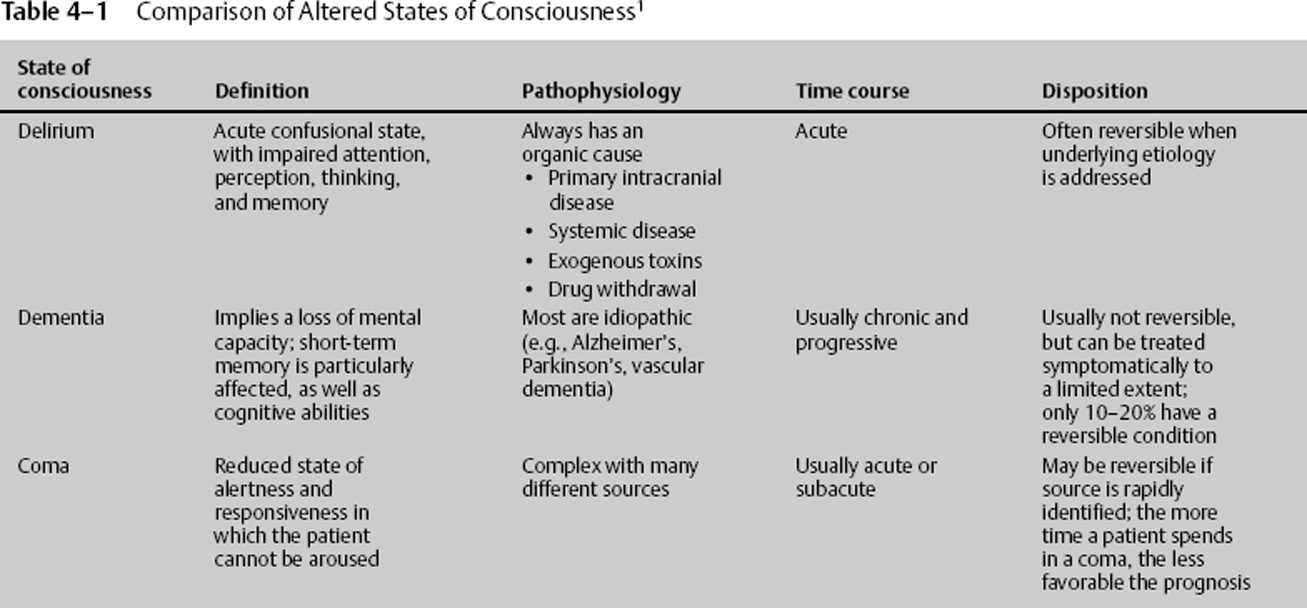
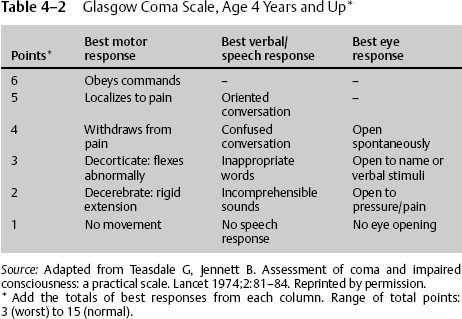
4 Jeffery M. Jones and Dan Miulli Before discussing the causes, categories, workup, or treatment of an altered level of consciousness (ALOC), it is necessary to give a brief description of the term consciousness. Although this subject frequently lends to long philosophical debates, consciousness exists to perceive that which exists. That which exists includes subjects such as people, places, things, the actions of that which exists, time, and a multitude of other mental functions such as concept formation and the ability to manipulate these concepts. Consciousness is the awareness of self and the environment in which we live. It is the physician’s responsibility to evaluate these mental processes and compare them within the context of the patient’s age, medical condition, baseline level of mental functioning, and numerous other factors, including comparison to the average mental functioning of the general population. What follows is the evaluation process, along with the differential diagnosis and initial management, of these patients in the neurosurgical intensive care unit (NICU). There are three major categories of ALOC that should be defined: delirium, dementia, and coma. Coma will be discussed in Chapter 5. The main differences between dementia and delirium are etiology and time course of the disease process. Delirium is generally due to more acute, reversible processes, whereas dementias tend to be due to chronic irreversible diseases. Table 4–1 summarizes the characteristics of each.1 The most common methods for evaluating a patient’s mental status as an inpatient are the Glasgow Coma Scale (GCS) and the Mini-Mental State Examination (MMSE). Other methods of evaluation of mental status and disability are available, but they are rarely used in the inpatient setting due to limited time and use in following the patient’s day-to-day progress. This being said, it may be of some utility to use more comprehensive functional scales to follow the patient’s progress over time. An in-depth functional predischarge assessment can be reviewed and contrasted for each clinic follow-up appointment. It will also provide rehabilitation services with an idea of the patient’s baseline following the neurologic insult. The rehabilitation physician, neurointensivist, neurologist, and neurosurgeon should determine, and, if possible, agree upon the best choice of in-depth functional assessment and grading scale for tracking progress. Coma is considered to be a GCS score of 8 or less (see Chapter 5). An additional measurement, the National Institutes of Health (NIH) Stroke Scale, may also be used, particularly if the patient has focal or lateralizing motor or sensory deficits (see Tables 4–2 and 4–3).2–4 The causes of altered mentation in the NICU are slightly different than in the ER. Most NICU patients have head trauma, cerebrovascular accident (CVA), neurosurgery, or other known sources of intracranial insult that could lead to an ALOC. Many times the neurointensivist is faced with a patient who was previously alert and aware and has deteriorated. The challenge to the neurointensivist is to identify the cause of the ALOC and institute the appropriate intervention. It is beyond the scope of this book to give an exhaustive list of the possible causes of ALOC, but Table 4–4 represents the categories of causes and some of the most common causes of ALOC in each category.
Altered Level of Consciousness: Pathophysiology and Management
 Definitions
Definitions
 Evaluation of Mental Status
Evaluation of Mental Status
 Causes of Altered Level of Consciousness
Causes of Altered Level of Consciousness
|
Source: From Psychological Assessment Resources, Inc., 16204 North Florida Avenue, Lutz, Florida 33549, from the Mini–Mental State Examination by Marshal Folstein and Susan Folstein, by special permission of the publisher. Copyright 1975, 1998, 2001 by Mini Mental LLC, Inc. Published 2001 by Psychological Assessment Resources, Inc. Further reproduction is prohibited without permission of PAR, Inc. The MMSE can be purchased from PAR, Inc., by calling (813) 968-3003.
| Category of cause | Most common examples |
| 1 Trauma | SDH, EDH, contusions, DAI |
| 2 Epileptic | Seizure, status epilepticus |
| 3 Cerebrovascular | CVA, SAH, ICH, vasovagal |
| 4 Infectious | Meningitis, encephalopathy, sepsis |
| 5 Toxic/drug | Oversedation, EtOH, delirium tremens, illicit drugs, withdrawal, suicide attempts |
| 6 Metabolic | Hypoglycemia, diabetic ketoacidosis, hepatic encephalopathy, electrolyte disorders |
| 7 Cardiopulmonary | MI, respiratory distress, PE, hyperventilation |
| 8 Psychiatric | Malingering, acute psychotic episode |
CVA, cerebrovascular accident; DAI, diffuse axonal injury; EDH, epidural hematoma; EtOH, alcohol; ICH, intracerebral hemorrhage; MI, myocardial infarction; PE, pulmonary embolism; SAH, subarachnoid hemorrhage; SDH, subdural hematoma.
 Workup for Altered Level of Consciousness
Workup for Altered Level of Consciousness
The workup for ALOC is driven mainly by the clinician’s suspicion for a certain etiology. For example, a patient who has sudden onset of ALOC with tonic-clonic movements would lead the physician toward a workup and intervention for a seizure. In a patient who has a known small epidural hematoma and was GCS 15 upon admission and deteriorates to a GCS 12, a stat CT should be ordered to further evaluate the hematoma and the need for surgical intervention. If a postoperative craniotomy patient has decreasing level of consciousness and fever, the suspicion of a postoperative infection should be entertained, and a CT with contrast and a lumbar puncture (LP) will likely need to be performed. The noncontrast CT scan is used in many situations as the initial study for ALOC because it is able to give information quickly as to whether there is a need for immediate surgical intervention. Once an anatomical source is ruled out, then further testing should be ordered to find an etiology for the ALOC. Table 4–5 gives the most common diagnostic modalities in each category of cause.5–10
 Interventions for Altered Level of Consciousness
Interventions for Altered Level of Consciousness
Any particular intervention for ALOC will depend on the disease process. Processes that cause anatomical derangement should be taken care of in an emergent fashion. Subdural hematomas, epidural hematomas, contusions, and so on, are all disease processes that, if severe enough, will require emergent surgical intervention. A seizure will require anticonvulsant therapy, and if prolonged, in status epilepticus or multiple, may require emergent benzodiazepines. Cerebrovascular accidents of the ischemic type may be treated with clot-busting drugs or other interventional techniques if the time period is within certain guidelines. A large middle cerebral artery (MCA) territory ischemic stroke may require a lifesaving craniectomy. Hemorrhagic strokes may require surgical intervention if they meet certain criteria and the patient would likely benefit from evacuation of the clot. Table 4–6 shows the most common treatment modalities in each category. Many of these treatments and their specific implementation are covered in more detail in other parts of this book.
