![]() Dislocated Ankle Joint
Dislocated Ankle Joint
![]() Demonstrated on plain radiographs
Demonstrated on plain radiographs
![]() Clinically dislocated with neurovascular compromise
Clinically dislocated with neurovascular compromise
CONTRAINDICATIONS
![]() Open dislocations without neurovascular compromise may be better managed in the operating room for cleaning before reduction
Open dislocations without neurovascular compromise may be better managed in the operating room for cleaning before reduction
![]() After one or two unsuccessful attempts at reduction, orthopedic consultation should be considered
After one or two unsuccessful attempts at reduction, orthopedic consultation should be considered
RISK/CONSENT ISSUES
![]() Neurovascular damage may result from reduction attempt
Neurovascular damage may result from reduction attempt
![]() Closed reduction may be unsuccessful and operative repair may be required
Closed reduction may be unsuccessful and operative repair may be required
![]() Risks of intravenous (IV) analgesia/sedation
Risks of intravenous (IV) analgesia/sedation
![]() Risks of regional anesthesia
Risks of regional anesthesia
![]() General Basic Steps
General Basic Steps
![]() Patient preparation
Patient preparation
![]() Obtain radiographs
Obtain radiographs
![]() Analgesia/Sedation
Analgesia/Sedation
![]() Reduce joint
Reduce joint
![]() Check neurovascular status
Check neurovascular status
![]() Immobilize joint
Immobilize joint
![]() Postprocedure radiographs
Postprocedure radiographs
LANDMARKS
![]() The ankle joint is a modified saddle joint that comprises the distal fibula, tibia, and the talus bone of the foot
The ankle joint is a modified saddle joint that comprises the distal fibula, tibia, and the talus bone of the foot
![]() Is a stable joint with strong ligamentous support
Is a stable joint with strong ligamentous support
![]() Dislocations are a result of significant forces applied to the ankle and are often associated with fractures; isolated dislocations are uncommon
Dislocations are a result of significant forces applied to the ankle and are often associated with fractures; isolated dislocations are uncommon
TECHNIQUE
![]() Preprocedure Examination
Preprocedure Examination
![]() Search for other injuries, especially if high-energy mechanism
Search for other injuries, especially if high-energy mechanism
![]() Check neurovascular status of the foot
Check neurovascular status of the foot
![]() Get prereduction radiographs of dislocation (anteroposterior [AP], lateral, mortise views)
Get prereduction radiographs of dislocation (anteroposterior [AP], lateral, mortise views)
![]() If there is neurovascular compromise or tenting of the skin, perform immediate reduction before obtaining radiograph
If there is neurovascular compromise or tenting of the skin, perform immediate reduction before obtaining radiograph
![]() Try to ascertain the mechanism of injury
Try to ascertain the mechanism of injury
![]() Analgesia and Sedation
Analgesia and Sedation
![]() Procedural sedation
Procedural sedation
![]() Regional analgesia
Regional analgesia
![]() Bier block
Bier block
![]() Hematoma block
Hematoma block
![]() Procedure
Procedure
![]() Technique depends on type of dislocation but, in general, involves downward traction on heel while a force opposite to the direction of the dislocation is applied
Technique depends on type of dislocation but, in general, involves downward traction on heel while a force opposite to the direction of the dislocation is applied
![]() Flexion of the hip and knee to 90 degrees may aid reduction by relaxing the gastrocnemius–soleus complex
Flexion of the hip and knee to 90 degrees may aid reduction by relaxing the gastrocnemius–soleus complex
![]() If no assistant is available this can be accomplished by hanging the patient’s knee over the end of the bed
If no assistant is available this can be accomplished by hanging the patient’s knee over the end of the bed
LATERAL DISLOCATION (FIGURE 67.1)
![]() Most common ankle dislocation seen in the emergency department (ED)
Most common ankle dislocation seen in the emergency department (ED)
![]() Usually result of forced inversion of the foot
Usually result of forced inversion of the foot
![]() Associated with malleolar or distal fibula fractures
Associated with malleolar or distal fibula fractures
![]() May be associated with rupture of the deltoid ligament
May be associated with rupture of the deltoid ligament
![]() Presents with foot laterally displaced with the skin very taut over the medial aspect of the ankle joint
Presents with foot laterally displaced with the skin very taut over the medial aspect of the ankle joint
![]() Technique
Technique
![]() Place one hand on the heel and the other on the dorsum of the foot
Place one hand on the heel and the other on the dorsum of the foot
![]() Apply longitudinal traction to the foot
Apply longitudinal traction to the foot
![]() While assistant applies countertraction to the leg, gently manipulate the foot medially. Successful reduction usually produces a palpable thud.
While assistant applies countertraction to the leg, gently manipulate the foot medially. Successful reduction usually produces a palpable thud.
POSTERIOR DISLOCATION (FIGURE 67.1)
![]() Usually result of forced plantar flexion or a strong forward force applied to the posterior tibia
Usually result of forced plantar flexion or a strong forward force applied to the posterior tibia
![]() Most are associated with a fracture of one or more malleoli
Most are associated with a fracture of one or more malleoli
![]() Presents with the ankle held in plantar flexion with foot shortened in appearance and resistant to dorsiflexion
Presents with the ankle held in plantar flexion with foot shortened in appearance and resistant to dorsiflexion
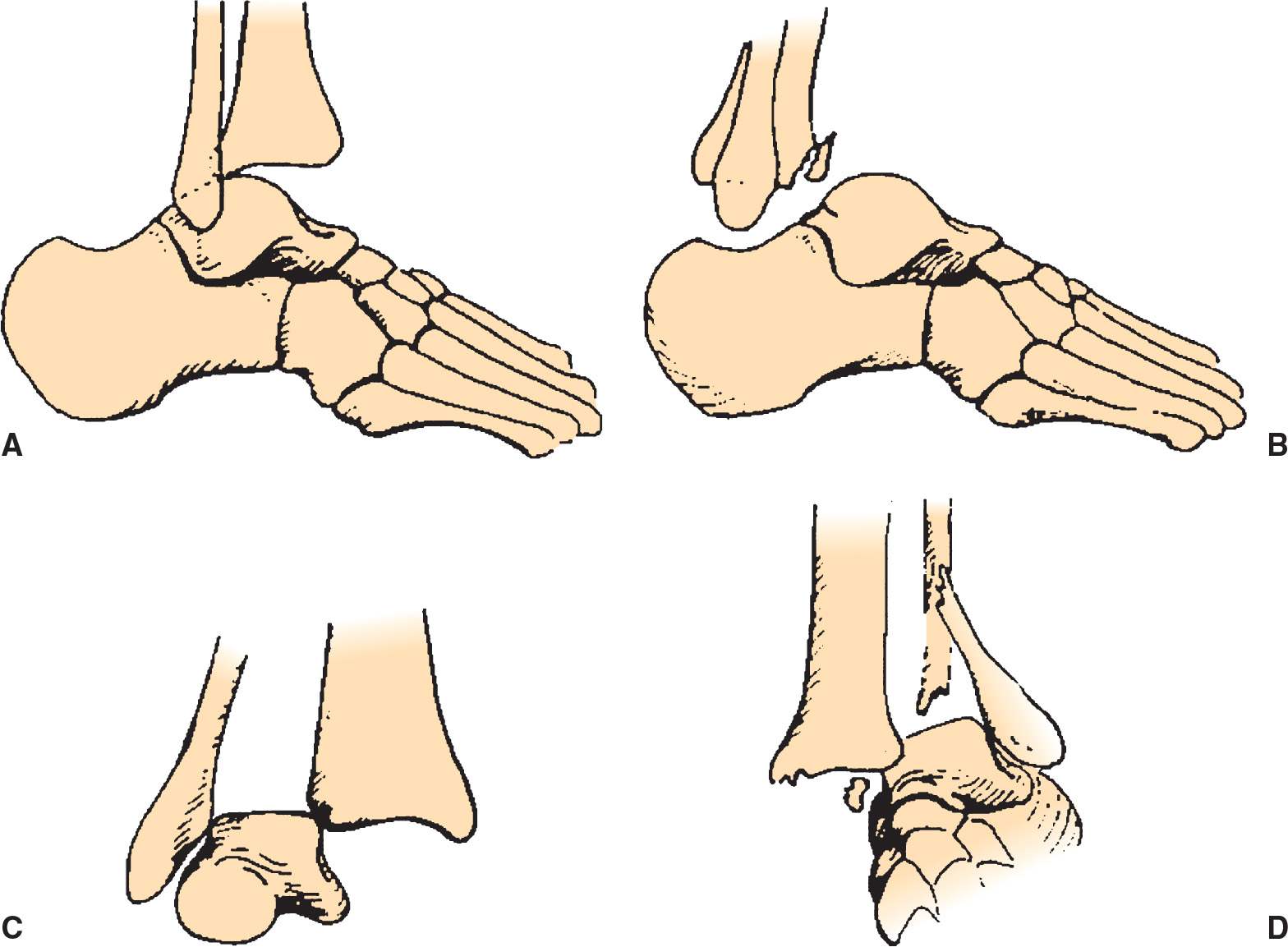
FIGURE 67.1 Four types of ankle dislocations. A: Posterior. B: Anterior. C: Superior. D: Lateral. (From Simon RR, Brenner BE. Emergency Procedures and Techniques. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002:285, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


