Chapter 6 Airway management equipment
Standards, techniques (and fashions) in airway management have changed considerably over the last two decades. Although the most basic principle of anaesthesia is the maintenance of a patent airway aimed at providing adequate oxygenation and ventilation, the range of devices and products used has seen major changes especially in the focus of the designs. Of the developments in the last decade several are notable.
Numerous alternatives to the LMA have since been developed. These devices which sit outside the larynx and aim to provide a gas-tight seal are now generally referred to simply as supraglottic airways or SADs (supraglottic airway devices): the term extraglottic airway is more anatomically accurate but is not widely used.1 The number and variety of SAD designs have expanded dramatically in the last few years with the result that there are numerous products that vary considerably in materials and performance. Many of these are single-patient use laryngeal masks designed to compete for the market share of the original LMA. Nonetheless several newer SADs offer genuine advances in versatility, efficacy and safety.
Finally, overlying all the above considerations; concern about the transmission of infective agents, particularly those responsible for variant Creutzfeldt–Jakob disease (vCJD), has been the apparent driving force behind an increasing trend towards reliance on single-use airway devices. This trend, whether based on science or not (of which more later) has meant that the majority of airway devices now being developed are at least in part single-use. Production and material costs and hence price, as well as storage and stocking issues, are ultimately more significant considerations for single-use items and this is already affecting the range and quality of equipment available in many hospitals.
Fundamentals
The fundamental principle of airway management during general anaesthesia is that:
1. a clear airway must be established and maintained allowing free passage of gasses to and from the patient’s lungs. Failure to do this is likely to lead to collapse of the airway at pharyngeal or laryngeal level. Without intervention airway obstruction is inevitable and if not correctly managed, will be followed within minutes by hypoxia, brain damage and death.
Additionally it may be necessary to provide:
2. a sealed airway that enables controlled (positive pressure) ventilation and prevents loss or dilution of anaesthetic gasses
3. a protected airway that prevents the respiratory system being contaminated by regurgitated gastric contents or pharyngeal debris.
Materials used in airway devices
Plastics
The most common plastics are polyethylene and polyvinyl chloride (PVC). Polyethylene is cheap, fairly pliable, non-allergenic and can be moulded easily. It is ideal for breathing hoses, connectors and hypodermic syringes but not for the manufacture of reusable items as it will not withstand autoclaving and components may deform with repeated use. It is unsuitable for tracheal tubes (see below) as other materials cannot be easily welded or glued to its surface (e.g. cuffs). For this purpose, PVC is more suitable. PVC is brittle on its own but can be made in varying degrees of softness by the addition of plasticiszers (see below). Concerns have been raised in some areas about potentially toxic chemicals in PVC called phthalates and the potential production of both phthalates and dioxins when PVC is disposed of or incinerated.2
Materials used in tracheal tube construction are described in more detail below (p.156)
Artificial airways
Terminology
The term airway (or anatomical airway) will be used to describe the air passages within the subject, including and beyond the nasal and oral openings. The term distal refers to the part of the airway or device furthest into the subject’s airway and the term proximal to the part emerging or closest to the mouth or nose. Artificial airway then is any device that aims to maintain patency of any of the air passages. Artificial airways may be:
• simple airway adjuncts, such as the oropharyngeal and the nasopharyngeal airways. These may not be sufficient to maintain the patency of the airway on their own and may require the patient’s jaw to be supported as well. Although these are strictly speaking supraglottic devices in that their distal orifice lies above the glottis, in general usage the term SAD is not used to encompass or imply these simple airways.
• supraglottic airway devices (SAD) such as the laryngeal mask airway (LMA) and many others which aim to maintain patency of the airway on their own
• infraglottic devices, which are airway devices whose distal part lies below the glottis. Therefore they include all tracheal and tracheostomy tubes, jet ventilation catheters and cannulae, and bronchial blockers. It is a lesser used term.
