Patricia Polgar-Bailey Asthma is a chronic inflammatory disorder of the airways characterized by increased responsiveness of the tracheobronchial tree to various stimuli, resulting in episodic reversible narrowing and inflammation of the airways.1,2 In susceptible individuals, this bronchial inflammation causes recurrent episodes of wheezing, shortness of breath, chest tightness, and cough. These episodes are usually associated with widespread but variable airflow obstruction that is often reversible, either spontaneously or with treatment. The inflammation also causes an associated increase in the existing bronchial hyperresponsiveness to a variety of stimuli.1,2 Asthma attacks can vary from mild to life-threatening and can be triggered by many factors, including allergens, infections, exercise, abrupt changes in weather, and exposure to airway irritants such as tobacco smoke.2 The concept of asthma as a chronic and inflammatory process represented a significant change in the previous understanding of the disease. During the past decade there have been substantial advances in the understanding of the genetics, pathogenesis, and natural course of the disease, which have had important implications for its management, particularly the development of new, targeted therapies, especially for severe asthma.1 Asthma is the most common chronic respiratory disorder among all age groups and affects 5% to 16% of people worldwide.3 Although the global prevalence of asthma increased markedly during the latter half of the of the 20th century, it appears to have plateaued since then, especially in countries with the highest asthma rates such as the United Kingdom.1 An exception to this is the United States, where the prevalence of asthma increased from 7.3% (20.3 million persons) in 2001 to 8.2% (24.6 million persons) in 2009, a 12.3% increase. Prevalence among children (persons aged <18 years) was 9.6% and was highest among poor children (13.5%) and among non-Hispanic black children (17.0%). Prevalence among adults was 7.7% and was greatest in women (9.7%) and in adults who were poor (10.6%). Looking at subgroups, a rising trend in asthma prevalence was observed for non-Hispanic black children (11.4% to 17.0%), non-Hispanic white women (8.9% to 10.1%), and non-Hispanic black men (4.7% to 6.4%).4 In 2009, asthma prevalence was greater among children than adults (9.6% versus 7.7%) and was especially high among boys (11.3%) and non-Hispanic black children (17.0%). Prevalence among adults was greatest for women (9.7%) and adults who were poor (10.6%).4 These statistics, as striking as they are, may still underestimate the actual prevalence of asthma, especially in communities where access to care, including emergency care, is limited.5 Among racial groups, persons of multiple race had the highest asthma prevalence (14.1%), whereas Asian persons had the lowest rates (5.2%). Persons of black (11.2%) and American Indian or Alaska Native (9.4%) races had higher asthma prevalence compared with white persons (7.7%). Among Hispanic groups, asthma prevalence was higher among persons of Puerto Rican (16.1%) than Mexican (5.4%) descent.6 Asthma attack prevalence refers to the number of people who had at least one asthma attack during the previous year; it is a crude indicator of how many people have uncontrolled asthma or are at risk for a poor outcome, such as hospitalization.6 In 2008, at least half (52.6%) of those diagnosed with asthma reported having an asthma attack within the past year.7 Asthma attack prevalence decreases with age; a greater proportion of children than adults (57.2% versus 50.7%) were reported to have had an asthma attack within the preceding 12 months. Women have a 35% higher asthma attack prevalence than men, but this pattern is reversed among children, in whom the attack prevalence for boys was 45% higher than the rate for girls.6 A greater proportion of persons who had an asthma attack reported being in fair or poor health (24.8%) than of those who did not have an asthma attack (17.9%).7 Asthma interferes with daily activities, including attending school and going to work. In 2008, on average, children missed 4 days of school and adults missed 5 days of work because of asthma, 26% reported emergency department (ED) or urgent care center visits, and 7% reported having been admitted to a hospital.7,8 Occupational asthma is currently the most common occupational ailment. Widespread exposure in the workplace environment to airborne dusts, gases, vapors, or fumes contributes to both the development of asthma and the worsening of asthma for those already affected. An estimated 1.9 million cases of asthma among adults were work related, accounting for 15.7% of current adult asthma cases. Work-related asthma significantly differs by age; the incidence is highest among persons aged 45 to 64 years (20.7%).8 Asthma accounts for 10.1 million lost work days annually and a total annual economic cost of $19.7 billion—$14.7 billion in direct costs, and another $5 billion in lost productivity.8 Asthma is one of the most common reasons for visits in ambulatory settings; in 2010 there were 14.2 million office visits with asthma as the primary diagnosis.9 Asthma is still responsible for a disproportionate and increasing number of ED visits (1.8 million) and hospitalizations (0.5 million).7 The type of medical setting in which persons receive health care for asthma differs for those with private health insurance and those without health insurance. From 2001 to 2009, health care visits for asthma per 100 persons with asthma declined in primary care settings, whereas asthma ED visit and hospitalization rates were stable. For the period of 2007 to 2009, black persons had higher rates for asthma ED visits and hospitalizations per 100 persons with asthma than white persons, and a higher asthma death rate per 1000 persons with asthma. Compared with adults, children had higher rates for asthma primary care and ED visits, similar hospitalization rates, and lower death rates. Asthma is a condition that can be treated effectively in primary care, resulting in fewer ED visits, improved continuity of care, and decreased health care costs based on Centers for Disease Control and Prevention (CDC) 2012 health statistics for U.S. adults.9 Although the asthma prevalence is higher among children, asthma deaths in children are relatively rare.10 Women have an asthma death rate higher than that of men.6 High mortality rates are associated with high rates of hospitalization in impoverished urban areas. Most of those hospitalized or seen in the ED had been there before, reflecting the fact that inadequate health care results in increased costs.10,11 Asthma hospitalization rates have been highest among African Americans, women, and children; likewise, death rates have consistently been disproportionately higher among African Americans, especially those aged 15 to 24 years.6 Although prevalence is higher among racial and ethnic minorities, a more valid relationship may exist between socioeconomic status and increased asthma prevalence, morbidity, and mortality than between race and asthma prevalence. Asthma mortality has also been associated with poverty, urban living conditions, exposure to oxidant pollutants, and passive smoking.7 Allergic asthmatic children exposed to high levels of indoor allergens, such as those associated with cockroaches, rodents, and mold, have more severe and more frequent episodes of asthma.11 The financial impact of asthma is considerable. At least 1% of all U.S. health care costs are spent on asthma—an estimated $3300 per person with asthma annually.8 Direct and indirect asthma-related costs are estimated to be $56 billion per year, with ED visits and hospitalizations responsible for the majority of the cost. Worldwide, an estimated 300 million people are affected by asthma, and the prevalence of asthma ranges from 1% to 18% of the population, depending on the country.2 It is estimated that the number of people with asthma will grow by more than 100 million by 2025.8 Workplace conditions, such as exposure to fumes, gases, or dust, are responsible for 11% of asthma cases worldwide. Prevalence rates vary widely depending on the country, which reflects a true difference in prevalence as well as different diagnostic standards. The prevalence has been increasing in low- and middle-income countries and plateauing in high-income countries.. Deaths from asthma worldwide have been estimated at 250,000 per year, but mortality does not appear to correlate well with prevalence.12,13 Although the cost to control asthma on a global scale is high, the cost of not treating asthma is even higher. It is now believed that the primary event in asthma is airway inflammation and that airway hyperresponsiveness and airflow obstruction are secondary and symptomatic features of the disease. Underlying airway inflammation (which involves cellular infiltration, edema, nerve irritation, and vasodilation) results in constriction of airway smooth muscle, increased production of mucus, and airway hyperresponsiveness. The airflow limitation associated with asthma is caused by a variety of changes in the airway, all of which are influenced by airway inflammation. These changes include bronchoconstriction (bronchial smooth muscle contraction that quickly narrows the airways in response to a variety of stimuli, including allergens and irritants), airway hyperresponsiveness (an exaggerated bronchoconstrictor response to stimuli), and airway edema (hypersecretion of mucus and mucous plugs as the disease becomes more persistent, which further limit flow).12 With time, remodeling of airways may occur, and reversibility of airway obstruction may be incomplete in some persons. Possible changes in airway structure include sub-basement fibrosis, hypersecretion of mucus, epithelial cell injury, smooth muscle hypertrophy, and angiogenesis (the growth of new blood vessels from existing blood vessels).12 The development of asthma appears to involve an interplay among host