Fig. 36.1
Gram positive lancet shaped diplococcic confirming Streptococcus pneumonia (Image courtesy of Dr. Valerie Ng at Alameda Health System)
During transfer of the patient from the ED, the patient developed a generalized tonic-clonic seizure and was urgently given IV lorazepam. Due to decreased level of consciousness after the seizure, the patient was intubated for airway protection and was admitted to the ICU.
Question
What additional inpatient precautions should be taken for the most likely diagnosis?
Answer
Droplet precautions for presumed acute community acquired bacterial meningitis.
This patient presented with the ‘classic triad’ for bacterial meningitis of fever, neck stiffness and altered mental status (AMS). Although the complete triad is present only 44 % of the time [1], nearly all patients with bacterial meningitis will present with one of the three findings [2]. The absence of all three of these signs in the classic triad essentially eliminates bacterial meningitis from the differential [2]. The classic physical exams for evaluation of meningeal irritation, Kernig’s and Brudzinski’s signs are not that useful as these only have 61 % sensitivity for bacterial meningitis compared to nuchal rigidity (difficulty with chin to chest or flexion of the cervical spine) which has 84 % sensitivity for bacterial meningitis [3]. While these physical exam signs may provide support in establishing the diagnosis, a lumbar puncture is still required for definitive diagnosis.
Until the specific pathogen responsible for community acquired bacterial meningitis has been identified, strong consideration should be given for initiating droplet precautions. Droplet precautions are recommended by the CDC to decrease the spread of infection caused by Neisseria meningitides and Haemophilus influenzae type b. A definitive diagnosis may be delayed for several days [4]. In addition, depending on the quality of the gram stain, differentiating between gram positive cocci and gram negative cocci may be difficult. For these reasons, a general recommendation is to keep patients with presumed community acquired bacterial meningitis in droplet precautions for at least the first 24h of therapy and until the etiology has been determined.
Although appropriate empiric antibiotics to cover the usual organisms implicated in community acquired bacterial meningitis were initiated, all adult patients with suspected or confirmed bacterial meningitis by lumbar puncture should also be treated with IV dexamethasone prior to or at the time of their first dose of antibiotics [1]. In our case, this patient should have be started on the standard dose of dexamethasone at 10 mg IV q6h, 15 min prior to initiation of his antibiotics to complete a 4 day course [1, 5]. The efficacy of steroids in bacterial meningitis is discussed further in the management section of this chapter.
It is critical to initiate empiric antibiotics promptly and without delay while awaiting CSF gram stain results or imaging of the brain. In this case, the patient did meet criteria for imaging prior to LP due to altered level of consciousness, (see below), still empiric antibiotics were given promptly. Initially, during selection of the antibiotics it is important to assume a high likelihood of antimicrobial resistance and select broad coverage. In this case, our patient’s empiric antibiotics included vancomycin and ceftriaxone to cover for the most common pathogens, Streptococcus pneumoniae and Neisseria meningitides. Because this patient was over age 50 years, ampicillin was also appropriately added to cover for Listeria monocytogenes.
Although the gram positive diplococci were seen on gram stain, suggestive of Streptococcus pneumoniae, the patient was continued on the recommended empiric antibiotics vancomycin 15 mg/kg IV q8h (15–20 ug/mL trough target) and ceftriaxone 2 g IV q12h until definitive culture results and sensitivities are available. See Fig. 36.1.
Our patient was also started on anti-epileptic therapy and had no additional seizure activity. Over the next few days the CSF cultures grew pansensitive Streptococcus pneumoniae and the patient was continued on ceftriaxone for a 14 day course. By the third day the patient was alert and able to follow commands and was extubated. Seizure medications were discontinued and no further seizures occurred.
Principles of Management
Early recognition and treatment is critical to survival from bacterial meningitis. The host inflammatory response to this infection can be devastating. Several host and pathogen related factors ultimately lead to this condition. Virulence factors allow bacteria to colonize host epithelium with seeding of the bloodstream, crossing of the blood brain barrier and subsequent multiplication in the CSF due to the relative paucity of humoral immunity in the CSF. This cascade of events can lead to both systemic and neurologic complications. Here we will discuss the basic epidemiology, diagnosis, and treatment of community acquired bacterial meningitis.
Epidemiology
In recent decades there has been a shift in the pathogens responsible for bacterial meningitis. With the development and standardization of childhood vaccines against H. influenza type b (Hib) in 1985, pneumococcal vaccines (pneumococcal conjugate vaccine [PCV13] and pneumococcal polysaccharide vaccine [PPSV23]) in 2000 and meningococcal conjugate vaccine (MCV4) in 2005 the burden of bacterial meningitis has shifted to predominately older populations [6, 7]. Despite vaccines, Streptococcus pneumoniae and Neisseria meningitidis still account for over 80 % of bacterial meningitis cases [7, 8]. Less common pathogens, Group B Streptococcus (GBS), Haemophilus influenzae Listeria monocytogenes make up the remaining approximately 17 % of cases [7]. Patients’ ages 16–50 are at greatest risk for Neisseria meningitidis or Streptococcus pneumoniae, however, patients over the age of 50 or immunocompromised patients have an increased risk for Listeria monocytogenes, GBS, and aerobic gram negative bacilli [7, 8].
