| Stanford classification | |
| Type A | Dissection involving the ascending aorta, as defined as proximal to the brachiocephalic artery, with or without involvement of the descending aorta |
| Type B | Dissection of the descending aorta alone, defined as distal to the left subclavian artery |
| DeBakey classification | |
| Type 1 | Dissection of the entire aorta |
| Type 2 | Dissection of the ascending aorta alone |
| Type 3 | Dissection of the descending aorta alone |
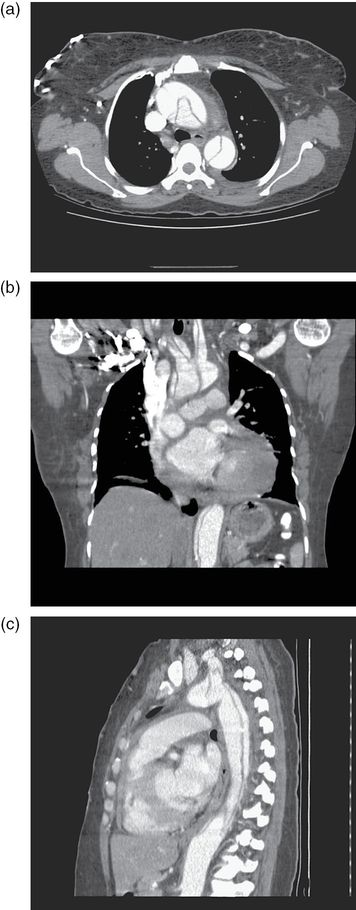
Figure 25.1. Aortic dissection diagnosed on CT angiography is visible in transverse (a), coronal (b) and sagittal (c) views. (Images courtesy of Amanda Holland Yang, MD.)
Critical management
- Place two large-bore IVs in preparation for potential massive resuscitation with fluids and blood products.
- Connect the patient to a monitor with continuous blood pressure monitoring and electrocardiogram.
- Obtain a 12-lead ECG to rule out cardiac ischemia or infarction.
- In the hemodynamically unstable patient with suspected acute aortic dissection, a transesophageal ultrasound is the confirmatory test of choice as it can be done at bedside and does not require for the patient to be taken out of the emergency department.
- Provide pain relief with opiates (morphine, fentanyl, or hydromorphone).
- Aggressive early blood pressure control serves as the critical intervention in acute dissection.
- The blood pressure should be dropped rapidly to a goal of 100–120 mmHg systolic, and the heart rate to 60–80 bpm.
- Beta-blockers are the initial agents of choice. They should be administered prior to vasodilators in order to prevent reflex tachycardia that may exacerbate shear forces.
- Labetalol: Bolus 10–20 mg IV, double the dose every 10 minutes to a maximum of 80 mg/dose, or start a continuous infusion starting at 2–10 mg/minute IV and increase by 1 mg/minute every 10 minutes until the desired blood pressure is achieved.
- Esmolol: Bolus 500 micrograms/kg IV followed by a continuous infusion starting at 25–300 micrograms/kg/minute. Titrate by 50 micrograms/kg/minute every 4 minutes.
- Labetalol: Bolus 10–20 mg IV, double the dose every 10 minutes to a maximum of 80 mg/dose, or start a continuous infusion starting at 2–10 mg/minute IV and increase by 1 mg/minute every 10 minutes until the desired blood pressure is achieved.
- Beta-blockers are the initial agents of choice. They should be administered prior to vasodilators in order to prevent reflex tachycardia that may exacerbate shear forces.
- If necessary, vasodilators can be added after initiation of the beta-blockers.
- Sodium nitroprusside: Start a continuous infusion at 1–4 micrograms/kg/minute and titrate by 0.25–0.5 microgram/kg/minute every 2–3 minutes.
- Glyceryl trinitrate: Start a continuous infusion at 10–200 micrograms/minute and titrate by 5–10 micrograms/minute every 5–10 minutes.
- Nicardipine: Start a continuous infusion at 2.5–15 mg/hour and titrate by 2.5 mg/hour every 5–10 minutes.
- Sodium nitroprusside: Start a continuous infusion at 1–4 micrograms/kg/minute and titrate by 0.25–0.5 microgram/kg/minute every 2–3 minutes.
- Monitor for signs of oliguria or neurological dysfunction.
- Early surgical consultation should be obtained for patients with Stanford type A dissections.
- Stanford type B dissections are frequently treated with medical therapy alone.
Sudden deterioration
- Sudden decompensation will most likely result from cardiovascular catastrophe.
- Maintain a low threshold for intubation and ventilation in cases of hemodynamic instability or neurological deficit leading to airway compromise.
- In cases of hypotensive shock, consider acute myocardial infarction, aortic rupture, and hemopericardium.
- Pericardiocentesis should be considered but only be aimed at removing enough pericardial fluid to raise the blood pressure to an acceptable level.
- In the presence of acute myocardial infarction or stroke, aortic dissection is a contraindication to thrombolytic therapy.
- Indications for surgical management of type B dissections include persistent pain, rapid expansion on serial imaging, evidence of organ or peripheral ischemia, or acute rupture.
- Active hemorrhagic stroke is a relative contraindication to surgery.
Critical care considerations
Vasopressor of choice: Patients with acute aortic dissection usually present with hypertension but can become hypotensive with progression of the condition. These patients will need to be aggressively resuscitated with blood products. Infusion of crystalloids and use of vasopressors such as phenylephrine and norepinephrine can be initiated as a temporizing measure.
References
Braverman AC. Aortic dissection: prompt diagnosis and emergency treatment are critical. Cleve Clin J Med. 2011; 78: 685–96.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






