Fig. 33.1
Mechanism of action of surgical bariatric procedures
Based on estimated bariatric surgery numbers for 2013 published by the American Society for Metabolic and Bariatric Surgery (ASMBS), Roux-en-Y gastric bypass (RYGB), adjustable gastric band (AGB), and sleeve gastrectomy (SG) account for 90.3 % of all of the bariatric procedures performed in 2013 [17]. Of those, 88.9 % are performed laparoscopically, an approach that now represents the standard of care for bariatric surgery [16]. Although very good outcomes in terms of morbidity and mortality are achieved with this approach, many of these procedures are complex and can only be carried out by highly skilled surgeons after a steep learning curve.
Adjustable Gastric Band
Its use was primarily widespread in Australia and European countries due to its relative simplicity, reversibility, and safety profile [12]. Since the approval of the LAP-BAND® (Apollo Endosurgery, Austin, TX) system in the USA in 2001, its use has grown significantly and is now considered a well-established bariatric procedure with good medium and long-term results in terms of sustained weight loss [18, 19]. LAGB is a purely restrictive procedure that can be routinely performed in an outpatient setting; however, gastric banding is an implantable device that can be associated with late complications such as band slippage or erosion, gastric prolapse, pouch enlargement, and tubing/access port complication, which in the long term will require either band revision or explantation in a high percentage of patients [20–23].
Roux-en-Y Gastric Bypass
Laparoscopic roux-en-Y gastric bypass (RYGB) is considered the gold standard for the surgical treatment of morbid obesity due to its greater weight loss and lower rates of weight regain when compared with other bariatric procedures, becoming one of the most commonly performed bariatric surgeries in the USA [17]. This combined, malabsorptive/restrictive procedure induces weight loss by several mechanisms: by gastric restriction and early satiety, the volume of food to be consumed is decreased and ultimately the amount of caloric intake and by malabsorption which is created by bypassing the foregut delivering enteral nutrition directly into the mid small intestine avoiding the nutrient absorptive circuit. Bypassing the foregut also induces anorexia by alteration of hormone secretion [24].
Sleeve Gastrectomy
Sleeve Gastrectomy (SG), which is the fastest growing procedure in bariatric surgery [17], was first performed laparoscopically in 1999 [11]. Subsequently it was used as a first step in a staged concept for high-risk patients undergoing bariatric surgery. The rationale for this approach was to lower the morbidity of a complex surgical procedure by offering a less challenging operation, decreasing operative time, and allowing patients to lose weight before proceeding with the second stage. However, as a consequence of the proven outcomes in terms of excellent weight loss and resolution of comorbidities, it is now being increasingly favored as a stand-alone procedure [25–27]. Initially conceived of as a purely restrictive surgery, it has been shown that laparoscopic sleeve gastrectomy (LSG) has strong metabolic effects probably due to accelerated gastric emptying, early satiety, reduction of the ghrelin-producing cell mass after resection of the gastric fundus, and complex neurohormonal regulation of intestinal hormones [14, 28].
Novel Technologies in Bariatric Surgery
The Role of Robotics
The most significant impact in robotically assisted surgery was the possibility to extend the already well-known benefits achieved with minimally invasive surgery to difficult procedures often performed in an open manner. Its application in bariatric surgery amplified the benefits of minimally invasive access without increasing complication risks and with a lower learning curve.
The first bariatric procedure with robotic assistance was described by Cadière who performed a robotic-assisted adjustable gastric band placement in 1999 [29], and after that in 2001, Horgan and Vanuno published the first series of robotic-assisted RYGB [30]. Robotic technology is now applied to complex primary and revisional bariatric procedures without increasing complication risks as a result of the learning curve and overcoming the drawbacks inherent to a laparoscopic approach especially in the morbidly obese population.
Major advantages of the use of robotic technology for bariatric surgery are the greater exposure and visualization particularly useful in morbidly obese patients with excessive intra-abdominal fat deposition and oversized and fatty livers, which makes maneuverability difficult. Larger, more rigid and articulated instruments that avoid bending are an additional benefit while operating on patients with thicker abdominal walls (Fig. 33.2a, b). The possibility to perform precise maneuvers despite increased torque pressure facilitates the completion of hand-sewn gastrointestinal anastomosis, which can reduce the risk of leaks and future anastomotic strictures (Fig. 33.3a–c).
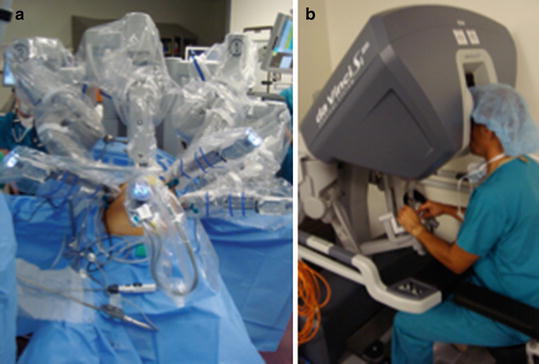
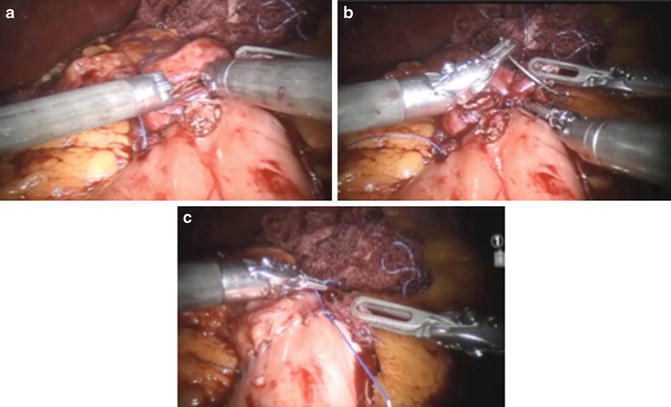
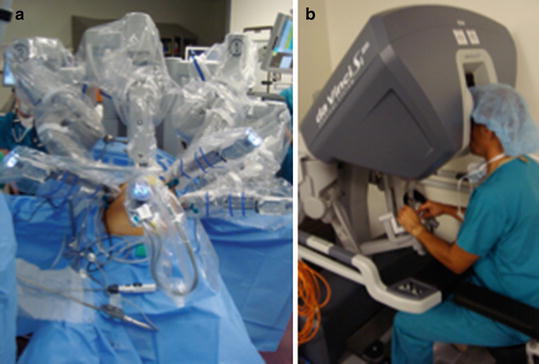
Fig. 33.2
(a, b) Robotic-assisted bariatric surgery. (a) Surgical cart over the head of the patient. (b) Surgeon at the robotic console
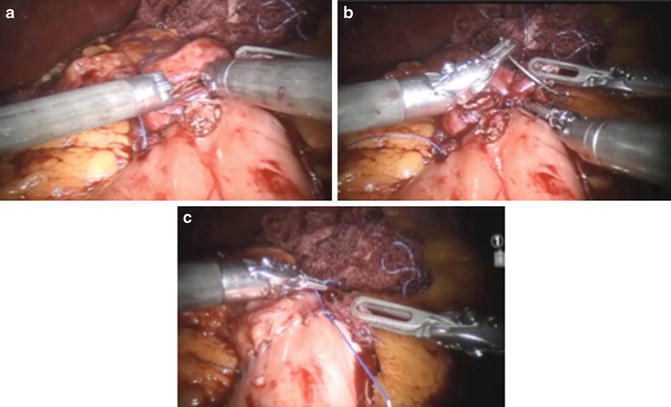
Fig. 33.3
(a–c) Robotic-assisted Roux-en-Y gastric bypass. (a) Creation of the gastrostomy and jejunostomy in preparation for the gastrojejunal anastomosis. (b) Running suture of the posterior outer layer of the gastrojejunal anastomosis. (c) Completed gastrojejunostomy
The major disadvantage is the higher operational costs compared with laparoscopic surgery [27].
Robotic Lap Band
Few studies followed the first publication of robotic-assisted lap band [31–33]. Due to the safety and effectiveness of the laparoscopic approach, the adoption of robotic-assisted LAGB continues to be scarce; however, its use for patients with preoperative BMI >50 kg/m2 was suggested to be advantageous owing to the characteristics of the robotic instruments that are longer and stiffer and with greater mechanical power. Also operative time in these patients proved to be shorter than laparoscopic counterparts [33]. Another application of the robotic platform is in the case of revisions for band slippage.
Robotic Roux-en-Y Gastric Bypass
Robotic-assisted RYGB was first introduced in 2001 [30], but its acceptance rapidly increased as its feasibility and safety have been clearly proven especially for difficult cases such as high-risk and super obese patients [33, 34]. Several systematic reviews and comparative studies reported similar or better outcomes thanks to robotic technology. Main advantages of its use for RYGB were the shorter learning curve and a lower overall complication rate but specifically for the gastrojejunostomy leak rate [31, 34].
A recent comparative study which included 389 laparoscopic and 388 robotic RYGB also showed a significantly reduced conversion rate in the robotic arm compared with the laparoscopic arm (<1 % vs. almost 5 %) although operative time was longer [34]. The same study group reported their cost analysis, which showed a clear advantage of the robotic approach by reducing complication rate and the need for postoperative radiologic studies.
Along the same line, Hagen et al. evaluated the costs of robotic versus laparoscopic RYGB. An increase in costs was observed for the laparoscopic approach, with contributing factors such as length of hospital stay, time in the ICU, complication rates, such as anastomotic leak and the use of laparoscopic staplers [35]. The robotic platform is also showing promising results in revisional surgery, where cases are considerably more complex and challenging due to the frequent occurrence of previous open approach, multiple adhesions, altered anatomy, erosions, and fistulas.
Robotic Sleeve Gastrectomy
Robotic technology for SG has not been widely adopted among bariatric surgeons due to its relatively straightforward acceptance to perform it laparoscopically; however, few series with encouraging results have been published [36–38]. The main indication for robotic assistance is represented by super and super-super obese patients, where the accomplishment of the procedure by laparoscopic approach implies a greater challenge because of the previously mentioned characteristics of the laparoscopic instruments and the patients’ abdomen [39, 40]. Although there are no reports about middle and long-term follow-up, results of robotic SG seem to be comparable to laparoscopic approach in terms of excess weight loss but with technical advantages and a reduced learning curve [36–38]. Also, this procedure represents a helpful training model for bariatric fellows and residents [38].
The Role of Single-Incision Surgery
In an effort to progress toward a less invasive and more innovative approach, the so-called scarless surgery emerged in an attempt to allow surgeons to perform laparoscopic procedures with virtually no visible scars. Those procedures were single-incision laparoscopic surgery (SILS) and natural orifice translumenal endoscopic surgery (NOTES).
Potential advantages include additional reduction of wound morbidity such as infection, hematoma, and incisional hernia, less postoperative pain, faster recovery, and further enhancing of cosmetic results (Fig. 33.4a–f).
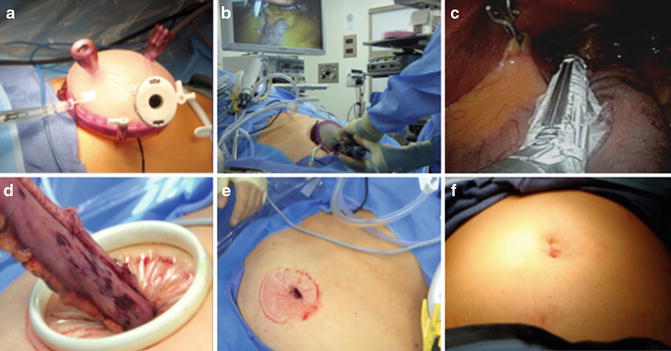
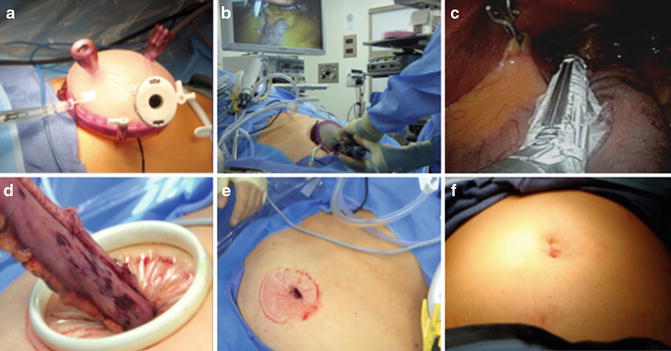
Fig. 33.4
(a–f) Single-incision laparoscopic sleeve gastrectomy. (a) Ports placement. (b) Laparoscopic instruments introduced through the single-port platform. (c) Gastric transection. The left lobe of the liver is lifted by a laparoscopic internal retractor. (d) Extraction of resected stomach after sleeve completion through the umbilical incision. (e) Umbilical incision after the single-port platform was extracted. (f) Immediate postoperative cosmetic result
Although SILS proved to be feasible, surgeons faced several challenges: the lack of instrument triangulation, the lack of optimal visualization of the operative field, internal and external friction between the instrument, and inadequate internal retraction. Hence, the widespread application of this technique came with different developments from the industry to overcome these issues such as articulating instruments, multiple access lumen, and multichannel operative platform among others.
Beginning in 2008, many groups started to report the application of a single-incision technique for bariatric procedures [41–43]. Several series demonstrated that single-incision LAGB and single-incision SG can be performed safely even with the challenges that entail operating on a morbidly obese patient. The technique was proven to be as effective and safe as conventional multiport laparoscopic approach with equivalent outcomes for weight loss [44–46]. However, patient selection is of paramount importance when performing SILS, particularly in bariatric patients. As was shown by a systematic review published in 2014 [44], the presence of super obesity, concomitant incisional hernias, previous abdominal surgeries, and a xiphoid-umbilicus distance longer than 20 cm may represent exclusion criteria for the application of this approach. Also, the common presence of an enlarged and fatty liver and its retraction are still a true challenge [46–48].
The single-incision approach was also described for more complex procedures such as RYGB, reported by Huang and colleagues in 2009 [49]. Later, in 2012 the same author published the first series with promising outcomes [50]. However, no other authors have published anything else other than case reports or technique descriptions.
Novel Technologies Outcomes
The latest systematic review and meta-analyses of robotic-assisted bariatric surgery was published in 2013 [51]. Two previous systematic reviews were published in 2011 [51] and 2012 [52], but the first one did not include SG in their analysis.
Even though the last systematic review and meta-analysis has major limitations such as the low quality of the studies, sample size, and lack of important information such as bariatric and metabolic outcomes, the study suggests that robotic bariatric surgery is feasible independently of the type of procedure performed and safe based on complications, reoperations, and 30-day postoperative mortality rates.
A lower complication profile, specifically anastomotic leak, strictures, and bleeding, a shorter learning curve, and the ease to carry out complex maneuvers such as gastrointestinal anastomosis in RYGB and vertical gastric resection in SG are named as the main advantages of robotic surgery over open and laparoscopic approaches. The main disadvantage was the cost of the robotic platform.
Thirty-day postoperative mortality was zero regardless of the procedure and the rate of postoperative complications was 4.26 % for major and 1 % for minor in RYGB and 1.2 and 0 % for SG. An updated systematic review and meta-analysis of laparoscopic and open bariatric surgery published in 2014 [53] showed a 30-day postoperative mortality rate between 0.11 and 0.07 % for RYGB and 0.50 and 0.29 % for SG. Complication rate for laparoscopic and open RYGB was 21 and 13 % for SG. Specific surgical complications were not mentioned in this meta-analysis.
The systematic review published in 2012 by Fourman and Saber compared the outcomes of robotic bariatric surgery versus laparoscopic bariatric surgery [52]. They found a mean complication rate for all robotic procedures of 10.2 % versus 12.6 % for the conventional laparoscopic approach. The learning curve was measured for RYGB and proved to be shorter for robotic than laparoscopic approach (10–15 vs. ≥100). No major differences were observed for mean hospital stay or excess body weight loss when these variables were reported. The strongest advantages of robotic surgery found in this study were the shorter learning curve, lower leak rate for gastrojejunal anastomosis, improved ergonomics, and less operator fatigue. The major drawback was also the cost of the robotic system and its maintenance.
The most recent systematic review of single-incision bariatric surgery was published by Moreno-Sanz and colleagues in 2014, and included 13 observational studies and 1 randomized control study with a total of 2,357 patients analyzed [52]. The study concluded that single-incision bariatric surgery is a feasible option when the patients are correctly selected and the procedure is carried out by an expert bariatric surgeon knowledgeable in single-incision techniques. Conversion rate to laparoscopic approach was 2.4 % for LAGB and 1.83 % for SG. No conversions were observed among the RYGB cases. The use of an additional trocar to complete the case was reported in 3 of 8 studies of LAGB, in 1 of 4 of SG, and in 1 of 2 studies for RYGB. Overall morbidity rate was 4.8 % for single-incision versus 5 % for conventional laparoscopic approach, and the predominance was for minor complications. Interestingly, no differences were observed in terms of wound complications. Mortality was 0.005 % of all single-incision cases and was represented by one case in the AGB group.
No differences were observed on percentage of weight loss and improvement of comorbidities.
The main advantages observed with single-incision approach were reduced analgesic consumption and improved cosmesis. Disadvantages were longer operative times in almost all single-incision groups. In terms of costs, no significant differences were found between groups; however, if lower morbidity rates, necessity of reoperations, and reduced length of stay associated with single-incision access are achieved, this technique could be more cost-effective.
The Future of Bariatrics
Bariatric surgery has been continually evolving to shift from open procedures to minimally invasive approaches, considering laparoscopy as the gold standard nowadays. The state-of-the-art surgeries are still changing to improve their safety profile and technique, as the case of the laparoscopic gastric plication, a similar procedure to laparoscopic sleeve gastrectomy, which involves the creation of gastric folds by a suture line to reduce the size of the stomach.
Research interests are now focused on approaches and procedures that have similar mechanisms to surgery but less invasiveness aiming at developing durable, reversible, easier, and safer treatment options. Current and ongoing studies have delivered promising results with endoscopy, endoluminal surgery, and natural orifice translumenal endoscopic surgery; however, many of those techniques are still in there study phase or are considered as experimental due to the lack of controlled data, even when they have been used for several years already (Table 33.1).
Table 33.1
Summary of bariatric emerging procedures
Procedure | Device | Indication | Status |
|---|---|---|---|
Restrictive | |||
Gastric volume reduction | |||
Endolumenal vertical gastroplasty | EndoCinch™ (C.R. Bard, Murray Hill, NJ) | Primary/revision | On market |
Intragastric restrictive implant | TERIS (BaroSense, Redwood City, CA) | Primary | Investigational not FDA approved |
Transoral gastroplasty | Sleeve stapler (TOGA®) (Satiety, Inc., Palo Alto, CA) | Primary | Investigational not FDA approved |
Endolumenal suturing | OverStitch™ (Apollo Endosurgery, Austin, TX) | Primary/revision | Clinical trials |
Endolumenal suturing | Incisionless operating platform (IPO; USGI Medical Inc., San Clemente, CA) | Primary/revision | Clinical trials |
Intragastric space occupying | |||
Intragastric balloon | BioEnterics® BIB (Carpinteria, CA), Orbera® (Apollo Endosurgery, Austin, TX) | Primary | Investigational not FDA approved |
Intragastric balloon | Heliosphere bag system | Primary | Premarket approval (PAM) application |
Intragastric balloon | Silimed gastric balloon (Rio de Janeiro, Brazil) | Primary | Investigational not FDA approved |
Intragastric balloon
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||





