GENERAL PRINCIPLES
• Lipophilic drugs produce rapid induction of general anesthesia
• Most IV anesthetics exert effect through activation or augmentation of postsynaptic GABAA receptors (↑ chloride influx → hyperpolarization → ↓ neuronal excitability)
• An ideal anesthetic drug provides amnesia, analgesia, immobility, and hypnosis; “balanced anesthesia” uses combinations of drugs to achieve these aims
• Infusions used for maintenance of GA; this total intravenous anesthesia (TIVA) is a useful, though costly, option in selected scenarios (e.g., MH susceptibility, severe PONV)
• Low-dose infusions/small incremental boluses used for procedural sedation, regional anesthesia adjunct
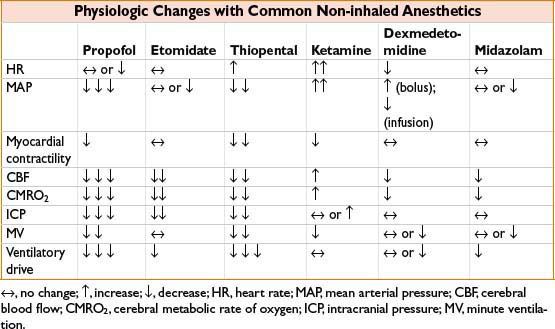
• Most IV anesthetics are capable of causing transient apnea with induction doses; respiratory depressant effects ↑ by co-administration of narcotics
• Direct myocardial depressant properties “unmasked” by hypovolemia, critical illness, or catecholamine depletion; use caution and adjust dosing accordingly
• Agents with varying extent and route of metabolism show similar duration of action after bolus (induction) dosing because termination of effect is due to redistribution to skeletal muscle or fat
• Drugs bound to plasma proteins are unavailable for uptake by target organs; dosing for highly protein-bound drugs may need adjustment in disease states with ↓ protein production (CHF, malignancy, renal or hepatic failure)
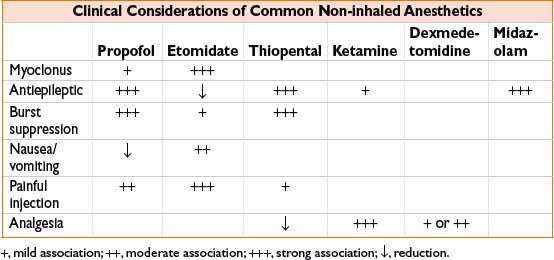
PROPOFOL (DIPRIVAN)
• Widely used for anesthetic induction, though associated with CV depression
• Reduce/titrate dose for elderly, critically ill, hypovolemic (↓ central distribution volume, ↓ clearance → ↑ myocardial depression)
• Infusion common for MAC and TIVA; rapid clearance makes context-sensitive half-life <40 min for infusions up to 8 hrs
• Hepatic and extra-hepatic clearance to inactive metabolites; minimal kinetic changes in renal/liver disease
• Insoluble alkylphenol formulated in lipid emulsion containing egg yolk lecithin (most egg allergies are to egg white antigens, though avoidance prudent with clear hx of egg anaphylaxis)
• Lipid emulsion supports bacterial growth linked to sepsis; observe aseptic technique and use within 12 hrs of opening
• Prolonged infusion linked to rare but lethal syndrome of arrhythmias, lipemia, metabolic acidosis, rhabdomyolysis
FOSPROPOFOL (LUSEDRA)
• Water-soluble propofol prodrug, indicated for adult procedural sedation via IV bolus
• Give bolus doses >4 min apart to prevent dose stacking while prodrug is transformed
• Key features: ↓ pain on injection, slower onset, ↑ duration of action compared to propofol
ETOMIDATE (AMIDATE)
• Favored for induction in hemodynamically unstable patients due to minimal direct myocardial depression, though may still cause hypotension in hypovolemic patients
• Adrenal suppression (blocks hydroxylases in cortisol pathway) limits use as infusion; importance of transient effect after single dose is highly controversial, may affect outcome in sepsis (Intensive Care Med. 2011 Jun;37(6):901–910)
SODIUM THIOPENTAL (PENTOTHAL)
• Barbiturate with favorable neurologic profile, used for neuroprotection during ↓ cerebral perfusion
• Large doses can be titrated to ↓ EEG activity (burst suppression) in neurosurgery and status epilepticus
• Generally ↑ CV stability than propofol, though effect varies markedly based on cardiac function, volume status, autonomic tone
• Alkaline solution precipitates with acids (e.g., neuromuscular blockers); severe tissue injury with extravasation (rx with local anesthetic infiltration) or intra-arterial injection (rx with papaverine, regional sympathetic block)
• Unavailable in USA after controversy over use for capital punishment. (ASA Statement on Sodium Thiopental’s Removal From the Market. January 21, 2011)
METHOHEXITAL (BREVITAL)
• Barbiturate with cardiorespiratory and injection considerations similar to thiopental
• More rapid hepatic clearance than thiopental → ↓ elimination t1/2
• Uniquely activates epileptic foci facilitating electroconvulsive therapy and identification of seizure foci during ablative surgery
KETAMINE (KETALAR)
• Phencyclidine derivative with unique action through NMDA receptor
• Produces analgesia, unique dissociative hypnosis (limb movement, eye opening common), potent bronchodilation
• Perioperative adjuvant dosing associated with ↓ postoperative opiate use (Cochrane Database of Systematic Reviews, 2006)
• Relative preservation of respiratory and CV function (sympathomimetic)
• Adverse effects include ↑ cardiac work, ↑ oral secretions, direct myocardial depressant effect seen with catecholamine depletion (sepsis, trauma)
• Dose-dependent psychomimetic effects (e.g., hallucinations), ↓ with co-administration of benzodiazepines
• Oral and IM routes useful for non-cooperative patients
DEXMEDETOMIDINE (PRECEDEX)
• Selective α2 adrenergic agonist with sedative, amnestic, analgesic effects
• Approved for procedural and short-term (<24 hr) ICU sedation; slower onset/offset than propofol
• Desirable for sedation with very minimal respiratory depression, maintenance of arousability
• Perioperative opioid use ↓ when used as adjunct
• Adverse qualities include dose-dependent hypotension and bradycardia, ↑ cost
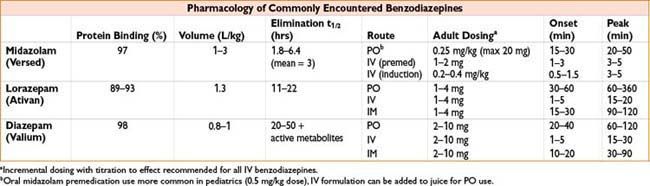
BENZODIAZEPINES (SEE THE TABLE ON NEXT PAGE)
• Effective premedications (usually midazolam); produce anxiolysis and amnesia
• Associated with ↓ respiratory depression than barbiturates; unique ability to be antagonized by flumazenil (see Chapter 2H-58)
• Potent anticonvulsants useful for status epilepticus, alcohol withdrawal, local anesthetic toxicity
• Duration of effect depends on hepatic clearance rate (midazolam >> lorazepam > diazepam)
• Midazolam used for infusion; caution due to association with ↑ delirium, renal excretion of active metabolite
• Diazepam, lorazepam cause pain on injection due to propylene glycol solvent
• Large (GA induction) doses of midazolam may cause ↓ preload and afterload, prolonged sedation
< div class='tao-gold-member'>