Simple airway adjuncts
The maintenance of a clear airway in an anaesthetized patient can often be achieved by a simple elevation of the jaw (jaw thrust) and/or extension of the head on the cervical spine. These movements tend to separate the tongue, epiglottis and soft palate from one another and away from the posterior pharyngeal wall (Fig. 6.1). However, in many patients maintenance of the airway in this manner is either ineffective or impractical for surgery. Patients with anatomical reasons for such manoeuvres to fail include those whose ‘pharyngeal spaces’ are absolutely or relatively small (e.g. a large tongue, small lower jaw, large diameter neck, obesity and also those with large adenoid or palatine tonsils). In such patients the obstruction must be relieved and the easiest way to achieve this is by inserting a device that separates these structures and thus creates an artificial airway. These airway adjuncts may be inserted via the mouth (oropharyngeal airway) or via the nose (nasopharyngeal airway) (Fig. 6.2).
Oropharyngeal airway
These devices are shaped to emulate and so restore the space present in the pharynx during consciousness by pushing the tongue and epiglottis away from the posterior pharyngeal wall. Oropharyngeal airways are usually oval-shaped, occasionally circular, in cross-section and are produced in varying lengths and diameters to suit different patient sizes from premature neonate to large adult. The proximal end has a flange to limit the depth of insertion and prevent its loss into the pharynx. Devices are sufficiently rigid to prevent collapse should the patient bite down and indeed they may be used as a ‘bite block’ in an intubated patient (to prevent airway obstruction as a result of the tracheal tube being obstructed by biting). When inserted, the distal end should lie at the posterior of the tongue but above the epiglottis. Insertion too deep may in itself lead to airway obstruction either by mechanically pushing the epiglottis back or by irritating the sensitive laryngeal inlet leading to laryngospasm. There is a standard colour and number coding for size. The most popular oropharyngeal airway type is the Guedel pattern (Fig. 6.3). To select the correct size of Guedel airway, the distance from the flange to the distal tip of the airway should be about the same as from the patient’s lips to the tragus of the ear.
Complications
The airway may damage the front teeth, especially if:
• teeth are crowned or part of bridgework
• excessive pressure is exerted due to postoperative masseter spasm or involuntary biting
Oropharyngeal airways for flexible endoscopic oral intubation
A number of airways have been devised to assist oral intubation. When used to aid flexible endoscopic intubation they serve to deliver the endoscope behind the tongue, and as close to the larynx as possible, ideally having bypassed any secretions. Their shapes are broadly similar to the Guedel airway but often describing a fuller curvature along the length and with a more circular cross-section (Fig. 6.4).
The Berman airway (originally designed to assist blind oral intubation and pharyngeal suction), like the VBM and Ovassapian (not pictured) airways is open along one side. These devices when used for endoscopic intubation are removed before passage of the tracheal tube. The fully enclosed Optosafe airway has a large enough diameter to accommodate a tracheal tube.
The airways also act as a ‘bite block’ preventing damage to expensive fingers or delicate endoscopes (see also: Flexible endoscopes, conduit airways). This purpose is better served by the use of a dedicated bite block such as the BreatheSafe (Fig. 6.5) which more resembles a dental prop and allows full access to the oral cavity while preventing mouth closure.
Nasopharyngeal airway
The nasopharyngeal airway is designed to be passed through the nares and along the floor of the nose to deliver the tip beyond the soft palate to lie in the oropharynx, above the epiglottis. It can bypass nasal, soft palate and tongue base obstruction. The tubes have either a fixed or adjustable flange (Fig. 6.6) at the proximal end to prevent loss of the device into the nose and to limit insertion of an excessive length. The tip is bevelled to make its passage through the nose less traumatic. Some designs have a hole cut in the wall opposite the bevel to maintain patency if the tip becomes obstructed. They are produced in a range of sizes with the length of the airway governed by the internal diameter of the tube.
