
Ankle and Foot Injuries
Kaushal Shah and Natasha Desai
Ankle injuries are among the most common sports-related and extremity injuries presenting to the emergency department (ED) accounting for approximately 20 million injuries per year and up to 20% of all sports injuries (1,2,3). Although the vast majority are benign injuries, there are instances when immediate action and emergent consultation are necessary.
The ankle and foot are relatively simple structures. The ankle is formed by (a) the tibia, which forms the medial malleolus, the posterior malleolus, and the plafond (ceiling); (b) the fibula, which forms the lateral malleolus; and (c) the talus (Fig. 45.1). The ankle is held together by (a) the medial ligaments collectively termed deltoid ligament; (b) the lateral ligaments–-anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL); and (c) the syndesmosis between the distal tibia and fibula (Fig. 45.2). The foot has three general parts: the hindfoot (calcaneus and talus), the midfoot (navicular, cuboid, and cuneiforms), and the forefoot (metatarsals and phalanges) (Fig. 45.1).
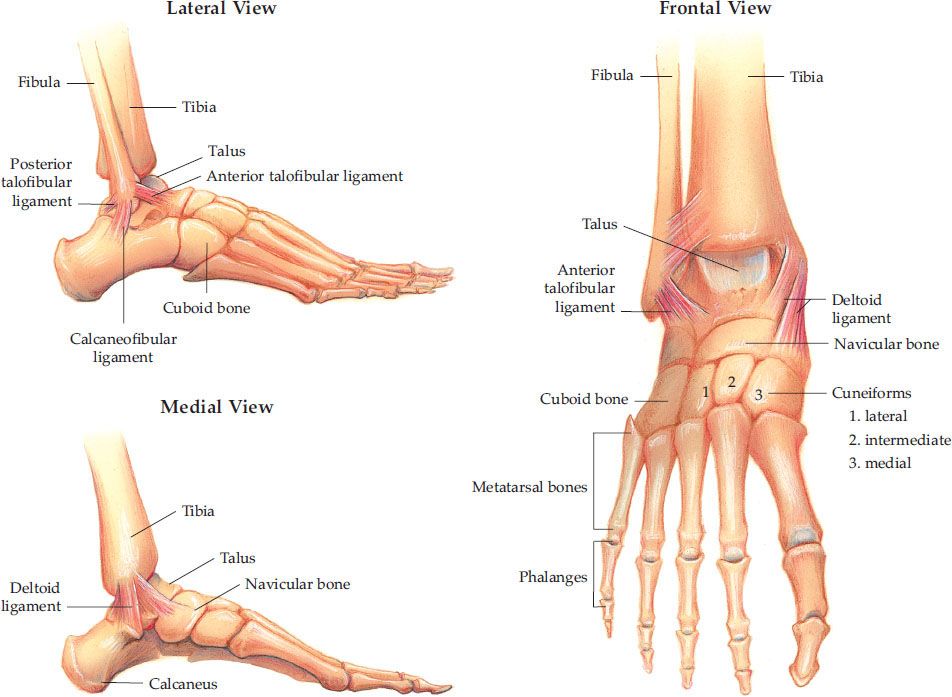
FIGURE 45.1 Anatomy of ankle and foot.
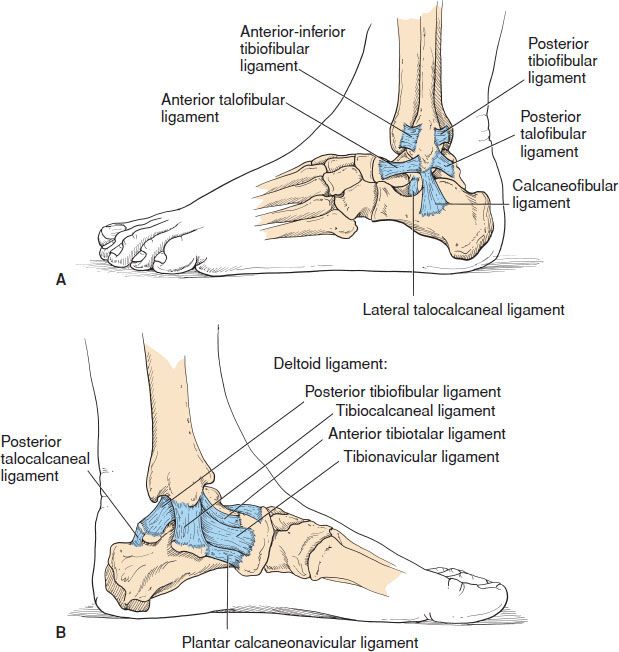
FIGURE 45.2 Ankle and foot – ligaments (A) lateral view; (B) medial view. (From Cipriano J. Photographic Manual of Regional Orthopaedic and Neurological Tests, 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins; 1991.)
CLINICAL PRESENTATION
Ankle injuries can be anticipated by the position of the foot and direction of the force at the time of injury. Other key factors include the ability to ambulate after injury and a history of previous injuries (1). Most common “red flags” suggestive of a fracture rather than a sprain are inability to bear weight, significant swelling, or tenderness. The ankle should be considered as a closed ring with the tibia, fibula, and talus as the main parts held together by ligaments. A break in two or more places results in instability.
ED EVALUATION AND MANAGEMENT
Ankle Ligamentous Injuries
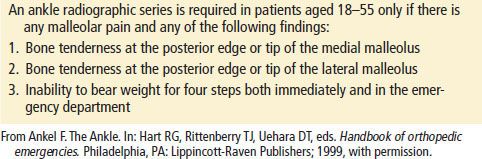
Approximately 90% of ankle ligamentous injuries are due to inversion of the ankle, resulting in sprain of the lateral ligaments, most commonly the ATFL (1). Significant injuries from an eversion mechanism are far less common because the broad deltoid ligament is strong and resistant to tears. The clinical findings associated with ankle sprains range from mild pain and swelling to severe pain with edema and ecchymosis. Neurovascular status should be checked by palpating the posterior tibial and dorsalis pedis pulses, checking capillary refill, and assessing distal sensation. However, without gross deformity, it is extremely unlikely that the neurovascular status will be compromised. Palpation of the medial and lateral malleoli and the base of the fifth metatarsal for focal tenderness are critical to evaluate for associated fracture. The Ottawa Ankle Rules (OAR) are useful in determining which patients do not need radiographic evaluation for an ankle injury; the sensitivities range from 97% to 100% (Table 45.1) (4–6). In the pediatric population, the OAR have been shown to be 98.5% sensitive for predicting significant ankle and midfoot fractures in a meta-analysis of 12 studies which included 3,130 children older than 5 years (B). If x-rays are obtained, the physician should inspect the AP view for talar shift and malleolar fractures, the mortise view for widening of the tibiotalar joint, and the lateral view for posterior malleolar fracture and general alignment.
TABLE 45.1
Ottawa Criteria for Ankle Radiographs
Provocative tests for ankle stability are necessary to determine the grade of injury. eTable 45.1 describes the grading of ankle sprains. The anterior drawer test assesses the integrity of the ATFL (Fig. 45.3). The test is positive if greater subluxation is noted on the injured ankle than the opposite one. The talar tilt test can be used to assess the lateral and medial ligaments (Fig. 45.3). If there is significant subluxation with inversion, tears of the ATFL or CFL should be suspected. Significant subluxation with eversion raises suspicion for a tear of the deltoid ligament. Integrity of the tibiofibular syndesmosis can be tested via the squeeze test, which involves squeezing the proximal tibia and fibula together. If pain is elicited, the test is positive (eFig. 45.1).
eTABLE 45.1
Classification of Ankle Sprains
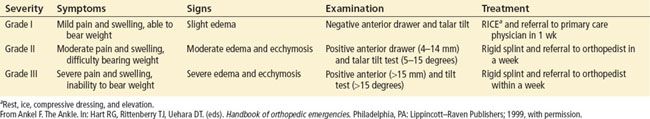
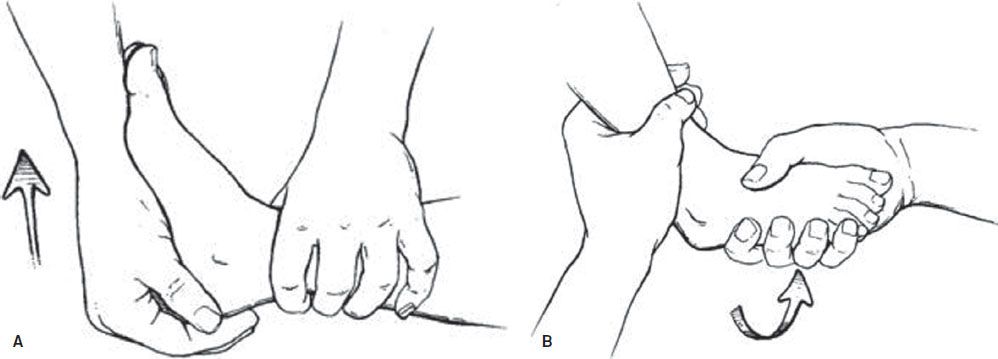
FIGURE 45.3 A: The anterior drawer test is performed by placing the patient’s heel in the palm of the examiner’s hand with the ankle at a 90-degree angle to the long axis of the leg. The examiner gently, but firmly, moves the heel and foot forward (arrow). B: In the talar tilt maneuver, the heel is firmly adducted (arrow) and assessed for increased laxity or instability compared with the noninjured side. (Adapted from Fleisher GR, Ludwig S, Henretig FM, et al. Textbook of Pediatric Emergency Medicine. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)

eFIGURE 45.1 The squeeze test—practitioner squeezes the tibia and the fibula together. If pain is elicited, it suggests a tibiofibular syndesmosis injury. (From Dale Berg, Katherine Worzala. Atlas of Adult Physical Diagnosis. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)

eFIGURE 45.2 X-ray of a pilon fracture in a 46-year-old man, resulting from an axial load in a motorcycle accident. A: AP view. B: Lateral view.