| Category of cause | Most common diagnostic modalities |
| 1 Trauma | CT without contrast, ICP monitoring, brain metabolic monitoring |
| 2 Epileptic | EEG, continuous EEG, MRI |
| 3 Cerebrovascular | CT without contrast, carotid duplex, MRA, four-vessel angiography |
| 4 Infectious | CT/MRI with and without contrast, LP, blood cultures, HIV titers |
| 5 Toxic/drug | CT (rule out anatomical disease), drug screen, toxin screen, EtOH level |
| 6 Metabolic | CT (rule out anatomical disease), metabolic profile, liver function, Schilling test, EEG, folate, vitamin B12, thyroid function |
| 7 Cardiopulmonary | CT (rule out anatomical disease), EKG, cardiac enzymes, ABG, spiral CT |
| 8 Psychiatric | CT (rule out anatomical disease), psychiatric consult, review medications and side effects |
ABG, arterial blood gases; CT, computed tomography; EEG, electroencephalogram; EKG, electrocardiogram; EtOH, alcohol; HIV, human immunodeficiency virus; ICP, intracranial pressure; LP, lumbar puncture; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging.
 Prognosis for Brain Injury
Prognosis for Brain Injury
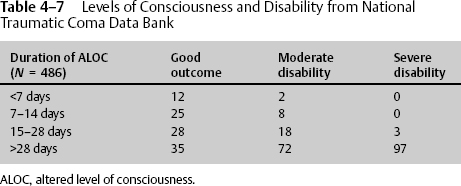
The prognosis for brain injury depends on the portion of the brain affected, duration of affect, and quantity affected. Advances in recent years have led to 20% of those with GCS = 3 surviving, with 10% having a functional survival. Those patients older than 60 years have the worst outcome. The complications of injury also affect outcome. If there is a single episode of hypotension or hypoxia, the morbidity and mortality increase. In traumatic brain-injured patients, traumatic subarachnoid hemorrhage and midline shift greater than 0.5 to 1.5 cm predicts poor outcome. The brain part injured correlates directly with the amount of life alteration. Dominant brain lesions are usually more devastating than nondominant lesions. Injuries to the brain usually have short-term effects of changes in mood, judgment, memory, behavior, depression, and headaches. The amount of change to normal lifestyle frequently depends on the degree of preinjury education, with those patients having higher education levels able to return to some productive lifestyle, whereas those with less formal education are often less able to meet the same expectations. In addition to education portending prognosis, the length of loss of consciousness lends itself to disability prediction (Table 4–7).
| Category of cause | Most common treatment modalities |
| 1 Trauma | Craniotomy for evacuation of hematoma, craniectomy for ICP control, CSF drainage, osmotic diuretics |
| 2 Epileptic | Anticonvulsants, benzodiazepines for status epilepticus, future vagal nerve stimulation, future epilepsy surgery |
| 3 Cerebrovascular | Clipping/coiling of aneurysms, clot lyses, merci extractor, stenting, endarterectomy, hematoma evacuation, craniectomy for ICP control in MCA strokes |
| 4 Infectious | IV antibiotics, surgical debridement of infected hardware or abscess, sepsis management |
| 5 Toxic/drug | Symptomatic treatment of drug and EtOH withdrawal |
| 6 Metabolic | Lactulose, glycemic control, electrolyte correction |
| 7 Cardiopulmonary | Anticoagulation, cardiology consult |
| 8 Psychiatric | Psychiatric consult, antipsychotics, review of medication and side effects |
CSF, cerebrospinal fluid; EtOH, alcohol; ICP, intracranial pressure; IV, intravenous; MCA, middle cerebral artery.
< div class='tao-gold-member'>