Nasopharyngeal airways are often indicated where a patient has limited jaw opening, awkward or fragile dentition or where an oropharyngeal airway is frequently displaced by a marked overbite. They are well tolerated by patients during relatively light levels of anaesthesia and during emergence. To avoid traumatic insertion and heavy bleeding nasopharyngeal airways are ideally soft (plastic, polyurethane or latex rubber). Avoiding excessively large tubes also minimizes complications during use, but the tube must be long enough to extend well into the oropharynx. An estimate of appropriate length is the distance from the tip of the nose to the tragus of the ear.
Facemasks
Anaesthetic facemasks are designed to fit over the patient’s nose and mouth and enable the creation of a low pressure seal. This should not require excessive force. The facemask (Fig. 6.7) consists of three parts: the mount, the body and the edge. A snug fit is achieved by incorporating one or more of the following features into the design: by anatomically shaping the body, by the use of an air-filled cuff at the edge (Figs 6.8B, D and E) that has a soft cushioning effect or by a soft pliable flap (Figs 6.8A and C) that takes up the contour of the face.
The body may be made from black rubber, neoprene, plastic, polycarbonate or silicone rubber. In some cases, a malleable wire stiffener or wire gauze is incorporated in the body so that the shape may be altered to fit the patient’s face. The transparent body of a polycarbonate or plastic facemask permits continuous inspection of the airway and respiration to be monitored by the appearance of condensation during exhalation. This is useful during anaesthesia and particularly during resuscitation. A transparent facemask also affords the possibility of seeing regurgitant matter or vomitus emerging from the mouth. Such masks are perhaps less threatening to children and anxious adults (Figs 6.8C, D and E).
The internal volume (apparatus dead space) within the body of the facemask is relatively unimportant in adults but may assume significance in neonates and infants where it can constitute 30% or more of their tidal volume. Several designs shape the paediatric facemask to minimize the apparatus dead space (Fig. 6.9). In spite of this, good fit may be more important than theoretical apparatus dead space: paradoxically in paediatrics, a larger facemask particularly of the Rendell-Baker or Laerdal type, may allow the face to fit further into the mask with improved fit and reduced effective apparatus dead space.
The edge may be anatomically shaped and fitted with a cuff or flap. A good fit is essential to prevent dilution of administered gasses by room air during spontaneous respiration and to allow positive pressure ventilation without gas leak. A variety of types and sizes of facemask must be available, since none will be a good fit for every face. Edentulous or bearded patients may be especially difficult. The former are best managed by leaving any dentures in place to prevent the cheeks from falling away from the mask and by using a smaller mask. Beards often prevent a good seal around the edge of the mask and a leak-free fit may sometimes be achieved with a bigger mask held firmly with two hands. Anaesthetists have often had to go to bizarre lengths to achieve a useful seal in heavily bearded patients (e.g. using a pierced defibrillator gel pad on the face3 or even wrapping the entire head in clingfilm4). Reusable masks with a cuff have a small filling tube fitted with a plug to enable the degree of inflation to be regulated. The plug must be removed to allow the cuff to deflate if the mask is to be autoclaved.
The shift towards disposable single-use facemasks avoids the cost of sterilization (increasingly performed off-site for many hospitals) packaging, and mandatory tracking and trace systems, but risks a reduction in quality. The same principles of design nevertheless apply to plastic disposable facemasks (Figs 6.8C, D and E). Materials and components are cheaper and of lower quality, but more importantly there is a much more limited range of designs and sizes. Most, even those for paediatric use, are essentially based on the one design of air-filled cuff and cone-shaped body. As they are reproduced with differing quality and materials by numerous manufacturers, uniformity of performance cannot be assumed. They may be advertised with bold claims of high performance and popularity but formal clinical evaluation is not a pre-requisite to bringing them to market. Several new designs have been found to be substandard and it is wise to assess performance before changing devices. Sizes do not necessarily equate between manufacturers. Some single-use masks do not allow adjustment of the volume of the air-filled cuffs and these may be both under filled and of less pliable plastic leading to a poor-quality seal. Poor design or poor fit, even in the absence of a leak, can cause areas of high pressure on the skin, which if unchecked, could lead to ulceration. Single-use masks do, however, have a number of advantages beyond sterility. These include use of inert plastics (eliminating risk of allergy to latex), transparency and even the potential to add scent to the plastic making the products more readily accepted by patients.
Many anaesthesia masks are supplied with a ring device that has several lugs protruding to allow attachment of a head harness. Older black rubber masks have a similar metal harness ring (Figs 6.8A, D and E). A head harness may be used to allow facemask anaesthesia while allowing the anaesthetist to keep both hands free. Since the introduction of supraglottic airways head harnesses are rarely used, if ever, except during non-invasive ventilation (see below).
Masks for some dental anaesthetic techniques are designed to fit the nose only, so that the dentist has unimpeded access to the mouth (Fig. 6.10). They are also known as nasal inhalers.
Facemasks are also used for non-invasive ventilation (NIV) or continuous positive airway pressure (CPAP) in differing scenarios, both in and out of hospital (see Chapter 7, Fig. 7.17). These are similar to anaesthesia facemasks and may cover the mouth and nose (conventional CPAP) or just the nose (for nasal CPAP). Such masks tend to be single-patient use devices made of plastics and soft silicone rubber. They are usually of a higher quality than single-use anaesthesia masks as comfort and tolerability is the key to treatment compliance and success. CPAP masks often incorporate additional ports for valves and airway manometry and have attachments for a retention harness to keep the mask comfortably on the patient’s face.
Supraglottic airways
History
Prior to 1988 maintaining a clear airway in a non-intubated, anaesthetized patient, might well have involved elevating and protruding the lower jaw, supporting it in this position with a Guedel airway, placing a facemask over the nose and mouth and securing this with a Clausen’s (head) harness to provide a gas-tight fit: all essentially dextrous tasks requiring practised performance. Although preceded by numerous devices that were designed to control the airway without tracheal intubation, it was not until the advent of the Laryngeal Mask Airway (LMA), first described in 1983,5 and introduced commercially in 1988, that such devices achieved success in anaesthesia. It soon became evident that the LMA allowed all the tasks described above to be replaced with a single device requiring minimal training in its use, but with an astonishing success rate in achieving a clear leak-free airway. Within a year of its introduction all UK hospitals had placed orders: the anaesthetic ‘supraglottic revolution’ had begun.
Since that time more than 40 novel, and less novel, supraglottic airway devices (SADs) have been brought to market. Since 2003 numerous manufacturers have produced copies (or near copies) of the LMA, most of them disposable and plastic. Many new supraglottic devices are based on the general design of the LMA and several are based on the Combitube (see below), which, although in origin pre-dates the LMA,6,7 was (and remains) more a device for airway rescue than for routine anaesthetic use. Other novel approaches to SAD design have met with varying degrees of success. No design has so far proven as popular as the LMA, in spite of the occasional publications claiming similar or better performance.8,9
Features
SADs generally have the following features in common:
• An inflatable cuff that sits over or above the level of the larynx. A minority of devices are cuff-less. Crucially, in all SADs, function relies on an open laryngeal inlet.
• ‘Blind’ insertion is possible, obviating the need for laryngeal visualization.
• They rely, for correct positioning, on a soft distal tip that lodges in or just above the upper oesophagus behind the cricoid ring. A minority sit well above this.
• There is an inability to guarantee tracheal isolation from gastric contents in the event of reflux or vomiting. This issue is increasingly being solved.
• The use of wide bore tubing for the airway tube (as this is not limited by the size of the larynx and trachea), and which can therefore be used as a conduit for other instruments such as a tracheal tube or a flexible endoscope.
• An ISO 15 mm male connector proximally enables connection to an angle piece, catheter mount or breathing system.
Terminology
The term originally coined to describe the generic group of LMAs and other similar devices is supraglottic airway devices (SADs). The term extraglottic has been suggested as more accurate by some authors.10 The term SAD has the advantage of primacy and widespread use and is adopted here. Several authors have attempted to classify SADs on the basis of patient or device anatomy but the classifications are cumbersome and not widely adopted.11 The author of the previous incarnation of this chapter attempted (to no avail!) to introduce the term ‘augmented supraglottic airway’ to delineate simple oral and nasopharyngeal airways from those supraglottic devices that aim to provide a gas-tight seal to the airway.
