INTRODUCTION AND EPIDEMIOLOGY
Given the mobility of the ankle joint and our bipedal existence, ankle injuries are a common complaint. They represent 14.6% of all visits to the ED.1 Fractures of the lateral malleolus are more prevalent in men younger than 50 years old and in women older than 50 years old.2,3 Previous ankle sprain and participation in sports like soccer, basketball, rugby, and football are risk factors for ankle injuries.4,5,6,7 A review of the National Electronic Injury Surveillance System in 2009 reported an incidence of ankle sprains of 206 per 100,000 people in the United States.8
ANATOMY
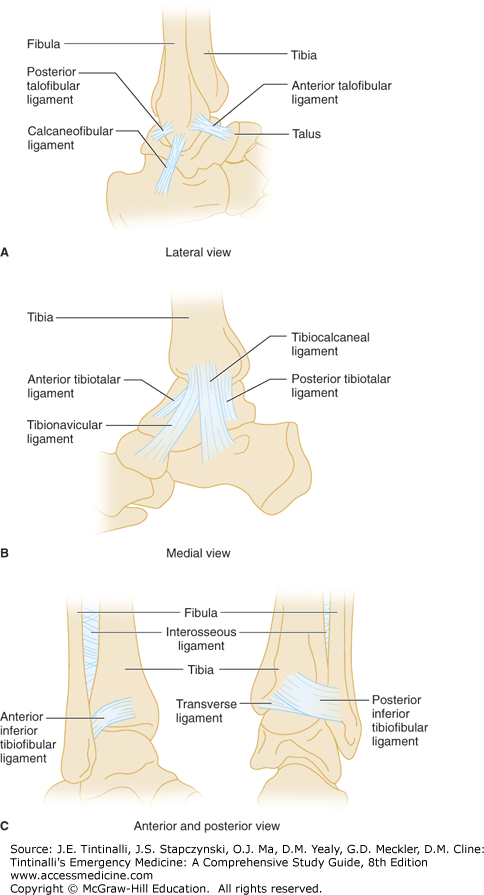
The proximal part of the ankle mortise is comprised of the distal fibula and tibia that fits on top of the talus. These bones are wider anteriorly than posteriorly. Joint stability is provided by medial and lateral malleoli extending on either side of the talus. The medial deltoid ligament, lateral ligament complex, and syndesmosis are the three distinct groups of ligaments that stabilize the ankle9 (Figure 276-1). The deltoid ligament is the strongest of these ligaments and is a thick, triangular band of tissue originating from the medial malleolus. The lateral ligament complex consists of the lateral malleolus that attaches to the anterior and posterior aspects of the talus and calcaneus by the anterior talofibular, posterior talofibular, and calcaneofibular ligaments, respectively. This ligament complex, the anterior talofibular ligament in particular, is the weakest and most commonly injured in lateral sprains and represents 85% of all ankle sprains.10 The syndesmosis, which holds the tibia and fibula together, is a group of four distinct ligaments attaching the distal tibia to the fibula just above the talus (Figure 276-1). The syndesmosis allows the fibula to rotate and carries approximately 16% of the axial load.9
FIGURE 276-1.
Ligaments of the ankle joint. A. The three lateral ligaments: the anterior and posterior talofibular ligaments and the calcaneofibular ligament. B. The four bands of the deltoid ligament: the anterior and posterior tibiotalar, the tibiocalcaneal, and the tibionavicular. C. Anterior and posterior view of the ankle syndesmosis. The ligaments of the syndesmosis are the anterior inferior tibiofibular ligament, the posterior inferior tibiofibular ligament, the transverse ligament, and the interosseous ligament, which connects the entire length of the tibia and fibula.
