Fig.
64.1
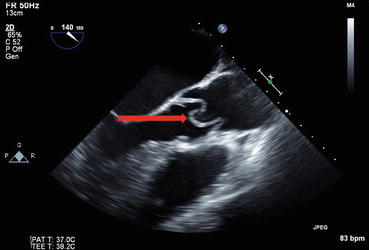
Fig.
64.2
Questions
- 1.
What do the images show?
- 2.
How is this condition created?
- 3.
What are the presenting features of this condition?
- 4.
How is this condition classified?
- 5.
What end organ complications can we expect?
- 6.
What is the role of imaging and laboratory testing?
- 7.
What is the treatment of choice?
Answers
- 1.
- 2.
Acute aortic syndromes have very high mortality and need a very high index of suspicion for diagnosis. Acute aortic dissection, intramural hematoma, and penetrating aortic ulcer are all considered to be acute aortic syndromes [1].
Aortic dissection is a disruption of the medial layer of the aortic wall with bleeding within or along the wall of the aorta. The blood may tear through the adventitia or back into the intima creating a dissection flap. Acute aortic dissection is rapidly fatal, 40% patients die immediately, about 20% patient die during or immediately after surgery, and only about half the patients are alive 5 years out from surgery [2, 3].
Conditions that place extreme stress on the aortic wall (hypertension, deceleration injury, weight lifting) or lead to degeneration of the aortic media (genetic syndromes, inflammatory vasculitides, bicuspid aortic valve) can increase the risk of aortic dissection.
- 3.
Presenting symptoms are sudden onset and severe chest, back, or abdominal pain that is described as tearing or ripping in quality [4, 5]. Some patients with acute aortic dissections may not have any chest pain at all and may present with syncope and shock like state. Patients also present with perfusion defects and end organ damage depending on the extension of the dissection flap, with resulting neurological deficits, myocardial ischemia, renal insufficiency, mesenteric ischemia, or limb ischemia.
On physical exam, patients may demonstrate perfusion deficits in the form of a pulse deficit and systolic blood pressure deferential. Vascular examination of all four extremities should be conducted in all patients with suspected aortic dissection [6].
- 4.
Get Clinical Tree app for offline access
Thoracic aortic dissections are classified according to the involvement of the various segments of the thoracic aorta. Accurate classification is necessary to decide on surgical versus medical management. Two classification schema have been proposed: DeBakey and Stanford. The Stanford classification is more widely used, it classifies thoracic aortic dissections based on the involvement of the ascending aorta into:
- (a)
Stanford A: involving ascending aorta (before the brachiocephalic artery). Urgent surgery is recommended.
- (b)
Stanford B: involving the descending aorta only (after the left subclavian artery). Surgery usually not recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



- (a)