This author has coined the phrase first-generation and second-generation SADs to demarcate those devices which are simple airway tubes (first generation), from those which are designed with the intention of reducing the risk of pulmonary aspiration of gastric contents (second generation). The proposed advantage of this classification is that it is simple, is not dependant on patient/device anatomy, but is ‘patient centred’. Second-generation devices may be designed to improve patient safety, but the effectiveness of this design feature is not proven in all cases. Second-generation devices comprise the ProSeal LMA, the Combitube and Easytube, the Laryngeal Tube Suction mark II, the Streamlined Liner of the Pharynx Airway, the i-gel and the Supreme LMA.
Pharyngeal seal and efficacy vs oesophageal seal and safety
Several recent studies indicate that the extent of oesophageal seal varies considerably between different SADs.12–15 They also demonstrate that under experimental conditions in cadavers, those with a drain tube will usually effectively vent regurgitant fluid provided the drain tube is not occluded. Particulate matter has not been studied. These are important findings, though their clinical correlates are not in all cases confirmed.
First-generation SADs
The laryngeal mask airways
The LMA Classic
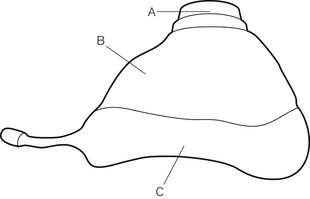
The mask (distal) end of the cLMA is made of medical grade silicone and consists of a shallow bowl resembling a small facemask, which is surrounded by an inflatable tubular cuff (Fig. 6.11). The latter, when inflated, fits around the laryngeal inlet and supports it in a position away from the posterior pharyngeal wall. The back of the bowl leads into a semi-flexible tube which passes out of the pharynx and mouth and has a 15 mm ISO male connector so that it can be attached to a breathing system. At the point the tube enters the mask, there are two thick silicone rubber strands (grilles, or bars) designed to prevent the epiglottis falling into it and occluding the lumen. The mask cuff is inflated via a pilot tube that terminates in a small ‘pilot balloon’ giving an indication of cuff inflation/deflation. A self-sealing valve prevents deflation of the cuff.
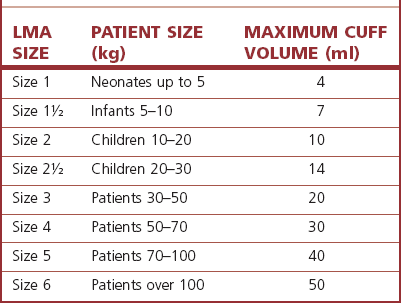
cLMAs are made from silicone rubber so that they can be autoclaved and reused. The manufacturer has designated the cLMA for 40 uses. Experience suggests the cLMA can withstand many more cycles of sterilization, but this is ‘off label’ use and cannot be recommended. Originally produced in four sizes, two mid-range sizes and two further larger sizes were added later (Fig. 6.11).
Experience with sizes 1 and 6 is comparatively limited. It should be noted that, although originally developed from plaster casts of cadaveric adult larynxes, subsequent sizes are simply scaled versions of the originals. As infant and paediatric laryngeal anatomy varies considerably, the smallest sizes may not provide as reliable an airway as adult sizes. The manufacturer’s recommendations are as shown in Table 6.1. Where the predicted size does not fit well, an alternative size may provide a better airway.
The term LMA is a registered trademark of Intavent Ltd, UK.
cLMA dimensions relevant for its use as a conduit
The size of tracheal tube that can be passed through a given size of cLMA varies as tracheal tubes of the same internal diameter can have different external diameters depending on the model and manufacturer (Table 6.2).