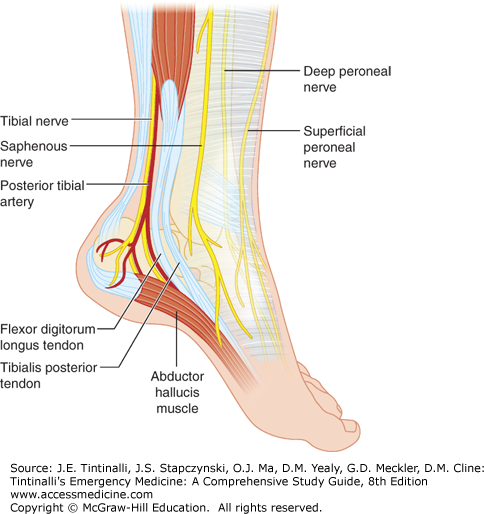
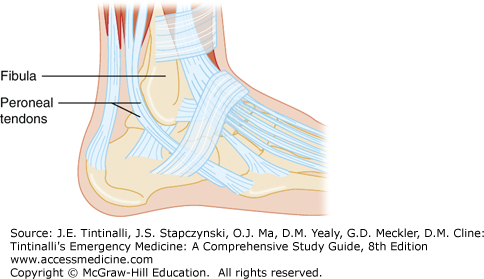
The ankle is considered a hinged joint, but ligamentous attachments allow for some rotation and translation within the mortise of the talar dome.9 Branches of the sciatic nerve, the superficial peroneal, deep peroneal, peroneal, and tibial, innervate the four muscle groups of the ankle joint with branches of the popliteal artery serving as the blood supply (Figure 276-2). The tibialis anterior, extensor digitorum longus, and extensor hallucis longus muscles run over the anterior aspect of the joint and are responsible for dorsiflexion. Inversion is accomplished by the tibialis posterior, flexor digitorum longus, and flexor hallucis longus. The peroneus longus and brevis muscles, sharing a common synovial sheath held in place by a groove on the posterior aspect of the lateral malleolus and superior retinaculum, run laterally to evert and plantarflex the joint. Plantarflexion is primarily accomplished by the gastrocnemius and soleus muscles.
CLINICAL FEATURES
Understanding the mechanism and timing of the injury is important. Document these details along with any previous bony or soft tissue injuries. Patients with signs of neurovascular compromise, including coldness and numbness of the foot, a rapid onset of swelling, extreme pain, and complicating conditions such as diabetes, require urgent evaluation.5 A normal-appearing ankle does not preclude the need for further inquiry. Due to the significant swelling typically present after acute injuries, examining the ankle is challenging but can be helped by elevation of the injured extremity and ice applied at triage. Peroneal spasms may mask any instability in the joint.9
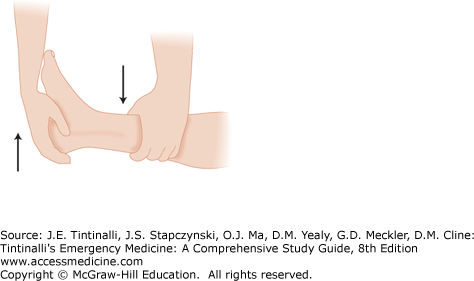
Place the patient on a stretcher to perform a thorough evaluation. A systemic approach to the examination decreases the chance of missed injuries. Starting with the skin and soft tissues, note any ecchymosis, abrasions, or swelling. Note the position, swelling, and skin integrity of the joint as well as any areas of tenderness or crepitus. Joints above and below the ankle need to be examined for any concomitant injuries. Suspect a Maisonneuve fracture (or fibulotibialis ligament tear) if there is tenderness of the fibular head or proximal fibular shaft. Palpate the area of obvious injury last. Test the functionality of the joint with both active and passive plantarflexion, dorsiflexion, and full range-of-motion exercises. Peroneal tendon injuries can occur from forced dorsiflexion, which presents as weakness on eversion (Figure 276-3). Check stability in external rotation, varus, and valgus. Palpate the posterior aspects of the lateral and medial malleoli, starting proximally to the joint and working distally. If there is a concern for isolated fibular fractures, check for evidence of injury to the syndesmosis or deltoid ligament.9 A positive anterior drawer test (Figure 276-4) is indicative of a torn anterior talofibular ligament. A positive anterior drawer test, swelling, and a hematoma are signs of a grade III sprain. Syndesmosis injuries can be deceiving because the patient describes ankle pain, but there is typically little ankle edema or ecchymosis. The crossed-leg test (compressing the fibula toward the tibia just above the midpoint of the calf11) can detect a syndesmosis injury and is indicated if pressure to the medial aspect of the knee elicits pain in the syndesmosis (Figure 276-5). The squeeze test is performed by squeezing the calf just above the ankle joint. Pain indicates syndesmosis injury. Calcaneofibular ligament instability can be detected with the inversion stress test or talar tilt.6 If the examination is uncomforTable for the patient, consider a hematoma block, sedation, or both to perform a more thorough examination.11
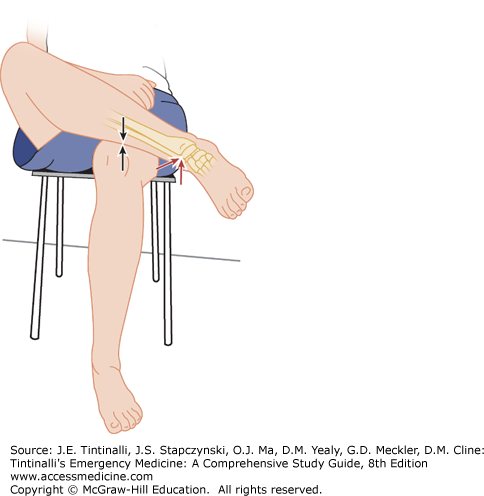
FIGURE 276-5.