factors, particularly genetics, and environmental factors that occur at a crucial time in the development of the immune system, although a definitive cause of the inflammatory process has not been established.12 Different immune responses influence the development of asthma, including the Th1-type and Th2-type cytokine responses. Numerous factors affect the balance between these responses early in life and increase the likelihood that the Th1 immune response—which fights infection—will be downregulated and that the Th2 immune response—which contributes to the development of allergic diseases and asthma—will dominate. This is known as the hygiene hypothesis, which postulates that early in life, exposure to other children (e.g., presence of older siblings and early enrollment in childcare, which increase the likelihood of exposure to respiratory infection), less frequent use of antibiotics, and “country living” are associated with a Th1 response and a lower incidence of asthma, whereas the absence of these factors is associated with a persistent Th2 response and higher rates of asthma.12 Asthma also has an inheritable component, but the genetic factors involved remain complex.12 One factor involved is atopy, which is the genetic tendency for development of immunoglobulin E (IgE)–mediated hypersensitivity reactions in response to environmental antigens and allergens; it is considered one of the strongest predisposing factors for the development of asthma. Certain stimuli induce asthma by causing or increasing airway inflammation, whereas other stimuli provoke bronchoconstriction in individuals who already have asthma or airway hyperresponsiveness. Inducers, stimuli that are known to increase inflammation, include inhaled allergens, low-molecular-weight sensitizers, viral or mycoplasmal respiratory infections, and high concentrations of noxious gases. Stimuli that trigger or cause bronchoconstriction include exercise, cold air, laughter, emotional upset, and inhaled irritants. Triggers of sudden severe bronchoconstriction include acetylsalicylic acid or nonsteroidal anti-inflammatory drugs (NSAIDs), beta-adrenergic blockers, food allergens, certain food additives, stings, bites, injections (e.g., allergy shots), and inhaled allergens. These stimuli set the stage for a cascade of cellular activation, which includes subsequent cytokine release and neurologic excitation. The antigenic response is limited by certain cellular processes such as mast cell activation through cytokines and infiltration by inflammatory cells, including neutrophils, eosinophils, and lymphocytes. The inflammatory cells are also the source of mediators that induce bronchoconstriction, excess production of mucus, airway edema, and further influx of inflammatory cells, all of which lead to bronchial obstruction. The late-phase reaction, which generally occurs 3 to 8 hours after antigen exposure, is the result of new cellular infiltration and activation. Nocturnal and early morning bronchospasm, which occurs with relative frequency in persons with asthma, may be related to circadian variations in cortisol and epinephrine levels, vagal tone, and inflammatory mediators. One common, often overlooked, exacerbating factor of asthma is esophageal reflux of gastric contents. The incidence of gastroesophageal reflux in adults with asthma has been reported to range from 15% to 82% by pH monitoring.13 Gastroesophageal reflux resulting in distal esophageal stimulation with acid may cause bronchoconstriction or may increase bronchial reactivity through vagal mechanisms. Although the potential mechanism exists for gastroesophageal reflux disease (GERD) to cause asthma symptoms, and it is fairly well accepted that GERD may be an exacerbating factor, particularly in difficult-to-control asthma, it remains unclear whether there is a true causal relationship between reflux episodes and asthma symptoms. A study involving the largest group of patients with difficult-to-control asthma to date found that the identification and treatment of GERD failed to improve asthma outcome in the group as a whole. However, this study did not exclude the possibility that antireflux therapy does contribute to asthma control in persons with well-controlled asthma.13 In addition to the aforementioned factors, environmental factors appear to play a role in the development of asthma, although the nature of specific environmental contributions is not clearly defined. Exposure in utero to tobacco smoke is associated with an increased risk of wheezing, but it is not clear whether this is linked to subsequent development of asthma.12 Air pollution (ozone and particular matter) and diet (obesity or low intake of omega-3 fatty acids) have been associated with asthma, although the contribution of these factors to the development of asthma has not been clearly defined. As mentioned, asthma has a strong genetic component. However, for this to manifest, interaction with environmental factors must occur. At least some of the difference in asthma prevalence between white and minority populations may be a result of differences in genetic susceptibility. Most of the evidence to date suggests that the explanation for these differences is most likely the disparity in socioeconomic, environmental, behavioral, and cultural factors and in access to routine health care.14 Asthma is a disease that varies within and among individuals, but inflammation of the airways is a persistent feature, even in persons with mild asthma. Although asthma is considered to be a disease of reversible airflow obstruction, chronic airway inflammation can lead to progressive airway remodeling and airflow obstruction, eventually resulting in an irreversible deterioration of airway function.1 At present, asthma has no cure, but effective management can reduce its impact on quality of life and morbidity. The clinical hallmarks of asthma include episodic wheezing associated with dyspnea, cough, and sputum production. Between episodes, symptoms may improve or completely resolve. Symptoms vary from mild to severe, with varying effects on activity. An increased index of suspicion for asthma is essential when respiratory symptoms, including cough, wheeze, shortness of breath, chest tightness, and soreness, persist or recur often. Although wheezing is probably the symptom most typically associated with asthma, the most common symptom of asthma and often the most troublesome is cough. However, cough is also the third most common presenting symptom in the ambulatory setting, with a corresponding long list of potential causes. Coughing is the only asthma symptom 7% to 57% of the time; this type of asthma is referred to as cough-variant asthma. Cough can be the principal or only manifestation of asthma, especially in young children.12 Cough is often treated symptomatically, which can easily result in a delayed or missed diagnosis of asthma. Asthma should be considered in the differential diagnosis of all patients with a cough because it is such a common cause. Most persons with a cough do not have associated variable airflow obstruction; if obstruction is present and reversible with bronchodilator medication, the diagnosis of asthma is confirmed.15 In addition to chronic cough, asthma has several common clinical presentations. An acute asthmatic episode is characterized by airway obstruction, manifesting with symptoms of breathlessness and anxiety and often accompanied by wheezing and sometimes coughing. These symptoms may resolve within several hours if treatment is given or within 1 to 3 days even without specific intervention, or they may progress to more severe airway obstruction and respiratory compromise if no therapy is provided. Between acute asthmatic episodes, airflow is normal and symptoms are absent. Several specific conditions are associated with acute asthma exacerbations. Exercise-induced asthma refers to the development of airway obstruction in an individual after the cessation of exercise, even after brief periods of exercise. Symptoms usually begin 5 to 10 minutes after the completion of exercise and resolve within 1 to 4 hours. Certain forms of exercise, including skiing, ice hockey, and running in the cold, more commonly precipitate airway obstruction; other forms of exercise, such as swimming, less commonly precipitate airway obstruction, probably because of the warmer and more humid air being inspired. Cold or dry air often predisposes an asthmatic individual to airway obstruction, such as occurs when a person enters a dry, air-conditioned environment (such as an indoor mall) from the warmer, more humid outside air. Common allergens that precipitate asthma include cat allergen (dander), house dust mite allergen, cockroach allergen, and tree and grass pollen. Viral illnesses can also induce airway obstruction in asthmatic individuals; symptoms may persist for weeks to months if therapy is not initiated. Occupational exposures are common asthma triggers. Early responses may occur within several hours; however, late responses may not occur for 8 to 12 hours after exposure. Often, occupation-induced asthma symptoms may persist long after the individual has left the workplace, an important consideration in the differential diagnosis. Approximately 1% to 10% of individuals with moderate to severe asthma have aspirin exacerbated respiratory disease (AERD) (aspirin-induced asthma), which is characterized by symptoms of moderately severe airway obstruction, rhinorrhea, sneezing, tearing, dermal changes, and in some cases gastrointestinal symptoms (nausea, vomiting, cramping) on exposure to aspirin or other prostaglandin (H synthase type 1) inhibitors. The onset of AERD occurs most often when patients are in their 20s and 30s.16 The diagnosis of aspirin-induced asthma is important for two reasons: aspirin-containing drugs should be avoided because these drugs may induce life-threatening asthma attacks, and effective treatment is available specifically for this type of asthma. In trials in which patients with AERD were challenged