Beckwith–Wiedemann
Wilms’ tumor
Macroglossia, hemihypertrophy, hepatoblastoma, hypoglycemia
Cerebro-oculo-facial
Renal agenesis, cryptorchidism
Arthrogryposis, microcephaly, cataracts
CHARGE
Small genitalia
Coloboma, congenital heart defects, choanal atresia, ear anomalies
Cornelia de Lange
Small genitalia, cryptorchidism
Micromelia, bushy eyebrows
Ehlers–Danlos
Hydroureter
Skin hyperextensibility, poor wound healing
Laurence–Moon–Biedl
Small genitalia
Obesity, retinitis pigmentosa, polydactyly
Marfan
Renal duplication, hydroureter, cryptorchidism
Aortic aneurysm, arachnodactyly
Prader–Willi
Cryptorchidism
Hypotonia, obesity, mental retardation
Prune belly
Hydronephrosis, cryptorchidism
Hypoplastic abdominal muscle, congenital heart defects, pulmonary hypoplasia, intestinal atresia, malrotation, leg maldevelopment
Robinow
Small genitalia, cryptorchidism
Short forearms, flat face
VACTERL
Hydronephrosis, renal dysplasia, hypospadias
Vertebral anomalies anorectal atresia VSD choanal atresia tracheoesophageal fistula deafness
In well children, having day-case procedures, e.g., circumcision, hypospadias, and preoperative testing, is not required. Anesthetic assessment for major urological surgery must ensure that hematology and biochemistry are within normal limits. Analgesic techniques commonly involve central neuraxial blockade for urological procedures. Contraindications such as congenital spinal abnormalities, local and systemic infections, bleeding diathesis, and absence of consent should be excluded. In congenital conditions, e.g., cloacal exstrophy, associated with a high incidence of spinal abnormalities, imaging of the spinal cord should be undertaken before any regional technique is considered.
Anesthetic Management
Posterior Urethral Valves
Posterior urethral valves occur in 1:25,000 – 80,000 live births. The abnormality results in congenital obstruction of the urethra and can be life threatening in the neonatal period [11]. It is usually diagnosed in the antenatal period as a result of fetal hydronephrosis. When severe, decreased fetal urine output leads to oligohydramnios and if this occurs at the time of pulmonary development, it leads to pulmonary hypoplasia and respiratory complications at birth.
The urethral obstruction affects the entire urinary tract causing back pressure and renal insufficiency. Newborns can present with severe systemic illness requiring early surgical intervention, e.g., cystoscopy and urethral valve ablation. Endotracheal intubation and careful monitoring of ventilatory pressures are essential. Analgesia is best managed using a caudal technique where possible. Spinal anesthesia has also been documented [12]. Particular care should be taken maintaining normothermia as neonates are prone to hypothermia and warmed irrigating fluids should be used for cystoscopy. Other methods to maintain temperature such as a warm theatre suite, intravenous fluids, and warming blankets should also be used.
Hypospadias
Hypospadias is a relatively common congenital defect. The external urethral meatus may be located anywhere along the ventral surface of the penis (Fig. 9.1). There may be an associated abnormal ventral curvature of the penis (chordee) and an abnormal distribution of the foreskin (hood), with a ventral deficiency [13]. The severity depends on how proximally the urethral meatus is located. In most cases the urethral meatus is placed distally – glandular, coronal, or distal penile, while the perineal position is rare.
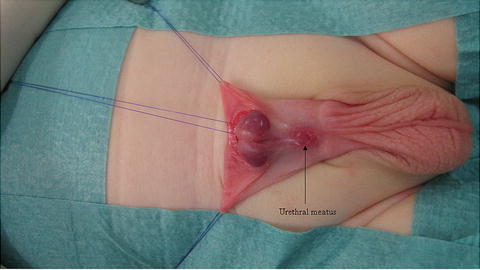
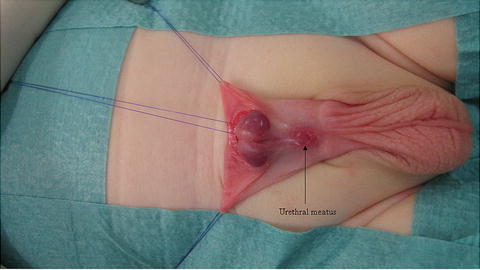
Fig. 9.1
Hypospadias
The incidence in the United States is 1 in 250 live births and is thought to have doubled between 1970 and the 1990s [13]. Environmental estrogenic pollutants and increasing maternal age are two suggested reasons for the increase. Several other factors have been implicated, but no single factor explains this embryological anomaly. The etiology may have a genetic component with an increased incidence in children whose fathers are similarly affected [13].
In cases of distal hypospadias, surgical repair is straightforward. In severe cases when the meatus is more proximal, periscrotal, scrotal, or perineal, reconstruction is complex [14]. The proximal intact urethra may have segments of the urethra that are thin ventrally. There may also be some degree of penile rotation along the long axis. Surgical correction is usually undertaken at 6–18 months and involves correction of the chordee and reconstruction of the urethra (urethroplasty) to produce a good cosmetic appearance. In complex cases the urethroplasty may be staged. If there is inadequate local tissue for the reconstruction, particularly in repeat procedures, a buccal mucosal graft may be required [15].
Hypospadias is not associated with an increased incidence of other congenital anomalies, but the diagnosis should prompt a search for other associated anomalies, e.g., cryptorchidism and inguinal herniation due to a persistent processus vaginalis. If hypospadias occurs in association with a unilateral or bilateral undescended testicle or ambiguous genitalia, a genetic and endocrine consultation should be made to exclude congenital adrenal hyperplasia (CAH) and other intersex conditions. The investigation should be completed prior to presentation for surgery so that appropriate steroid dosing can be instituted if required. Renal function is usually normal unless the hypospadias occurs in the presence of other renal abnormalities.
General anesthetic combined with a regional anesthetic technique is the usual method of choice. In infants, an endotracheal tube with controlled ventilation is preferable. This allows a better control of the end-tidal carbon dioxide when the duration of the surgical procedure is unpredictable. This technique may also be appropriate for proximal and redo cases that may require a mucosal graft. In older children with mild distal hypospadias, a laryngeal mask with spontaneous ventilation may be more appropriate. The incidence of postoperative nausea and vomiting is low, especially if opiates are avoided with the use of regional analgesia [16].
Minor cases should be carried out as day cases, whereas more complex cases require inpatient stay. In day-case procedures, analgesia should be provided with care not to delay mobilization. A caudal extradural block is an effective analgesic technique for hypospadias and reduces postoperative opioid analgesic requirements [17, 18]. Bupivacaine 0.25% at 0.8 ml.kg−1 usually produces an adequate block. Levobupivacaine 0.25% which has a better safety profile can also be used. Duration of action is about 6–8 hours when no additives are added. To prolong the duration of action of the local anesthetic, many different additives have been described including clonidine, ketamine, and tramadol [19–22]. No additional intraoperative analgesia may be required and acetaminophen (paracetamol) 15 mg.kg−1 may be saved for the postoperative period [23]. Nonsteroidal analgesics should be prescribed if there are no contraindications.
A penile block may be appropriate for distal hypospadias surgery and is associated with a lower incidence of urinary retention [24]. However, penile block is not appropriate for proximal or more complex cases. The volume of local anesthetic used for the penile block should be given some consideration. Recommended doses suggest 0.1 mls.kg−1 of 0.5% bupivacaine, with 5 mls as a maximum dose.
Intravenous fluids should be given based on the severity of hypospadias and duration of the surgical procedure. Postoperatively a compression dressing may be applied. Urinary drainage may be necessary postoperatively with either an indwelling or a suprapubic catheter. An early complication is hemorrhage requiring fluid resuscitation and urgent hemostasis.
The Acute Scrotum
Torsion of the testicle is a urological emergency. There are many potential differential diagnoses (Table 9.2) for testicular torsion, but due to the difficulty in excluding torsion on clinical grounds, most are managed by emergency exploration. However, Doppler ultrasound has been shown to have specificity of 100% and a negative predictive value of 97.5% [25].
Table 9.2
Differential diagnoses of the acute scrotum
Torsion of the testis |
Torsion of the spermatic cord |
Torsion of the appendage/epididymis |
Epididymitis/orchitis |
Hernia/hydrocele |
Trauma/sexual abuse |
Tumor |
Idiopathic scrotal edema (dermatitis, insect bite) |
Cellulitis |
Vasculitis (Henoch–Schönlein purpura) |
Normally, the tunica vaginalis covers the anterior surface of the testis, the epididymis, and the spermatic cord. If it only covers the spermatic cord, then the testis is suspended freely and may rotate in the tunical cavity. The testicle twists on the spermatic cord causing vascular compromise. There is usually a 4–8 hour window before ischemia causes irreversible damage to the testicle.
Testicular torsion presents with sudden onset of severe unilateral testicular pain [26]. Cold weather, causing cremasteric muscle activity, or trauma may be precipitating factors. The cause of sudden unilateral testicular pain in the 13–21 year age group is testicular torsion in 80–90% cases. In the prepubertal age group, other differential diagnoses are more common but torsion still accounts for 35% of the cases [27].
Two types of testicular torsion occur: extravaginal, largely confined to the perinatal period, prior to testicular descent into the scrotum where torsion of the testicle occurs proximal to the tunica vaginalis, and intravaginal testicular torsion which occurs within the tunica vaginalis. Extravaginal torsion is associated with abnormal fixation of the tunica vaginalis, sometimes referred to as bell-clapper deformity. Surgery involves untwisting of the testicle and assessment for viability. If viable, fixation in the scrotum is performed. In both types, the contralateral side is also fixed [28].
Torsion of the testis commonly presents out of hours, and surgery should proceed as soon as possible without waiting for adequate fasting. Even if the child is sufficiently starved, pain and distress or opioid analgesics may delay gastric emptying, and a rapid sequence induction is indicated in most cases. Testicular manipulation may elicit a vagal response; therefore, atropine or glycopyrrolate should be available. A multimodal technique to manage pain, using a combination of acetaminophen and NSAIDs, should be used. Infiltration with local anesthetic by the surgeon may be helpful in older children although a caudal extradural block is commonly used in the younger age group. Intravenous opioids (fentanyl 1–2 μg.kg−1, morphine 100–150 μg.kg−1) are also appropriate for this procedure. Incidence of postoperative nausea and vomiting is high, and therefore, prophylactic antiemetics, e.g., ondansetron and dexamethasone should be given.
Circumcision, Preputioplasty, and Meatotomy
Circumcision is one of the oldest and most commonly performed urological procedures, and the WHO estimates that approximately 30% of all males are circumcised worldwide [29]. The prepuce is adherent during intrauterine development and late in gestation spontaneous separation occurs. At birth the prepuce is almost always nonretractile, and by 5 years of age, 70% still have some adhesions. Left alone the majority becomes completely retractile by adolescence. Therefore, routine circumcision for physiological phimosis is not advocated. However, in the developing world, circumcision is encouraged as there is evidence to suggest circumcision reduces the rate of HIV transmission [29].
Religious circumcision is commonly performed in the neonatal period in both Muslim and Jewish communities. Historically, there has been controversy regarding analgesic requirements. Evidence indicates that analgesia avoids the adverse effects of gagging, choking, and emesis [30]. Therefore, efforts must be made to alleviate pain. A ring block or dorsal nerve block of the penis is recommended and should be used by appropriately trained clinicians. These techniques appear to be safe in newborns. Eutectic mixture of local anesthetic (EMLA) cream is more effective than the use of sucrose, but methemoglobin levels were evaluated in two trials, and it is not recommended in infants [31].
Medical indications for circumcision include conditions causing chronic progressive sclerosing inflammation. The foreskin is fibrosed and abnormally adherent and can affect the glans causing urinary retention, necessitating meatotomy and removal of the foreskin.
Most children undergoing circumcision are physically well, and therefore, it is commonly carried out on an ambulatory basis. Airway management using a laryngeal mask airway (LMA) is appropriate, although in infants, an endotracheal intubation is preferable [32]. In infants, the highly compliant chest wall, with less negative intrathoracic pressure and small airway resistance, increases the work of breathing. This results in a tendency to airway closure during tidal breathing. At induction of anesthesia, the reduction in functional residual capacity (FRC) further compounds this problem. Breathing spontaneously with an LMA in situ results in a progressive increase in ventilation and perfusion mismatch in infants. Ventilation through an LMA in this age group easily causes abdominal distension due to the respiratory mechanics. Intubation and ventilation allows the use of positive end-expiratory pressure (PEEP) to reverse these changes [32].
A regional anesthetic technique in combination with simple systemic analgesia using acetaminophen and nonsteroidal agents provides adequate analgesia. A single-shot caudal or a penile block may be used. Caudal additives may help prolong the duration of analgesia. Delayed mobilization occurs because of leg weakness due to a motor block; therefore, a penile block may be preferable for day surgery [31]. Ultrasound-guided penile block may be superior to landmark technique with respect to reduced postoperative pain scores in the first hour and time to first subsequent analgesic requirement [17, 31, 33]. Ultrasound-guided bilateral injections into the subpubic space, deep to Scarpa’s fascia, helps to visualize the spread of the local anesthetic as it comes into contact with the deep fascia, but the dorsal penile nerve cannot visualized [17, 33].
Post-circumcision Bleed
Incidence of significant hemorrhage following circumcision is 0.8% [34]. It may necessitate urgent return to the operating room for hemostatic control. Bleeding can be profuse and is usually underestimated. Asking parents how many diaper changes have been necessary prior to presentation may give some indication as to the extent of blood loss. Clinical assessment of blood loss using capillary refill time, pulse rate, blood pressure, and urinary output should be undertaken. Considerable blood loss is possible and resuscitation should be commenced as soon as possible. Good intravenous access should be secured, and it is essential that full blood count, crossmatch, and a coagulation profile be obtained. Hemoglobin levels may not reflect blood loss in the absence of adequate resuscitation. The patients may have been fed so a rapid sequence induction and intubation are indicated. Fluid resuscitation should be guided by clinical parameters, and blood transfusion may be required. Post-circumcision hemorrhage may also be the initial presentation of a previously undiagnosed bleeding disorder.