Diagnosis
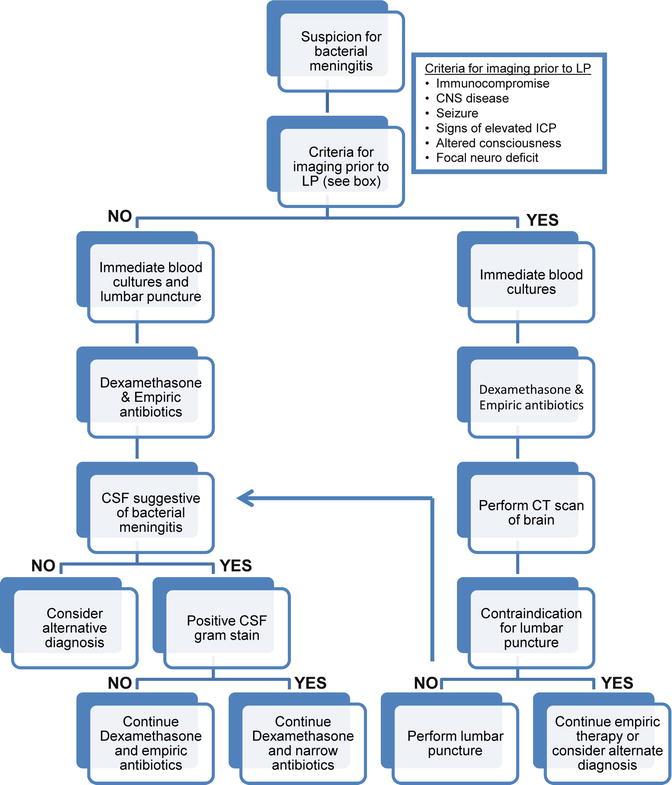
All patients with suspected bacterial meningitis should receive an LP unless contraindicated. See Fig. 36.2 for a management algorithm in all patients with suspected bacterial meningitis. Relative contraindications include elevated intracranial pressure, thrombocytopenia/bleeding diathesis or spinal epidural abscess [10]. If collection of CSF is delayed for imaging or other reasons, blood cultures should be collected prior to antimicrobial administration but antibiotics should not be delayed. Positivity of blood cultures for bacterial meningitis range from 50 to 90 % [1].
CSF results consistent with the diagnosis of bacterial meningitis include (1) elevated opening pressure (normal 20cmH2O), (2) pleocytosis of 1000 to 5000 μL with a >80 % neutrophil predominance, (3) glucose below 40 mg/dL (in adults glucose ratio CSF: serum ≤0.4), (4) mildly elevated protein level 100–500 mg/dL and (5) cloudy or turbid appearance.
Sensitivity for a positive gram stain ranges from 60 to 90 % with a >97 % specificity; greater likelihood of positive gram stains are seen in streptococcus pneumoniae, H. flu and Neisseria as opposed to gram negative bacilli [11]. See Table 36.1. CSF cultures identify an organism 70 to 85 % of the time [13]. Serum and urine bacterial antigens are not routinely helpful.
Gram stain appearance | Specific pathogen |
|---|---|
Gram positive diplococci ‘lancet-shaped’ | Streptococcus pneumoniae |
Gram positive cocci in clusters or tetrads | Staphylococcus aureus |
Gram positive cocci | Streptococcus agalactiae |
Gram positive rods | Listeria monocytogenes |
Gram negative diplococci | Neisseria meningitidis |
Pleomorphic gram negative rods (cocco-bacilli) | Haemophilus influenzae |
Gram negative rods | E. Coli or other Enterobacteriaceae |
Gram negative rods (bacilli) | Pseudomonas aeruginosa |
Notably, a traumatic tap, intracerebral or subarachnoid hemorrhage or recent seizure can all result in a falsely elevated WBC in the CSF. To correct WBC for a traumatic tap, subtract 1 WBC for every 500 to 1500 red blood cells (RBCs) in CSF to give the ‘Adjusted CSF WBC’ [14].
Select patients may be at risk for undergoing an LP and should receive imaging prior to LP. Antibiotic administration, however, should not be delayed [15]. See Fig. 36.2.
Repeat LPs are not indicated in patients with bacterial meningitis unless there has been no clinical improvement after 48 h of appropriate antibiotics. This is especially important if there is concern for pneumococcal meningitis with penicillin or cephalosporin resistance or when the patient has been treated with dexamethasone [1].
Antibiotics
A delay in administration of antibiotics of greater than 3 h from admission in bacterial meningitis has been associated with increased morbidity and mortality. Antibiotics should target the presumed pathogen identified by gram stain, or empirically started if the LP is delayed [1]. Antibiotics should be bactericidal and cross the blood brain barrier [16].
Empiric antibiotics for adults are vancomycin and a third generation cephalosporin (ceftriaxone or cefotaxime). In patients with risk factors for listeria (>50 years old, immunocompromised or alcoholism) the addition of ampicillin or penicillin G should be included. If there is a beta-lactam allergy: Vancomycin and moxifloxacin are considered empiric coverage with trimethoprim-sulfamethoxazole added for listeria. Consider the use of a fourth generation cephalosporin such as cefepime or a carbapenem such as meropenem in severely immunocompromised patients to cover for additional gram negative pathogens.
The duration of antibiotic therapy is usually from 7 to 14 days but should be guided by the specific pathogen identified, disease severity and antimicrobial agent selected [9, 17, 18] See Table 36.2.
Specific pathogen | Antibiotics | Duration |
|---|---|---|
Strep pneumoniae | ||
PCN | ||
MIC < 0.06 mcg/mL | Penicillin G (monotherapy) | 10–14 days |
MIC ≥ 0.12a | 3rd generation cephalosporinb | |
If Ceftriaxone MIC > 1 mcg/mL | Add Vancomycin | |
Neisseria meningitidis | 3rd generation cephalosporinb | 7 days
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|