with selective NSAIDs, there was a small risk of respiratory symptoms with selective NSAIDs. However, cyclooxygenase 2 (COX-2) inhibitors with etoricoxib did not appear to exacerbate airway inflammatory or obstruction in persons with AERD.16 Acute severe asthma, although it is not pathologically distinct from acute asthma, represents a more severe and prolonged form of the illness. Acute severe asthma is often characterized by unremitting asthma symptoms (including shortness of breath, diminished exercise tolerance, and wheezing) for weeks with less-than-optimum response to therapy. Often, asthmatic individuals develop prolonged severe asthma by inappropriately self-medicating with beta2-adrenergic agonist inhalers for weeks before seeking medical attention, at which point the risk of respiratory collapse and asphyxia may be great.15 Chronic stable asthma refers to asthma that is characterized by episodes of airway obstruction and airway symptoms. Although multiple asthma episodes may occur during a period of several months, most are of moderate severity and respond promptly to therapy. The two most important aspects of asthma therapy are pharmacologic therapy and environmental control. For severe asthma, treatment of comorbidities is also essential to achieve control, but may complicate asthma management.1,2 The National Asthma Education and Prevention Program (NAEPP) of the National Institutes of Health (NIH) developed sample questions for the diagnosis and initial assessment of asthma (Box 103-1).12 In addition to an assessment of symptoms, an individual’s family history is helpful when a diagnosis of asthma is being considered. Persons with asthma often have a family history of asthma or atopy. Also, family members are often able to identify specific exposures or circumstances that precipitate the patient’s symptoms. Sample questions for the follow-up assessment of patients with previously diagnosed asthma are listed in Box 103-2. Asthma can be classified according to the frequency and severity of symptoms and the pattern of airflow limitation or according to the treatment steps necessary to decrease symptoms, to improve lung function, and to prevent exacerbations to allow normal daily activities (Table 103-1). Asthma can have a variable course, and the degree of asthma control and the severity of asthma within an individual can change over time. Providers need to be aware of the difference between asthma control and severity. For example, severe asthma can be well controlled, that is, few exacerbations with intensive pharmacotherapy and good self-management. On the other hand, an individual with mild asthma and little need of intensive treatment may still have periods of poor control. Persons with well-controlled asthma are still vulnerable to acute exacerbations, especially if they are exposed to factors that precipitate their asthma symptoms. TABLE 103-1 Severity of Asthma Exacerbations There is increasing evidence that persons affected by problems of socioeconomic deprivation and psychosocial issues such as anxiety, depression, and stress are at increased risk for asthma exacerbations.17 A study by Sandberg and colleagues18 demonstrated that even in children with asthma, psychosocial stress can worsen asthma control and increase the risk of an acute exacerbation. The physical examination of the patient with asthma or suspected asthma can be divided into four objectives: (1) diagnosis and differential diagnosis, (2) assessment of asthma severity, (3) identification of adverse effects of medications, and (4) identification of concomitant medical problems. A complete physical examination is necessary if assessment of respiratory exertion or compromise is needed, coexisting medical conditions must be identified or evaluated, or the presentation is complex. The diagnosis of asthma is based on the history, physical examination, and certain diagnostic tests, particularly spirometry. The physical examination, although an essential part of the evaluation, may correlate poorly with objective measures of airway obstruction, such as pulmonary function tests (PFTs). In the asymptomatic patient, the physical examination findings may be entirely normal. Nonetheless, assessment of the severity of asthma and airway obstruction is the most important objective in evaluating a person with asthma. Wheezing may be detectable or elicited during forced expiration. In general, mild bronchospasm is associated with expiratory wheezing. As obstruction becomes more significant, wheezing is heard during both the inspiratory and expiratory phases, with a prolongation of the latter. With profound obstruction, wheezing may be heard only during the inspiratory phase or may be entirely absent. With severe obstruction, the intensity of the breath sounds diminishes. As obstruction increases, accessory muscles of respiration are used; with significant obstruction, there may be evidence of hyperinflation with a low diaphragm and an increased anteroposterior diameter. Severe asthma exacerbations are characterized by labored respirations, diaphoresis, anxiety, and breathlessness (inability to finish a complete sentence). A respiratory rate of 30 breaths per minute or more and a heart rate of 120 beats per minute or more suggest severe bronchospasm. Other signs and symptoms that often herald impending respiratory failure include agitation, confusion, somnolence, and cyanosis. Unilateral loss of breath sounds may reflect mucous plugging and secondary atelectasis, but pneumothorax must also be considered in this situation. However, even a careful physical examination provides only a crude estimate of airway obstruction, and significant airway obstruction is possible even when the physical examination findings are entirely normal. Assessment of respiratory status is best accomplished through measurement of lung function with spirometry or peak flow meters. The Global Initiative for Asthma (GINA) system of classifying the severity of asthma exacerbations is presented in Table 103-1. The physical examination is also important in identifying adverse effects of asthma medications. Side effects of beta2-adrenergic medications and theophylline include tachycardia and tremors. Inhaled corticosteroids (ICSs) can cause oral thrush and dysphonia. Adverse effects of oral (systemic) corticosteroids include central adiposity, hypertension, ecchymoses, cataracts, kyphosis, muscle weakness, and alterations in mental status. Coexisting medical problems can be conceptualized in two ways. Certain comorbid conditions, such as nasal polyps, allergic rhinitis, sinusitis, and eczema, are commonly associated with asthma. In addition, some coexisting medical problems may be unrelated to asthma, but their identification and management have important implications for asthma therapy and control. Such possible comorbidities include glaucoma, hypertension, gastroesophageal reflux, diabetes mellitus, arthritis, and current malignant neoplasms. A diagnosis of asthma is based on three components: (1) demonstration of episodic symptoms of airflow obstruction (e.g., wheeze, cough, shortness of breath), (2) evidence that airflow obstruction is at least partially reversible, and (3) exclusion of other conditions from the differential diagnosis.12 A thorough history and physical examination are essential to making the diagnosis of asthma. Physical findings can be helpful in identifying significant obstruction as it occurs but at best provide only a crude estimate of the degree of obstruction. However, significant obstruction may not manifest as an abnormal physical finding; in addition, findings are likely to be completely normal between episodes. In fact, reduced expiratory flow rates (forced expiratory volume at 1 second [FEV1]) and increased airway resistance may not be recognized as dyspnea until a 30% to 40% decline in FEV1 has occurred.19 Thus, objective measures of pulmonary function, such as spirometry and peak flow meters, are essential in establishing the diagnosis of asthma and assessing its severity. Spirometry is now recommended at the time of initial assessment to confirm the diagnosis of asthma, after treatment is initiated and symptoms and peak expiratory flow (PEF) have been stabilized, and at least every 1 to 2 years.12 Although spirometry provides many measures, the most useful for evaluation of asthma are the peak expiratory flow rate (PEFR), FEV1, maximum mid-expiratory flow rate (MMEFR), and forced vital capacity (FVC). Results are compared with expected values, derived from a population of healthy, nonsmoking adults, and are expressed as a percentage of the expected value. The most common pulmonary function abnormality in mild asthma is the decreased rate of airflow throughout the vital capacity as reflected by abnormalities in the PEFR, FEV1, and MMEFR (forced expiratory flow [FEF25-75]). During bronchospasm, spirometry reveals obstruction with decreases in FEV1 and MMEFR. The FEV1/FVC ratio is also reduced. As obstruction increases, an increased residual volume and functional residual are noted. One of the diagnostic hallmarks of asthma is reversal of obstruction after the administration of a bronchodilator, which corresponds with both clinical improvement and improved spirometric values. In addition to helping establish the diagnosis of asthma, spirometry helps assess the adequacy of therapy, the need for further therapy and evaluation during emergencies, and the need for hospital admission. The severity of asthma attacks must be assessed by accurate and reproducible measures of airflow. Health care providers tend to underestimate the degree of airway obstruction in individuals with acute asthma, and knowledge of a person’s pulmonary function has potentially important implications for treatment. For this reason, the NAEPP guidelines recommend the use of PFTs as part of the assessment and monitoring during the treatment of acute asthma. During a severe asthma attack, recording of the entire spirogram may be difficult, but the FEV1 can still be measured. As the asthma attack resolves, both the PEFR and the FEV1 increase, whereas the MMEFR usually remains significantly diminished. Most patients with controlled asthma will not exhibit reversibility in FEV1 at each visit, particularly those who are being treated for asthma, and therefore the test lacks sensitivity. Repeated testing at different visits may be helpful.2 PEF measurements with use of a peak flow meter may also be helpful in the diagnosis and management of asthma, but measurements of PEF are not interchangeable with other measurements of lung function such as FEV1 because values obtained with different peak flow meters vary and the range of predicted values is too wide.2 In addition, PEF measurements are effort dependent and may not be an accurate reflection of a person’s pulmonary function. PEF measurements done in the office should always be compared with the patient’s previous “personal best” using his or her own peak flow meter. The terms reversibility and variability refer to changes in symptoms accompanied by changes in airflow limitation that occur spontaneously or in response to treatment. Reversibility refers to rapid improvements in FEV1 or PEF minutes after use of a quick-relief medication such as a bronchodilator or sustained improvement during days or weeks after the introduction of a long-term control medication such as an ICS.2 In contrast, variability refers to the change (improvement or deterioration) in asthma symptoms and lung function occurring during a longer time.12 Variability may be experienced in the course of a day (diurnal variability), from day to day, from month to month, or seasonally. Obtaining a history of variability is an integral aspect of asthma diagnosis and management. Other laboratory tests that may be used to diagnose asthma or be included as part of the evaluation are airway responsiveness testing, arterial blood and other serum analysis, radiography, electrocardiography (ECG), and sputum cultures. Airway responsiveness testing measures the bronchoconstrictor response elicited by a standard stimulus. The FEV1 is measured after inhalation of an aerosol containing graded amounts of a bronchoconstrictor agonist. The most commonly used bronchoconstrictor is methacholine, but histamine, exercise, eucapnic voluntary hyperventilation or inhaled mannitol can also be used for bronchial provocation. These tests are moderately sensitive for a diagnosis of asthma, but have limited sensitivity. For example, airway hyperresponsiveness to inhaled methacholine can also occur in patients with allergic rhinitis.2 Individuals with asthma often have atopy, which is often reflected in blood eosinophilia. Total serum IgE levels are elevated in persons with asthma and associated with disease severity, but IgE levels cannot predict response to treatment.20 The data from studies in pediatric populations unambiguously suggest a positive relationship between atopy and asthma severity, but studies in adults show an inconsistent relationship between the two.21 In general, the chest radiographs of individuals with asthma are normal. Therefore, chest radiography is not indicated in the routine evaluation of patients with asthma unless physical examination findings are suggestive of infectious illness or respiratory complications such as pneumomediastinum or pneumothorax. If an asthma exacerbation is severe enough to warrant hospital admission, a chest x-ray film should be taken. The x-ray film may show hyperinflation (indicated by diaphragmatic depression) and abnormally translucent lung fields. Between asthma attacks, in the absence of respiratory infection, the sputum is usually clear. During an asthma attack, even in the absence of infection, the sputum may be yellow to green. This does not necessarily indicate infection; the color change may be from eosinophil peroxidase. Sputum culture specimens are generally not obtained unless there is suspicion of an acute contagious respiratory infection. ECG is not part of the routine evaluation of a patient with asthma. If it is performed during an asthma exacerbation, ECG in the absence of cardiac disease is usually significant only for sinus tachycardia. In severe attacks, right-axis deviation, right bundle branch block, cor pulmonale, or even ST-T wave abnormalities may occur. If these abnormalities resolve as the asthma attack abates, no further cardiac evaluation is necessary. Electrocardiographic findings should be monitored during asthma attacks for patients with significant cardiac disease to monitor for myocardial infarction, which can result from attack-induced stress.
Asthma
Definition and Epidemiology
![]() Specialist referral is indicated for patients with SaO2 less than 90% on room air, peak flow less than 70%, and failure to improve with three nebulizer treatments or three epinephrine injections.
Specialist referral is indicated for patients with SaO2 less than 90% on room air, peak flow less than 70%, and failure to improve with three nebulizer treatments or three epinephrine injections.
Pathophysiology
Clinical Presentation
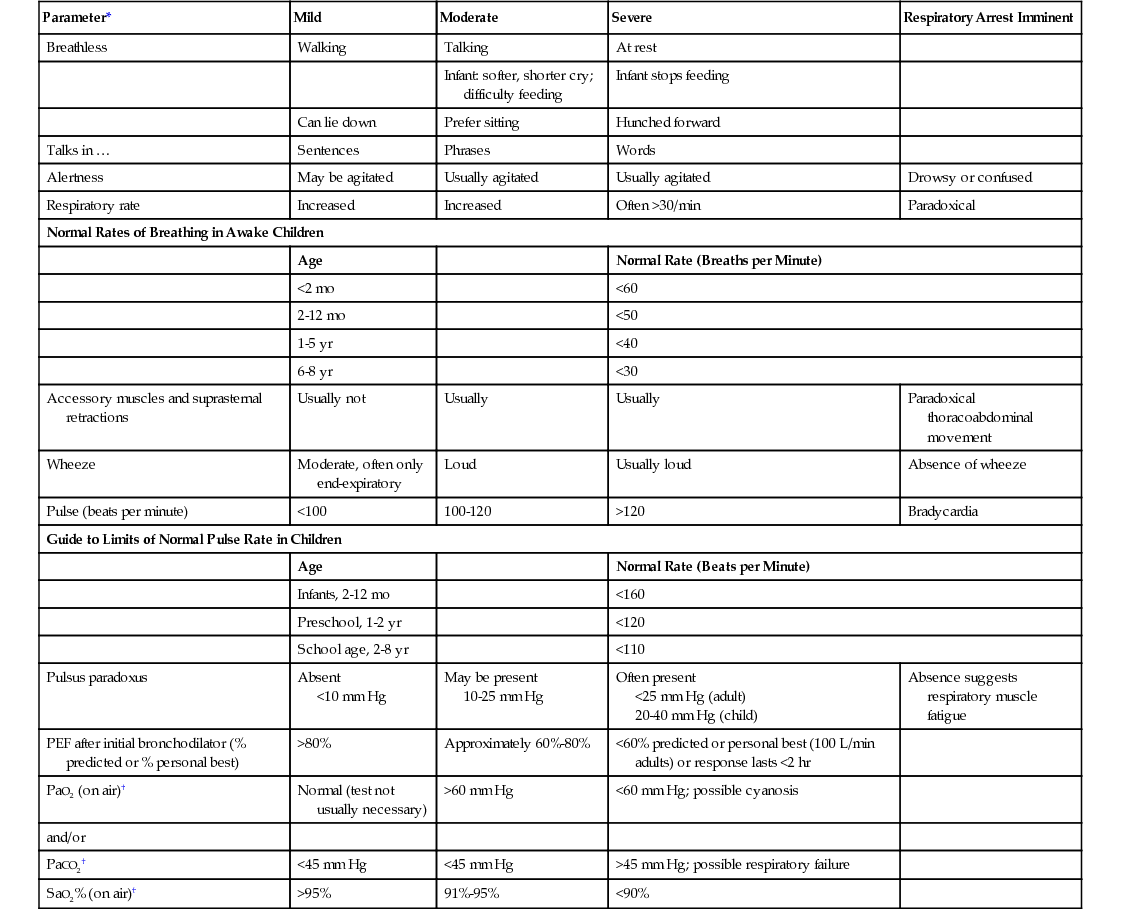
Parameter*
Mild
Moderate
Severe
Respiratory Arrest Imminent
Breathless
Walking
Talking
At rest
Infant: softer, shorter cry; difficulty feeding
Infant stops feeding
Can lie down
Prefer sitting
Hunched forward
Talks in …
Sentences
Phrases
Words
Alertness
May be agitated
Usually agitated
Usually agitated
Drowsy or confused
Respiratory rate
Increased
Increased
Often >30/min
Paradoxical
Normal Rates of Breathing in Awake Children
Age
Normal Rate (Breaths per Minute)
<2 mo
<60
2-12 mo
<50
1-5 yr
<40
6-8 yr
<30
Accessory muscles and suprasternal retractions
Usually not
Usually
Usually
Paradoxical thoracoabdominal movement
Wheeze
Moderate, often only end-expiratory
Loud
Usually loud
Absence of wheeze
Pulse (beats per minute)
<100
100-120
>120
Bradycardia
Guide to Limits of Normal Pulse Rate in Children
Age
Normal Rate (Beats per Minute)
Infants, 2-12 mo
<160
Preschool, 1-2 yr
<120
School age, 2-8 yr
<110
Pulsus paradoxus
Absent
<10 mm Hg
May be present
10-25 mm Hg
Often present
<25 mm Hg (adult)
20-40 mm Hg (child)
Absence suggests respiratory muscle fatigue
PEF after initial bronchodilator (% predicted or % personal best)
>80%
Approximately 60%-80%
<60% predicted or personal best (100 L/min adults) or response lasts <2 hr
PaO2 (on air)†
Normal (test not usually necessary)
>60 mm Hg
<60 mm Hg; possible cyanosis
and/or
PaCO2†
<45 mm Hg
<45 mm Hg
>45 mm Hg; possible respiratory failure
SaO2% (on air)†
>95%
91%-95%
<90%
Physical Examination
Diagnostics
Asthma
Chapter 103