Cystoscopy and Urolithiasis
Cystoscopy is performed for both diagnosis and treatment of pediatric urological conditions. It may form part of the investigation for recurrent urinary tract infection, urinary incontinence, hematuria, and the assessment of urological anomalies. Therapeutic procedures may be carried out for correction of urethral stricture, posterior urethral valves, and urolithiasis.
Diagnostic cystoscopy is generally a short procedure and is commonly performed using a laryngeal mask airway with spontaneous respiration; however, infants should be intubated [32]. Therapeutic procedures may be considerably longer, and intubation with controlled ventilation may be more appropriate. At the time of insertion of the cystoscope, urethral stimulation may provoke laryngospasm; therefore, it is important to ensure an adequate depth of anesthesia and analgesia. Cystoscopy may be complicated by hemorrhage, and a secure intravenous access is recommended. Prophylactic antibiotics are required and either gentamicin 5 mg.kg−1 or Co-amoxiclav 30 mg.kg−1 is given as indicated. A combination of simple analgesics such as acetaminophen, nonsteroidal agents, and short-acting opioids, e.g., fentanyl, along with local anesthetic gel applied locally to the urethra may be sufficient for postoperative analgesia. In the postoperative period, the patient should be monitored for hemorrhage. A rare complication of seizures secondary to dilutional hyponatremia caused by absorption of irrigation fluid can be prevented by avoiding the use of hypotonic intravenous fluids [35].
In patients suffering from recurrent urolithiasis, efforts should be made to exclude and treat underlying metabolic abnormalities, e.g., hypercalcemia, hyperoxaluria, and cystinuria. Stones are managed by extracorporeal shock wave lithotripsy (ESWL), laser lithotripsy, endoscopic removal, percutaneous nephrolithotomy, or open approaches. Unlike in adults ESWL is commonly performed under general anesthesia rather than sedation. Prophylactic antiemetic therapy is indicated.
Orchidopexy
Cryptorchidism, absence of one or both testes from the scrotum, is most commonly due to failure of testicular descent during normal embryological development. It affects 3.7% of term infants at birth, but this number reduces to 1% by 3 months of age [36]. If left untreated, from the age of 2 years, there is gradual loss of germ cells with progressive atrophy, azoospermia, and increased risk of cancer. To preserve fertility and reduce the risk of testicular malignancy, orchidopexy is indicated and involves location of the testis along with its fixation in the scrotum.
The surgical procedure performed depends on the anatomical location of the testis. Ultrasonography may identify the position but has a high rate of false positives and negatives. Therefore, if the testis is not palpable, the initial surgical procedure may be a diagnostic laparoscopy to detect an intra-abdominal testis. Before proceeding, an examination under anesthesia may be diagnostic
Orchidopexy is usually carried out between 6 and 12 months of age as an ambulatory procedure. A palpable undescended testis is usually managed with a single-stage orchidopexy via an inguinal or scrotal incision [37]. Dissection requires traction on the spermatic cord which may cause vagal stimulation. However, intra-abdominal testis may require a two-stage laparoscopic procedure. In the initial stage, surgical dissection allows greater mobility of the testis, but the blood supply becomes precariously dependent on the vessels to the vas deferens. The second stage is performed 6 months later and may be a combined inguinal and laparoscopic procedure to fix the testis in the scrotum.
Anesthesia can be performed using inhalation or intravenous induction depending on the age of child and the anesthesiologist’s preference. If laparoscopy is to be performed, endotracheal intubation and pressure-controlled ventilation is preferred. With an inguinal or scrotal approach, a laryngeal mask airway (LMA) with a volatile agent of choice in oxygen and air or nitrous oxide is adequate.
Analgesia should be provided using a caudal or ilioinguinal block [17]. Ultrasound-guided ilioinguinal block may be adequate for an inguinal approach, but if a scrotal incision is used, additional infiltration is required [38]. Ilioinguinal block using 0.25% bupivacaine 0.5 ml.kg−1 on either side is recommended.
Caudal extradural block using 1 ml.kg−1 of 0.25% bupivacaine achieves analgesia up to T10. Testicular innervation is derived from the aortic and renal plexuses and sympathetic fibers connecting to the T10 and T11 segments of the spinal cord. Caudal additives help to prolong the duration of the block and are useful in ambulatory patients [39, 40].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