Acutely, ibuprofen 10 mg/kg (not to exceed 800 mg) PO or acetaminophen 15 mg/kg (not to exceed 1,000 mg) PO should be administered for pain. Ketorolac 30 to 60 mg IM or IV, in an adult, is also effective. General management guidelines follow the “RICE” mnemonic: rest ankle and avoid reinjury which may entail use of crutches; ice the ankle for 20 minutes three to four times per day for the first day to reduce swelling; compress with an elastic ACE wrap or ankle brace to reduce swelling and pain; elevate the extremity as often as possible to reduce swelling. eTable 45.1 describes the management based on the grade of the injury. If serious ligamentous injury is suspected, resulting in joint laxity (i.e., grade II and higher sprains), more rigid splinting methods should be considered. An air stirrup splint is moderately effective in preventing inversion and eversion of the ankle and is appropriate for grades I and II ankle sprains. For grade III injuries, a short-leg posterior rigid splint (e.g., plaster) that runs from midcalf to the toes should be used to further immobilize the ankle to prevent worsening of the injury and promote healing.
All patients with ankle sprains can be discharged home but should have appropriate follow-up within 1 week. Although pain and swelling should abate and the ability to ambulate should improve with time, occult fractures and high-grade sprains may require further orthopedic or sports medicine care. Other indications for orthopedic referral include (a) a “pop” that is heard or felt, (b) a history of several previous injuries, (c) medial ankle tenderness, (d) a positive squeeze test or other stress test, and (e) grade II and higher sprains in children with open growth plates (7). In children, less force is required to sustain a Salter–Harris I fracture than is required to tear a ligament (see Chapter in Pediatric Section, “Extremity fractures”). Thus, any patient who is suspected of having a significant ankle sprain and no clear fracture on x-ray should be splinted and referred to an orthopedic surgeon for follow-up.
Ankle Fractures
Ankle fractures can present after a significant traumatic mechanism or after a simple ankle inversion or eversion twisting injury. There are several types of ankle fractures that should be considered in the differential diagnosis. A lateral malleolus fracture is the most common type of ankle fracture resulting from inversion of the ankle. Isolated medial malleolus fractures are less common because the injury requires more force than a lateral malleolus fracture. Therefore, other associated fractures and joint instability should be suspected. Patients with bi- or trimalleolar fractures present with significant pain, swelling, and ecchymosis, and associated dislocations are common. A distal tibial fracture through the articular surface is called a plafond fracture. Although commonly used interchangeably with the term plafond fracture, a pilon fracture is specifically a comminuted plafond fracture that results from an axial compression force to the tibial plafond (eFig. 45.3). The Maisonneuve fracture is an oblique fracture of the proximal fibula associated with a medial malleolus fracture or deltoid ligament tear. It can easily be missed if the proximal fibula is not routinely palpated in patients with ankle-twisting injuries. These last two fractures require radiographs of the entire tibia and fibula.

eFIGURE 45.3 Technique for posterior dislocation reduction.
As with ankle sprains, neurovascular status should be checked immediately. The history and physical examination are identical to that of ankle sprains. If there is gross deformity, a dislocation should be considered and should be reduced emergently if there is neurovascular compromise. Lacerations and wounds should be examined closely to ensure that an open fracture is not present.
Suspected ankle fractures require x-rays in three views as described above. The two most common classification systems for ankle fractures are the Lauge-Hansen and Danis–Weber. The Danis–Weber classification system is simpler and is based on the location of the fibular fracture (Fig. 45.4). A fibular avulsion fracture below the tibiotalar joint line is called a Weber type A fracture. If the fibular fracture is in the joint line, it is a Weber type B fracture. Fractures above the joint line disrupting the syndesmosis ligament are termed Weber type C fractures.
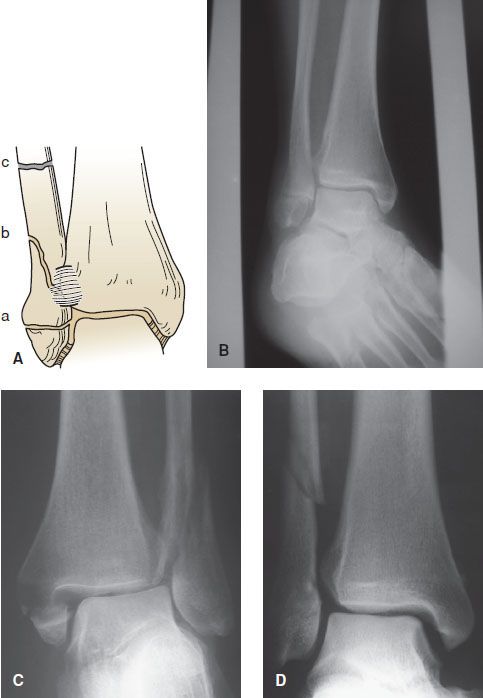
FIGURE 45.4 A: Schematic diagram of the Danis–Weber classification of ankle fractures. B: A type A fracture where the anterior tibiofibular ligament remains intact. C: A type B fracture with the fracture extending through the ligament. D: A type C fracture where the fracture is above the joint line. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
Patients should receive adequate analgesia. Intravenous, intramuscular, and subcutaneous injections are preferred (rather than oral administration) until it is certain the patient will not require an operative procedure. Isolated lateral or medial malleolar fractures without instability can be safely discharged home without orthopedic consultation in the ED. The emergency physician should first place the ankle in a posterior splint, provide crutches for nonweight bearing, provide adequate analgesia, and ensure close orthopedic follow-up. All other ankle fractures will require orthopedic consultation in the ED.
Isolated fractures of the distal tibia and fibula should be immobilized in a short-leg posterior splint. A sugar tong splint (U-splint) can also be used; it wraps along both the medial and lateral sides of the leg with the base of the “U” under the foot (similar to an air stirrup) and is more effective in stabilizing the medial and lateral ligaments. Patients with severe injuries to the ankle, such as bi- and trimalleolar fractures, should be placed in both a posterior splint and a sugar tong splint (“AO” splint). This provides immobilization similar to that of casting but allows for the expected ankle swelling.
Ankle Dislocations
For the talus to dislocate from the distal tibia, multiple ligaments are torn, and there are often associated malleolar fractures. Significant force is required, and there is always gross deformity and inability to bear weight.
The emergency physician should perform immediate reduction if there is neurovascular compromise or significant skin tenting with concern for conversion into an open fracture–dislocation. In cases of uncomplicated dislocations, x-ray evaluation should precede reduction.
Reduction of the ankle requires conscious sedation and two assistants. For posterior dislocations, the first assistant flexes the knee to 45 degrees and applies counter-traction over the calf while the second assistant pushes down on the front of the lower leg. The physician applies traction to the heel and forefoot after first plantar flexing the foot and then lifting the heel (eFig. 45.3). For anterior dislocations, the first assistant flexes the knee to 45 degrees and applies counter-traction over the calf while the second assistant lifts up on the lower leg. The physician should dorsiflex the foot initially to disengage the talus and then push downward on the foot (eFig. 45.4). For lateral dislocations, the physician applies longitudinal and medial traction whereas an assistant applies counter-traction.
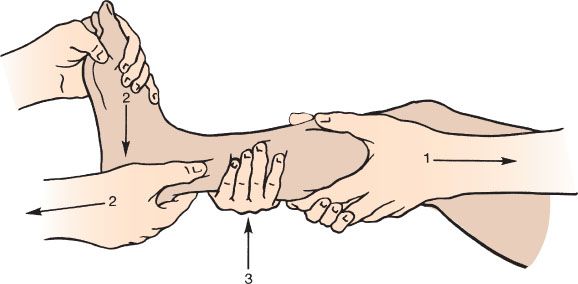
eFIGURE 45.4 Technique for anterior dislocation reduction.









