ALLERGIC EMERGENCIES
MICHELLE D. STEVENSON, MD, MS, FAAP AND RICHARD M. RUDDY, MD
GOALS OF EMERGENCY THERAPY
 Rapid treatment with epinephrine (intramuscularly, lateral thigh) is imperative in anaphylaxis to reverse shock and respiratory distress.
Rapid treatment with epinephrine (intramuscularly, lateral thigh) is imperative in anaphylaxis to reverse shock and respiratory distress.
 Hereditary angioedema management should include rapid, controlled airway management in cases of laryngeal edema, with prompt administration of C1-esterase inhibitor concentrate (or alternative therapy) to reduce the risk of morbidity and mortality due to acute attacks.
Hereditary angioedema management should include rapid, controlled airway management in cases of laryngeal edema, with prompt administration of C1-esterase inhibitor concentrate (or alternative therapy) to reduce the risk of morbidity and mortality due to acute attacks.
 The goals of treatment of serum sickness include removal of antigen exposure (if known), control of painful arthralgias and pruritis through nonsteroidal anti-inflammatory drugs (NSAIDs) and antihistamines, and appropriate monitoring for organ dysfunction (particularly renal involvement).
The goals of treatment of serum sickness include removal of antigen exposure (if known), control of painful arthralgias and pruritis through nonsteroidal anti-inflammatory drugs (NSAIDs) and antihistamines, and appropriate monitoring for organ dysfunction (particularly renal involvement).
 Although there is a paucity of comparative effectiveness data in children, intranasal corticosteroids are often considered to be a first-line agent in symptom management for allergic rhinitis. Oral nonsedating antihistamines and oral montelukast are common alternative therapies.
Although there is a paucity of comparative effectiveness data in children, intranasal corticosteroids are often considered to be a first-line agent in symptom management for allergic rhinitis. Oral nonsedating antihistamines and oral montelukast are common alternative therapies.
RELATED CHAPTERS
Signs and Symptoms
• Rash: Papulosquamous Eruptions: Chapter 65
Clinical Pathways
Medical Emergencies
• Dermatologic Urgencies and Emergencies: Chapter 96
ANAPHYLAXIS
Goals of Treatment
Early recognition, aggressive support of respiratory and circulatory compromise, and immediate treatment with intramuscular epinephrine in the lateral thigh are essential goals in the evaluation and treatment of anaphylaxis.
CLINICAL PEARLS AND PITFALLS
• Anaphylaxis is a life-threatening emergency which is not rare.
• Stridor, hoarseness, respiratory distress, and hypotension require rapid intervention.
• Delayed administration of intramuscular epinephrine is associated with an increased risk of morbidity and mortality.
• Most, but not all children with anaphylaxis will experience skin manifestations such as urticaria, which may be transient or masked by medications.
• Hypotension or shock may be present, but absence of circulatory compromise does not exclude the diagnosis of anaphylaxis, especially in children.
• Diphenhydramine and corticosteroids are not considered first line, but rather adjunctive therapy in the management of anaphylaxis due to lack of data regarding efficacy.
Current Evidence
Anaphylaxis is a potentially life-threatening manifestation of immediate hypersensitivity. The severity of these reactions varies from mild urticaria to shock and death. Anaphylaxis most commonly involves the pulmonary, circulatory, cutaneous, gastrointestinal (GI), and central neurologic systems.
The classic anaphylactic response is an IgE-mediated reaction that occurs after reexposure to an antigen to which the patient has previously been sensitized. The term anaphylactoid reaction is sometimes used to refer to a clinically similar syndrome that is not IgE mediated and does not necessarily require previous exposure to the inciting agent. It has become a common practice to use anaphylaxis to describe the clinical syndrome, regardless of the responsible mechanism. Although the mortality rate for children <18 years is low (estimated at 0.1 per million population), anaphylaxis causes approximately 20,000 emergency department (ED) visits per year in the United States across all age groups.
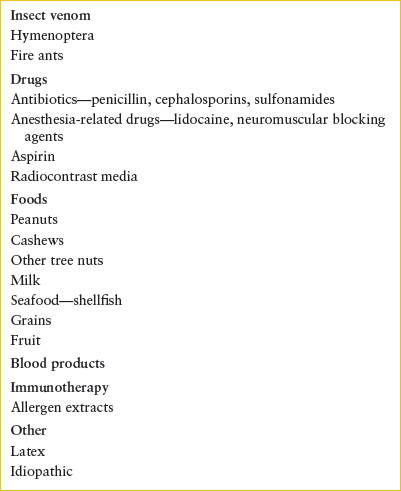
Any route of exposure, including parenteral, oral, or inhalation, has been associated with anaphylaxis. Food allergens represent the most common inciting agents among children in the United States with exposure most often occurring outside medical facilities. Other common triggers include hymenoptera stings, drugs, immunotherapy, radiocontrast media, and blood products (Table 93.1). The causative agent for anaphylaxis goes undetected in a significant proportion of cases.
TABLE 93.1
COMMON CAUSES OF ANAPHYLAXIS
Certain conditions are known to increase the risk of severe or fatal anaphylaxis. Systemic mastocytosis is a risk factor for severe anaphylaxis due to hymenoptera stings and venom subcutaneous immunotherapy. Peanut, cashew, and other tree nut triggers, especially when consumed outside the home environment, represent an important risk factor. Adolescents appear to be at the greatest risk for death, possibly due to risk-taking behavior. Asthma is also a worrisome historical feature in patients presenting with anaphylaxis, as is a delay in epinephrine administration. Most patients with a fatal reaction to a food have a history of an allergy to the specific food allergen trigger, but the severity of prior reactions may have been quite different.
During IgE-mediated anaphylaxis, IgE binds to high-affinity receptors on mast cells and basophils. The resultant sudden release of numerous mediators is presumed to be responsible for the pathophysiologic features of anaphylaxis (bronchospasm, increased vascular permeability, and altered systemic and pulmonary vascular smooth muscle tone). The most notable of these mediators is histamine, but others that have been implicated include prostaglandin D2, leukotrienes, anaphylatoxins (C3, C4a, C5a), platelet-activating factor (PAF), heparin, tryptase, and chymase. Levels of serum PAF, a proinflammatory phospholipid, are often elevated in patients with anaphylaxis and correlate with symptom severity.
Certain agents can stimulate the release of mediators directly by an unknown mechanism that does not involve IgE or complement. Agents capable of direct stimulation include hyperosmolar solutions such as mannitol and radiocontrast media. Other causes of apparent anaphylaxis have less clear mechanisms. These include reactions after the ingestion of aspirin and other NSAIDs and exercise-induced anaphylaxis in which vigorous exercise, often preceded by an allergenic food such as wheat or shellfish, is the trigger.
Clinical Considerations
Clinical Recognition
The time between exposure to the inciting agent and onset of symptoms can vary from minutes to hours, although epidemiologic data suggest that most children will experience symptoms within 30 minutes. Guidelines from multiple national and international allergy societies state that anaphylaxis is highly likely under any of the following circumstances: (1) Sudden onset of skin (e.g., urticaria, periorbital erythema, pruritus, flushing) and/or mucous membrane (e.g., oral/uvula swelling) changes in combination with either (a) acute respiratory symptoms (e.g., wheezing, stridor, or hypoxia) or (b) hypotension or signs of end-organ dysfunction (e.g., fainting/incontinence); (2) sudden involvement of at least two body organ systems after exposure to a likely allergen or trigger for that patient (skin/mucosa, GI, respiratory tract, central nervous system [CNS], or circulatory system); or (3) age-specific hypotension (or >30% decline in systolic blood pressure) after exposure to a known allergen.
Skin manifestations usually emerge first but may be absent. GI symptoms are relatively common and include nausea, vomiting, diarrhea, and crampy abdominal pain. Swelling of the lips or tongue can potentially impair swallowing and ventilation. An immediate life-threatening feature of anaphylaxis is upper airway obstruction that results from edema of the larynx, epiglottis, and other surrounding structures. Airway involvement may manifest either as subtle discomfort or pruritus of the throat, or as obvious stridor and respiratory distress. Anaphylaxis can also cause lower airway disease secondary to bronchospasm. This leads to findings similar to acute asthma, such as a sense of chest tightness, cough, dyspnea, wheezing, and retractions.
Another potential life-threatening feature of anaphylaxis is cardiovascular collapse and hypotensive shock. Arrhythmias and electrocardiographic evidence of myocardial ischemia may also be seen. These features are less commonly seen in anaphylaxis among children compared to adults. CNS involvement can include dizziness, syncope, seizures, and an altered level of consciousness.
Triage Considerations
Because evaluation and management of anaphylaxis is time sensitive, rapid identification and triage of patients presenting with signs and symptoms concerning for anaphylaxis is critical to minimize morbidity and mortality. Vital signs, pulse oximetry, and cardiopulmonary status should be immediately assessed upon arrival to the ED in children presenting with a possible “allergic reaction.” After ensuring a patent airway, supplemental oxygen should be administered if respiratory compromise is present or anaphylaxis is highly likely. Patients with circulatory compromise should be placed in the Trendelenburg position. Potential triggers should be immediately removed. Standardized protocols and immediate assembly of rescue or resuscitation teams can assist with appropriate, rapid management of affected patients. Cardiopulmonary resuscitation may be necessary in severe cases. Change in voice, difficulty in swallowing, dyspnea, and a sense of impending doom are characteristics of potentially serious anaphylaxis.
Clinical Assessment
After a rapid cardiopulmonary assessment and appropriate interventions have been initiated (see Fig. 93.1 and Management section), a more detailed assessment should be performed. The history should be directed toward determining the nature and severity of the reaction, the rapidity with which symptoms evolved, the management prior to arrival, and the evidence of ongoing progression.
Attempts should also be made to determine the offending agent. The history should focus on the 1- to 2-hour period before the onset of symptoms. While there may be history of an obvious sting or drug exposure, the association of anaphylactic reactions with food is often confusing. Although patients often identify a particular food as the cause, a more detailed history may implicate something else in the meal. For example, it is common to associate reactions with chocolate whereas the nuts in many chocolate preparations generally are the offending agents. Many patients will not have a prior history of reaction to the ingested trigger.
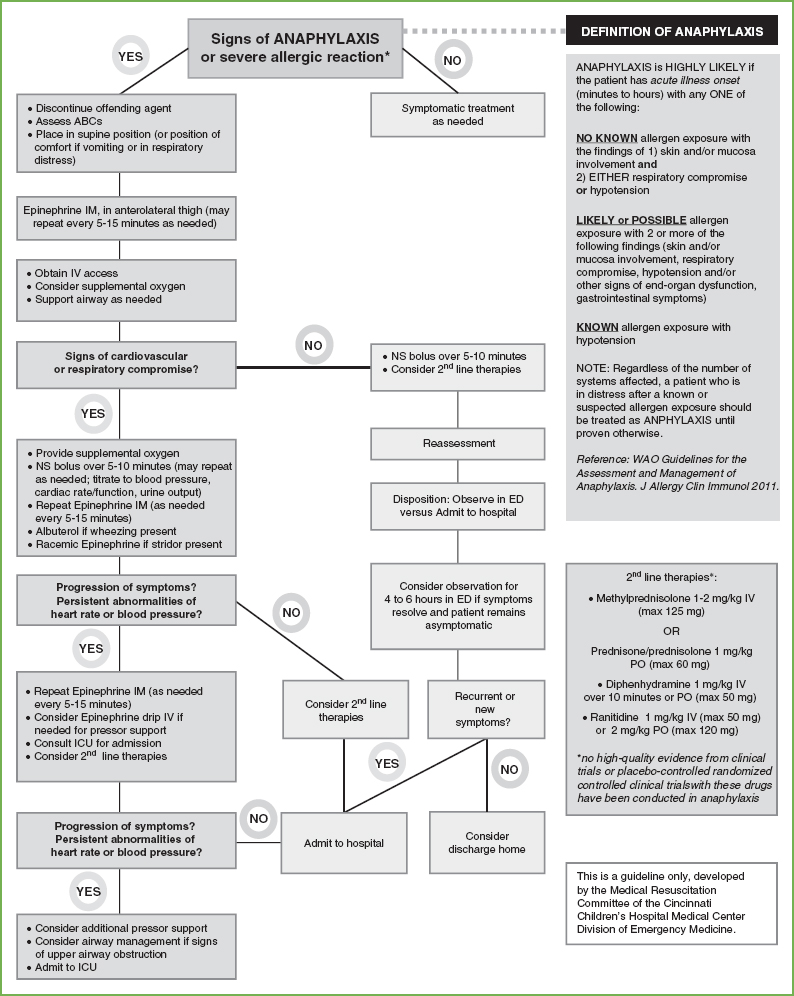
FIGURE 93.1 Anaphylaxis pathway. (From the guidelines established by the Medical Resuscitation Committee of the Cincinnati Children’s Hospital Medical Center Division of Emergency Medicine.)
Factors that may place the child at increased risk for a severe reaction should also be ascertained. These include a personal history of asthma or atopic disease or a previous allergic reaction. Although not commonly used in children, certain medications such as β-blockers, calcium channel blockers, and angiotensin-converting enzyme inhibitors may make anaphylaxis more severe or difficult to manage. Nonsteroid anti-inflammatory medications, ethanol ingestion, and concurrent respiratory illness may also exacerbate symptoms of anaphylaxis.
Anaphylaxis remains a diagnosis based upon clinical assessment. Although serum tryptase can be measured and may assist with the diagnosis of anaphylaxis in reactions in some cases, its suboptimal sensitivity and specificity, particularly in food-associated anaphylaxis, does not support routine use of this biomarker for confirmatory testing. Levels should only be considered if the diagnosis is uncertain, and appropriate follow-up of results can be assured. PAF measurements appear to have limited potential utility due to the transient nature of its elevation.
Management
Management of a life-threatening anaphylactic reaction requires simultaneous evaluation and management of the airway, breathing, and circulation, as well as the immediate administration of intramuscular epinephrine, preferably within 5 minutes. Any known trigger (e.g., intravenous medication) should be discontinued or removed promptly.
Epinephrine, the first-line drug for anaphylaxis, should be administered as soon as possible. There is no absolute contraindication for its use in anaphylaxis. Intramuscular epinephrine is indicated when anaphylaxis is highly likely or strongly suspected. It should be considered for any patient who experiences an isolated cutaneous reaction (e.g., urticaria, flushing) who also has risk factors for fatal anaphylaxis, or who has a history of a near-fatal episode, particularly when a known trigger is present. The recommendation to administer it sooner, rather than later, in the course of anaphylaxis comes from the increased likelihood of a fatal reaction among patients who receive delayed administration of epinephrine.
As an α-adrenergic agonist, epinephrine promotes vasoconstriction, which increases blood pressure and decreases capillary leakage. As a β-adrenergic agonist, it relaxes bronchial smooth muscle, increases cardiac rate and contractility, and inhibits further mediator release. Epinephrine should be administered via intramuscular injection to the thigh as a 1:1,000 solution (1 mg per mL), at a dose of 0.01 mg per kg (maximum 0.5 mL in adults, 0.3 mL in children). At some centers, pharmacy or ED storage of epinephrine 1:1,000 is not maintained, so sites have kept EPIPEN Jr (0.15 mg) and EPIPEN (0.3 mg) in the departments for convenience and safety, administering the full amount if <15 kg or >15 kg respectively. Epinephrine doses may be repeated every 5 to 15 minutes for persistent or recurrent symptoms. There is clear evidence that absorption is more rapid and peak plasma levels are greater when epinephrine is administered via the intramuscular route compared to subcutaneously.
If the patient is hypotensive or significantly hypoperfused, or if multiple intramuscular doses are ineffective, epinephrine should be administered intravenously or through an interosseous needle as a 1:10,000 solution, at a dose of 0.01 mg per kg (maximum 0.1 mL per kg) slowly over 1 to 2 minutes. In severe cases, this may need to be followed by a continuous epinephrine infusion of 0.1 μg/kg/min, which can be titrated to effect up to a maximum dose of 1 μg/kg/min. Inhaled epinephrine does not achieve adequate plasma levels and should not be substituted for the intramuscular dose during initial therapy for anaphylaxis. Ventricular arrhythmias, pulmonary edema, and hypertensive crises may be seen with epinephrine overdose.
Maintenance of the Airway
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