Table 6.2 Size of tracheal tubes that can be passed through a cLMA. The tabulated results are for a lubricated Portex blue line uncuffed tracheal tube* passed without force in a cLMA. If using a cuffed tracheal tube, reduce the size of tube by 0.5 mm. The results do not apply to laryngeal masks other than the LMA Classic. Distances are to the mask grilles: intubation would require longer tracheal tubes. (*External diameter ranges from 1.3 to 2.6 mm greater than internal diameter (ID), increasing as internal diameter rises.)
| cLMA SIZE | SIZE OF UNCUFFED TT PASSABLE (mm ID) | DISTANCE FROM CONNECTOR TO MASK GRILLES (mm) |
|---|---|---|
| 1 | 3.5 | 108 |
| 1½ | 4.5 | 135 |
| 2 | 5.0 | 140 |
| 2½ | 6.0 | 170 |
| 3 | 6.5 | 200 |
| 4 | 6.5 | 205 |
| 5 | 7.0 | 230 |
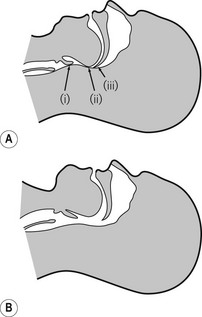
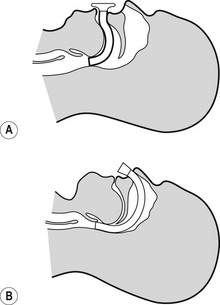
Inserting the LMA
Standard insertion
General anaesthesia should be adequate to allow generous mouth opening and jaw thrust without response. Under such circumstances there should be no need to use neuromuscular blockers. The patient’s head and neck are then placed in the ‘sniffing position’. The manufacturer’s recommended insertion technique requires that the cuff is deflated as above and the LMA is grasped like a pen in the dominant hand. The tip of the operator’s gloved index finger is placed at the junction of the tube and mask whilst the non-dominant hand maintains the position of the head and neck by cradling the occiput so that the patient’s mouth falls open. The mask is inserted into the mouth and the bowl is kept pressed against the hard palate as it is advanced in one smooth movement into the hypopharynx. The upward pressure against the palate flattens the cuff of the mask to give a smooth thin leading edge. The hard and then the soft palate and finally posterior pharyngeal wall act as a scoop to guide the mask into place and prevent snagging on the tongue or epiglottis. The mask is advanced until resistance is felt. For many people the index finger is not long enough to fully insert the LMA: the hand in the mouth, guiding the LMA, should remain in place while the hand on the occiput can now be used to push the LMA stem inwards (still guided by the hand in the mouth) until resistance is felt. The LMA is not fully inserted until it reaches resistance, signifying reaching the cricopharyngeal constrictor. Without holding the tube the cuff is then inflated with air. The manufacturer indicates a maximum volume for cuff inflation which must not be exceeded; inflation to an optimal pressure is preferable (see below). Use of the maximum volumes is likely to lead to excessively high intracuff pressures that reduce the device’s efficacy and safety profile. Where inflation to a predetermined volume is used, half the manufacturer’s recommended maximum is a good starting point.
Confirmation of correct placement
Remarkably, for a device that is inserted blindly, the mask almost always adopts the correct position and provides a patent airway with a success rate above 95%.16
Indications for using the LMA:
Instead of a facemask and pharyngeal airway, with the added benefit of:
1. releasing the anaesthetist’s hands to deal with other matters, and removing them from proximity to the operative site
2. providing a more reliable airway, particularly in patients placed in positions other than supine or where a facemask does not seal well against the face as in bearded patients.
Instead of a tracheal tube, in certain circumstances, for example:
1. elective procedures involving spontaneous or controlled ventilation, where tracheal intubation would have been used only to enable a ‘hands-free’ and gas-tight airway
2. elective procedures where intubation and the necessary drugs may elicit particularly undesirable cardiovascular or respiratory responses
3. patients in whom difficult intubation (but not difficult airway or mask ventilation) is predicted, as in those with cervical spine problems or moderately limited mouth opening, usually as a prelude to intubation via the LMA
4. as a first choice airway for use in emergencies by non-anaesthetic staff on the basis that success rate at establishing ventilation for non-specialist staff is greater with the LMA than with facemask ventilation or tracheal intubation.8
1. The LMA can be used as an aid to extubation and recovery, even after peroperative tracheal intubation. The LMA is less stimulating than a tracheal tube and less likely to elicit coughing and straining during recovery. It also protects the larynx from blood and secretions arising from the nasopharynx and oropharynx. An example of such use would be insertion of the LMA at the end of a tonsillectomy to facilitate a smooth wake-up. Placement of the LMA is much easier if the tracheal tube is at first left in place to guide insertion of the LMA. The device is advanced over the posterior aspect of the tracheal tube which ensures that the tongue and epiglottis are easily negotiated and the larynx may be held forward allowing the tip of the LMA to seat more easily behind the cricoid. The tracheal tube can then be removed.
For difficult airway management:
1. To provide a conduit to facilitate intubation. The LMA orifice lies directly over the laryngeal inlet in >90% of cases. In theory a gum elastic bougie or narrow long tracheal tube may be passed blindly through the LMA to enter the trachea; however, in practice, success rates are as low as 10–25% and such a ‘blind technique’ also risks trauma to a potentially already compromised airway. Far preferable are flexible endoscopic guided techniques, with use of an Aintree catheter being the best technique (described below).
2. To rescue the airway when intubation and/or facemask ventilation have failed. There is now considerable evidence to support the use of the LMA in these scenarios, some even suggesting that the LMA is more likely to be an effective airway in those in whom intubation has failed than it is in the general population. The device is consequently recommended in all international airway management algorithms.
1. There is considerable interest in use of SADs for maintenance of the airway during cardiopulmonary resuscitation. Several SADs are now recommended by the resuscitation councils. The largest bulk of evidence supports the use of the LMA, though several newer SADs that enable a higher pharyngeal seal may offer additional protection against regurgitation/aspiration and have potential benefits. The LMA may be used as a primary airway by those with little or no intubation skills and as a rescue device when tracheal intubation fails or is impractical because of patient entrapment. It may be easier for non-anaesthetists to achieve ventilation with a SAD than with a facemask.17
Contraindications
Accepted wisdom has it that the LMA does not protect the lungs against aspiration of refluxed or regurgitated gastric contents. In reality it offers some protection in the unconscious patient and therefore is ‘safer’ in this respect than facemask ventilation, with or without simple airway adjuncts.13,15 However, the LMA does provide less protection than the tracheal tube. The LMA should, therefore, not be used in patients with a full stomach or risk factors for regurgitation/aspiration (delayed gastric emptying, hiatus hernia, etc.).
LMA Flexible
The reinforced (or flexible) LMA (Intavent Direct, Maidenhead, UK) is an alternative version of the LMA in which the tube is thinner, narrower and longer and is reinforced with a spiral of steel wire to add flexibility and reduce the risk of kinking; it is available in sizes 2–5 (Fig. 6.12). Placement of the flexible LMA (fLMA) requires meticulous technique to prevent rotation leading to mask misplacement: the mask can rotate 180o about the axis of the airway tube, leaving the mask orifice facing backwards, without this being evident proximally. In performance terms the main difference between the fLMA and the classic LMA is that, once placed, its proximal tube can be moved in any direction without those movements being transmitted to the mask end of the device and leading to displacement. This makes the fLMA very popular for head and neck and intraoral procedures and enables the tube and breathing circuit to be positioned away from the operative site. Because the mask portion of the fLMA isolates the lower airway from above it is suitable for nasal and dental procedures. It may be used without a throat pack (therefore bypassing the risk of throat pack retention) though careful attention is required of both surgeon and anaesthetist to ensure surgical debris is not in the oral cavity during emergence. The fLMA is routinely used by a minority of anaesthetists for tonsillectomy where it can reduce the risk of blood entering the trachea during recovery from anaesthesia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree