Chapter 30
Airways and Emergency Airway Management 
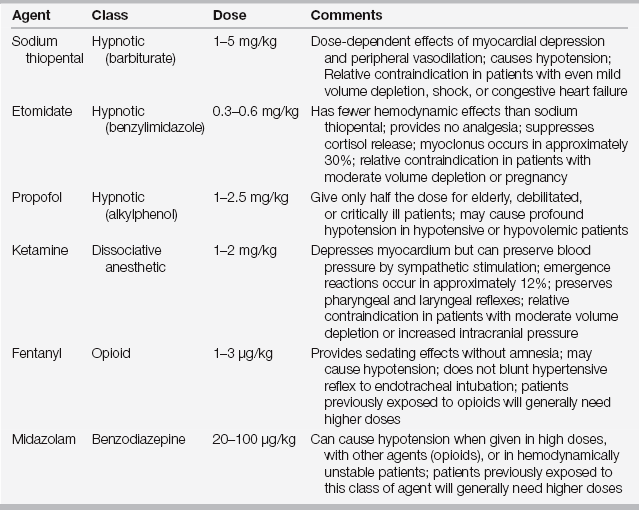
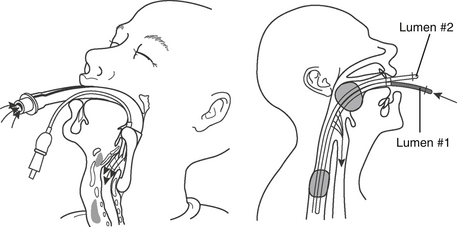
Airway management is an essential skill for the intensivist. A secure, patent airway facilitates respiratory gas exchange and clearance of orotracheal secretions, limits aspiration of orogastric contents, and can provide a route for the administration of humidified gases and some medications. Although the patient’s own anatomic airway may be sufficient to meet these needs, in the context of critical illness, invasive and non-invasive airway management techniques are often required. This encompasses familiarity with the equipment and standard techniques used for bag-valve mask ventilation, endotracheal (ET) tubes (Figure 30.1), ET intubation, and the pharmacologic agents that may be required to accomplish these maneuvers (Tables 30.1 and 30.2).
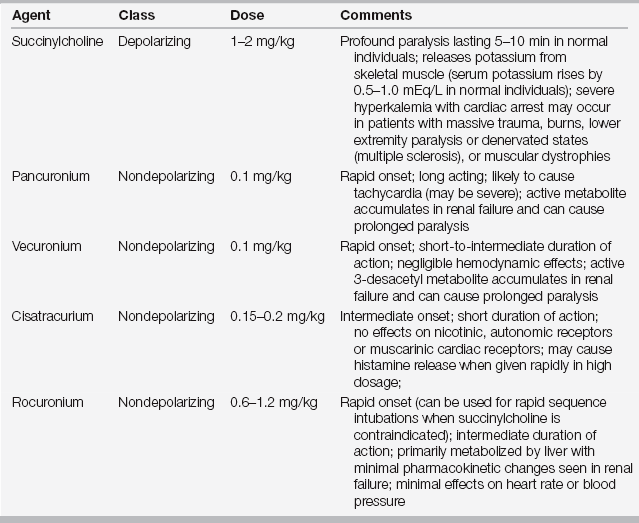
TABLE 30.2
Neuromuscular Blocking Agents Used for Endotracheal Intubation in the Intensive Care Unit
Emergency airway management in the intensive care unit (ICU) setting is potentially more technically difficult and hazardous than airway management in the elective setting. The difficult airway has been defined as the clinical situation in which a skilled operator experiences difficulty with mask ventilation, tracheal intubation, or both. When confronted with either an anticipated or unanticipated difficult airway, the intensivist should be familiar with methods of advanced or “rescue” airway management, including fiberoptic bronchoscopic intubation, laryngeal mask airway (LMA) or other blind-insertion devices, and emergent surgical airway access. Generally accepted predictors of difficult mask-ventilation or ET intubation are presented in Box 30.E1. ![]()
Useful Drugs in Emergency Airway Management
Local Anesthetics
Topical application or infiltration of local anesthetics can blunt airway reflexes and facilitate awake or semi-awake fiberoptic intubation by the oral or nasopharyngeal route. Lidocaine is used most commonly and is often combined with a vasoconstrictor designed to constrict mucosal blood vessels and minimize bleeding. Local anesthetics may be delivered topically using a standard nebulizer, a curved atomizer, an aerosol spray, or via soaked pledgets. The glossopharyngeal and laryngeal nerves may also be blocked by local infiltration, and the upper airways may be anesthetized using a transtracheal approach. Alternatively, the injection port of the bronchoscope may be used to deliver local anesthetic agents directly to the larynx as the scope is advanced into the airway.
Hypnotic Agents, Sedatives, and Neuromuscular Blockers
A variety of hypnotic agents, commonly used to induce general anesthesia in the operating room, can also be used to facilitate ET intubation in the ICU. In general these agents are selected for their rapid onset and short duration of action. Key properties and doses are presented in Table 30.1. To varying degrees, all of these agents can worsen hypotension in critically ill patients who are in shock, receiving pressors, or severely hypovolemic. Other agents, such as fentanyl, ketamine, or midazolam, can be used in these clinical circumstances and are favored during conscious sedation for semi-awake intubation or bronchoscopy. In order to produce favorable intubating conditions, hypnotic induction agents are frequently used in conjunction with a neuromuscular blocker. Since its introduction in the 1950s, succinylcholine has been the agent of choice for emergency intubation because of its rapid onset and short duration of action. Rocuronium, which approaches the rapid onset of succinylcholine without its numerous adverse effects, has gained favor. Table 30.2 lists dosing, adverse effects, and clinical considerations for the use of neuromuscular blockers for intubation.
Equipment for Emergency Airway Management
Tools for Mask Ventilation
Effective ventilation by face mask is a fundamental skill that every intensivist should master. Face mask ventilation may be lifesaving, but is sometimes underemphasized or taken for granted. Every patient room in the ICU should be stocked with a face mask and self-inflating (bag-valve mask) manual resuscitation bag that can be readily connected to wall oxygen.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree