominal hemorrhage; (4) cases of chest deformity in which closed chest CPR is ineffective; (5) penetrating abdominal trauma with deterioration and cardiac arrest; and (6) blunt trauma with cardiac arrest.10 However, the use of this technique requires a well-coordinated multidisciplinary team (see chapter 262, Cardiac Trauma).
Defibrillation is discussed in chapter 23, Defibrillation and Cardioversion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree