Joanne Sandberg-Cook
Ankle and Foot Pain
In the United States, foot and ankle problems are extremely common, with an incidence rate of 24% in middle-aged and older adults.1 Sports injuries are often the cause, but even activities of daily living stress the foot and ankle. Walking alone puts up to 1.5 times the body weight on the foot. The average person logs roughly 1000 miles yearly. During 1 hour of strenuous exercise, feet cushion up to 1 million pounds of pressure.
Foot and ankle pain is more prevalent in women, people who are older and obese, and those with other lower extremity joint pain or deformity. However, children and adolescents are also commonly injured during sports activities. The specific functions of the ankle and foot predispose them to injuries and disorders that can result in chronic problems if they are not identified quickly and managed properly.
Ankle Sprains
Definition and Epidemiology
The uniaxial ankle joint, or ankle joint, is the most primitive joint in the body and is crucial to walking, running, and the performance of all sports. The limited motion of the ankle gives it stability. The ankle joint consists of three major bones: the tibia, fibula, and talus. The tibia and fibula form the ankle mortise, and the talus fits into this mortise. The talus, which has no muscle or tendon attachment, gives the ankle its hinge motion. The talus also bears the entire weight of the extremity during walking. The deltoid, anterior talofibular, calcaneal fibular, and posterior talofibular ligaments hold the ankle bones in the mortise.
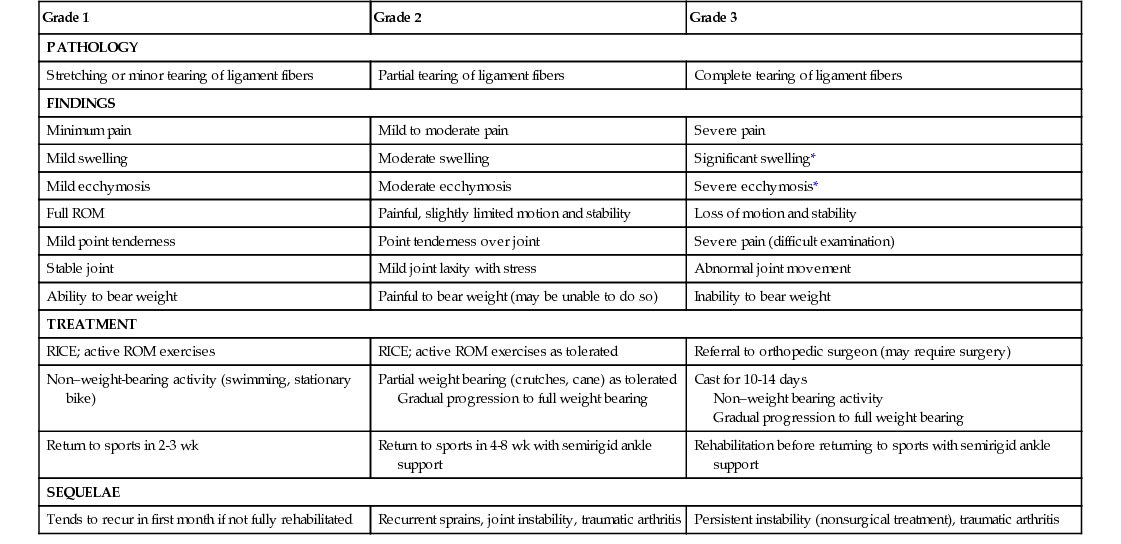
Ankle sprains occur at all ages and are common problems encountered by health care providers. A review of literature reveals that ankle sprain account for 15% to 20% of all sports injuries.2 A sprain is a ligamentous injury caused by an abnormal motion, a sudden change in direction, or a misstep on an uneven surface. Even a minor ankle sprain can jeopardize joint stability. The severity of the physical findings determines the sprain category (Table 171-1), and the category defines the management of the injury. Previous ankle sprains can increase the potential for injury recurrence. Early diagnosis, treatment, rehabilitation, and subsequent ankle support during activity decrease the recurrence of a sprain in a previously injured ankle.
TABLE 171-1
Classification and Treatment of Ankle Sprains
| Grade 1 | Grade 2 | Grade 3 |
| PATHOLOGY | ||
| Stretching or minor tearing of ligament fibers | Partial tearing of ligament fibers | Complete tearing of ligament fibers |
| FINDINGS | ||
| Minimum pain | Mild to moderate pain | Severe pain |
| Mild swelling | Moderate swelling | Significant swelling* |
| Mild ecchymosis | Moderate ecchymosis | Severe ecchymosis* |
| Full ROM | Painful, slightly limited motion and stability | Loss of motion and stability |
| Mild point tenderness | Point tenderness over joint | Severe pain (difficult examination) |
| Stable joint | Mild joint laxity with stress | Abnormal joint movement |
| Ability to bear weight | Painful to bear weight (may be unable to do so) | Inability to bear weight |
| TREATMENT | ||
| RICE; active ROM exercises | RICE; active ROM exercises as tolerated | Referral to orthopedic surgeon (may require surgery) |
| Non–weight-bearing activity (swimming, stationary bike) | Partial weight bearing (crutches, cane) as tolerated Gradual progression to full weight bearing | Cast for 10-14 days Non–weight bearing activity Gradual progression to full weight bearing |
| Return to sports in 2-3 wk | Return to sports in 4-8 wk with semirigid ankle support | Rehabilitation before returning to sports with semirigid ankle support |
| SEQUELAE | ||
| Tends to recur in first month if not fully rehabilitated | Recurrent sprains, joint instability, traumatic arthritis | Persistent instability (nonsurgical treatment), traumatic arthritis |
Pathophysiology
Two types of injuries cause an ankle sprain. The most common is the inversion injury, in which the foot plantar flexes and internally rotates as the ankle inverts. The “roll” of the ankle injures the lateral ligaments and can also cause a lateral avulsion fracture. The less common eversion injury occurs when the ankle sustains an external rotation mechanism. Eversion stress injures the medial structures of the ankle, damaging the deltoid ligament or the syndesmosis.
Clinical Presentation
The most common presentation of an ankle sprain is a swollen and painful joint. Ecchymosis and decreased range of motion are generally present. In many instances, weight bearing causes pain; some patients are unable to bear any weight on the affected joint.
In obtaining the history, it is important to determine whether the patient heard any audible sounds at the time of injury. An audible “snap” or “pop” indicates the potential for a more serious injury. Immediate swelling or ecchymosis raises the index of suspicion for a fracture or substantial amount of joint involvement. Patients also commonly report a sensation of lightheadedness, nausea, or diaphoresis immediately after the injury.
Physical Examination
With a sprain, the ankle joint is often swollen and ecchymotic, and the edema can create an illusion of deformity. Limited active and passive motion and point tenderness at the site of injury are common. Joint laxity is present in more severe sprains. Muscle spasm often prevents accurate testing of strength and stability. If the injury is not acute, swelling and ecchymosis at the lateral aspect of the foot and the toes are common. With severe ankle sprains, tenderness may extend up the extremity. The entire lower limb should always be palpated.
Diagnostics
Although guidelines for radiography are controversial, plain radiographs are recommended for severe injuries, especially when instability is present or fracture is suspected. An x-ray study of the lower leg should also be performed if there is tenderness at the fibular head to rule out fracture. With less severe injuries, radiographs can be used to exclude an avulsion injury. More extensive radiologic examinations, such as stress films or computed tomography (CT) or magnetic resonance imaging (MRI) scans, are considered in consultation with an orthopedic surgeon, especially preoperatively.
Differential Diagnosis
Ankle injuries range from simple strains to severe injuries. The possibility of associated fibula fracture, stress fracture, avulsion fracture, or dislocation should be considered. Bursitis and tendinitis should be included in the differential diagnosis, especially if no distinct injury is recalled. Osteoarthritis, rheumatoid arthritis, and gouty arthritis are also common causes of ankle pain and swelling, especially in the older adult.
Management
The severity of the sprain dictates the management (see Table 171-1). Rest and protection, ice, compression, and elevation (RICE) are key first steps in providing pain relief and limiting swelling. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help with pain management and may allow faster rehabilitation, although they can be associated with gastrointestinal (GI) side effects and in older adults should be used cautiously because of cardiovascular and renal concerns.2 Topical NSAID gels are very effective at reducing pain and swelling and improving function in grade 1 and 2 sprains.3 Thromboembolic deterrent (TED) hose provide support to the entire lower limb, aid in circulation, and are less bulky than ankle splints or braces for grade l and 2 sprains. Casting for 10 to 14 days has been shown to be effective in grade 3 sprains.2 Semirigid supports used after the acute injury has resolved may protect from subsequent sprains. All sprains require rehabilitation to restore the ankle to a stable and pain-free state. It is important for patients to understand that the treatment and recovery process will take weeks. Rehabilitation should begin as soon as possible after the injury and should include range-of-motion and strengthening exercises.4,5 Even a severely swollen ankle can be mobilized with the simple exercise of “writing the alphabet” (active range of motion) with the affected foot. A program of active and passive resistive exercises progresses as range of motion and strength improve.
Complications
Ankle sprains can recur within the first month if the ankle has not been fully rehabilitated. Grade 2 and 3 sprains carry with them an increased risk of joint instability and traumatic arthritis. Recurrent sprains, which result in chronic instability, may require surgical repair.5 A weak ankle joint is at risk for fracture when it is stressed.
Indications for Referral or Hospitalization
Fractures, dislocations, or subluxations and grade 3 sprains require an orthopedic referral. Physical therapy may also be indicated to promote rehabilitation and a safe return to sports or work-related activities.
Patient and Family Education
Patients need to understand the importance of RICE as well as the necessity of preventing weight bearing on the injured ankle. Patients and family members should also be instructed in medication doses and side effects, proper elastic bandage wrapping technique, cast care, and crutch use. The recuperative process and the risk of recurrence also require explanation.
Achilles Tendinopathy
Definition and Epidemiology
The Achilles tendon is posterior to the ankle joint and is responsible for flexion and extension of the ankle. It attaches the gastrocnemius and the soleus muscles of the calf to the calcaneus muscle and is palpable from the distal pole of the calf to the calcaneus. Disorders of the Achilles tendon include tendinosis, paratendonitis, insertional tendinosis, and frank rupture.
Achilles tendinitis manifests as pain with or without swelling around the Achilles tendon. Unlike other tendons, the Achilles tendon does not have a synovial sheath but instead has a paratenon, which, like a synovial sheath, functions to provide lubrication and vasculature to the tendon. Except for severe cases, true Achilles tendinopathy primarily affects the paratenon, resulting in inflammation, degeneration, and friability of the tendon.6 A nodule of mucoid degeneration can form in the body of the tendon in severe or chronic Achilles tendinitis.6
Pathophysiology
Achilles tendinopathy can occur in both adolescents and adults in both traumatic and nontraumatic settings. Aging, improper training, running up hills, or wearing shoes with soles that are too rigid can also contribute to the development of Achilles tendinopathy. Shoes or boots with a high back can irritate the tendon, causing pain and inflammation. Wearing of shoes with heels that maintain plantar flexion (high heels) for long periods can cause the tendon to shorten. Changing to flat or running shoes then increases stress on the tendon, causing pain. On occasion, Achilles tendinitis is caused by an anatomic abnormality, such as excessive foot pronation or tight hamstrings or gastrocnemius muscles.6,7
Clinical Presentation
Patients with Achilles tendinopathy may have intermittent symptoms and may describe a pain that subsides during exercise but increases in severity while at rest. Pain can be located in the heel (insertional tendinopathy) or along the length of the tendon (tendinosis). Morning stiffness or severe pain on climbing stairs is also common. Most patients have an abnormal gait. Some limp, and some walk on their toes to avoid the heel-strike phase of walking.
Physical Examination
Localized swelling may be present around the tendon. There may be a bony prominence at the heel known as a Haglund deformity. Pain is often worse in the morning or after a period of inactivity and aggravated by shoe pressure. A palpable nodule, inflammatory signs, and crepitus may be present in severe or chronic cases.7
Diagnostics
Radiologic or laboratory tests are usually unnecessary, but the appropriate diagnostic tests should be guided by the history. Ultrasound is inexpensive and noninvasive and can be used to rule out rupture of the tendon. MRI is the gold standard but may not be needed in mild or straightforward cases. MRI is usually done if surgical intervention is a consideration.
Differential Diagnosis
Achilles tendinopathy causes primarily heel pain. Heel pain has varied causes. Retrocalcaneal bursitis, infection, fracture, plantar fasciitis, and partial tendon rupture should be considered in the differential diagnosis of Achilles tendinopathy. Posterior calf pain can also be caused by muscle strain, bruising, or thromboembolic disease.8
Management
Treatment of the acute phase of Achilles tendinopathy begins with the cessation of all sports activities and exercise. Tendon rest is imperative to avoid further injury. Severe inflammation may respond best to immobilization in a boot or cast. Crutches and partial weight bearing may be indicated. NSAIDs, either oral or topical, and an ice massage for 20 minutes three or four times a day help decrease inflammation and pain.9 A simple shoe insert that raises the heel approximately 2 cm ( inch) also helps ease strain on the tendon. In more severe or chronic cases, ultrasound is an adjunct therapy used by physical therapists. Regular follow-up visits to assess progress and to discourage the patient from returning to activity prematurely are necessary. Resolution of acute tendinopathy can take 8 weeks or longer.7 A program of stretching and strengthening begins when pain and swelling have subsided. Many patients can recover fully with exercise alone.10 To prevent recurrence or rupture, it is essential that patients do stretching exercises before engaging in any exercise.
inch) also helps ease strain on the tendon. In more severe or chronic cases, ultrasound is an adjunct therapy used by physical therapists. Regular follow-up visits to assess progress and to discourage the patient from returning to activity prematurely are necessary. Resolution of acute tendinopathy can take 8 weeks or longer.7 A program of stretching and strengthening begins when pain and swelling have subsided. Many patients can recover fully with exercise alone.10 To prevent recurrence or rupture, it is essential that patients do stretching exercises before engaging in any exercise.
Severe cases unresponsive to conservative treatment may benefit from surgical debridement. In rare cases, tendon transplant to augment the strength of the damaged tendon may be necessary.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