The crossed-leg test. The affected leg is crossed over the opposite leg as demonstrated. If pain results at the arrow sites when pressure is applied to the medial side of the affected knee, the test is positive and indicates syndesmosis injury. [Copyright © 2010 by the American Orthopaedic Foot and Ankle Society, Inc., originally published in Foot & Ankle International in Kiter E, Bozkurt M: The crossed-leg test for examination of ankle syndemosis injuries. Foot Ankle Int 2: 187, 2005, and reproduced here with permission.]
Examine areas in close proximity to the ankle as well. What may be described as an ankle injury may end up being an injury to the Achilles tendon or foot and cannot be excluded by ankle radiographic imaging. Assess the integrity of the Achilles tendon. Fluoroquinolones and corticosteroids increase the risk of such an injury.12 Perform the Thompson test (see Figure 44-4 in chapter titled “Leg and Foot Lacerations”) if there is tenderness or a defect. Place the patient prone on the stretcher and squeeze the calf. Loss of plantarflexion indicates a complete Achilles tendon rupture. Palpate the hindfoot and midfoot over the calcaneus, tarsals, and base of the fifth metatarsal to check for areas of tenderness that may require further investigation.
Perform a neurovascular examination. Check dorsalis pedis and posterior tibial pulses and document digital capillary refill. Inability to dorsiflex the toes suggests a tibial nerve injury. Inability to plantarflex the great toe is suspicious for peroneal nerve injury.
If there are any significantly displaced fractures or dislocations, immobilize the joint in a neutral position with a well-padded splint to reduce further soft tissue injury. Follow this with elevation and application of ice to reduce edema. Emergently reduce any displaced fractures or dislocations with neurovascular compromise (see later treatment section under “Dislocations”).
DIAGNOSIS
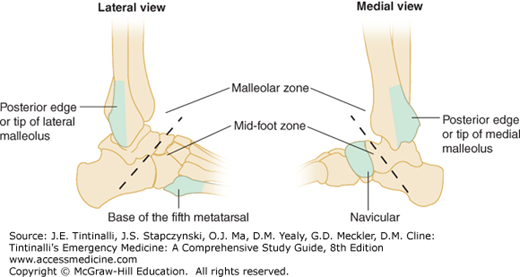
The Ottawa Ankle Rules for Ankle and Midfoot Injuries2,13,14,15,16,17 are easily applied by physicians and triage nurses.18,19 The rules are summarized in Figure 276-6.
The rules were originally developed for patients older than age 18 years who were able to cooperate, were not intoxicated, and had no distracting injuries or decreased sensation. Assuming the patient does not have any bony tenderness, assess the ability to bear weight by having the patient take four steps, resulting in two transfers to and from the injured ankle. The initial studies demonstrated a 30% reduction for the need of ankle radiographs.16,20
The standard ankle trauma series consists of three views: anteroposterior, 15-degree internal oblique, and lateral views. See Figure 276-7 for normal anatomy. About 95% of all ankle fractures can be detected with any two of these views.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree