The Anatomy of the Airway
The normal pediatric airway can be divided into supraglottic, glottic, and subglottic structures. Dividing the airway in this way allows us to consider the impact of pediatric airway development in a way that aligns with interventions and management.
The supraglottic structures include the elements of the upper airway: the tongue, palate, posterior pharyngeal space, and epiglottis. Supraglottic sensation is mediated by the superior laryngeal nerve.
The glottis is made up of the cartilages and muscular structures of the larynx. The larynx consists of nine cartilages, including the thyroid, cricoid, and epiglottis, and the corniculate, cuneiform, and arytenoid cartilages. These cartilages are covered by folds of mucosa, connective tissue, and muscle; laryngeal tissue folds define the glottis. The superior, inferior, and recurrent laryngeal nerves innervate the larynx. The recurrent laryngeal nerve provides most laryngeal motor innervation. Only the cricothyroid muscle is innervated by the superior laryngeal nerve.
The subglottis or infraglottis consists of the cricoid cartilage and the tracheal rings and mucosal surfaces of the upper trachea. This region also includes the trachea itself and the initial branches of the bronchial tree. Infraglottic sensation is mediated by the inferior laryngeal nerve. The airway is lined with ciliated and squamous epithelium that is highly vascular and overlies a rich network of lymphatic vessels.

Developmental Airway Considerations
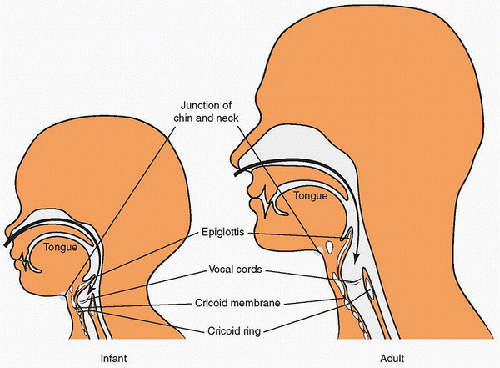
The anatomy of the pediatric airway differs from the adult airway until it reaches mature position at ~8-14 years of age. The major differences between pediatric and adult airway structures are size, shape, and position in the neck (
Fig. 24.1).
The infant’s tongue is large in proportion to the rest of the oral cavity and is closer to the palate; therefore, it can easily obstruct the airway. Laryngoscopic stabilization of the tongue may be more difficult in the infant and child than in the adult. The epiglottis is proportionally larger in the child than in the adult, and the ligamentous connection between the base of the tongue and the epiglottis (the hyoepiglottic ligament) is not as strong in the young child as in the adult. These differences can influence the selection of laryngoscope blade (straight vs. curved) for the intubation of young children (see discussion in the section Endotracheal Intubation— Intubation Procedure, later).
Tracheal diameter and length increase with age. Tracheal dimensions reported from postmortem examinations have been verified using magnetic resonance imaging (
MRI) (
1) (
Table 24.1). Because the diameter of the pediatric trachea is small, relatively minor compromise in tracheal radius can significantly increase resistance to airflow and work of breathing. Resistance to airflow is inversely related to the
fourth power of the radius during quiet breathing, when airflow is laminar, but is inversely related to the
fifth power of the radius when airflow is turbulent. When respiratory distress is present, providers should attempt to keep the child as quiet as possible to minimize agitation and to reduce turbulent flow, airway resistance, and work of breathing.
The glottic opening lies at approximately the level of cervical vertebrae C2 or C3 in the infant or child and at the level of C3 or C4 in the adolescent or adult. This position places the glottic opening of the infant or child at the base of the proportionally larger and predominantly intraoral tongue (
Fig. 24.1). This position of the pediatric glottis has been described as
anterior when compared to the mature laryngeal structures, because the airway may become hidden
by the tongue during laryngoscopy. The pediatric glottis is actually more
superior (i.e., higher or more cephalad) and more
anterior than in the adult airway. The larynx itself has an angulation, with the superior portion angled toward the provider. This can make it difficult to pass an endotracheal tube (
ETT), particularly during nasal intubation.
MRI studies in children document anterior angulation (nearly 10 degrees from the vertical) at approximately the level of the sternal notch (
1).
On the basis of cadaver studies, it has long been accepted that the child’s larynx is cylindrical from side to side but conical in the transverse or anterior-posterior dimension, with the
tip of the cone at the level of the cricoid cartilage. Pediatric studies using
MRI have confirmed this conical shape. In these studies of anesthetized, spontaneously breathing children, the smallest transverse diameter of the larynx was at and immediately below the level of the vocal cords, rather than at the cricoid cartilage (
2). However, because the vocal cords and subglottic tissues can be distended, the rigid cricoid ring is still the smallest functional part of the infant airway (
2). As the child grows to adulthood, the larynx becomes more cylindrical in shape, with the narrowest segment at the level of the vocal cords (see
Fig. 24.1,
Table 24.2).
The child’s subglottic airway is smaller and more compliant, and the supporting cartilage is less well developed than in the adult. As a result, upper airway obstruction (e.g., caused by croup, epiglottitis, or extrathoracic foreign body) can produce tracheal collapse and stridor. Although most of the child’s laryngeal mucosa is loosely connected to the underlying tissues, it is tightly connected in the area of the vocal cords and at the laryngeal surface of the epiglottis. Subglottic inflammation is typically contained below this level; however, with little room to accommodate even modest inflammation at the level of the vocal cords or epiglottis, such inflammation can lead to a gross distortion of tissue planes and anatomy and to airway obstruction.
These anatomic variations have long been thought to cause difficulty in intubating the child, requiring more expertise than intubating the adult. More recent evidence suggests that the general incidence of difficult laryngoscopy in children (0.58%-3%) is lower than that reported in adults (9%-13%). In a recent report of 8434 children intubated for 11,219 procedures, Heinrich et al. (
3) found an overall incidence of difficult intubation in 1.35% of all children, with the risk highest in neonates (3.2%) and infants (5%). They also found a correlation with severity of presenting illness, with difficult intubation reported in 3.8% of the sickest children (compared with 0.8% of the children who were less ill). Although the incidence of difficulty intubating children in general may be low, children with significant illness, such as those presenting in an
ICU are more likely to be difficult to intubate. It should also be noted that the above study looked at experienced practitioners in pediatric anesthetic practice. Other work has shown a high (50%) failure rate on first intubation attempt among pediatric residents (
4) and fellows intubating neonates (
5).
Selection of
ETT size can be challenging, and precise selection is extremely important. If the
ETT is too large, it can cause subglottic pressure ischemia and necrosis, leading to subglottic stenosis. If the
ETT is too small, it provides significant resistance to air flow and typically is associated with a large air leak that may complicate support of ventilation.
Oral intubation with direct laryngoscopy requires the establishment of a line of vision from the mouth and teeth to the vocal cords (i.e., the glottic opening). This line of vision requires the alignment of three axes: the oral, pharyngeal, and laryngeal. Normally, the laryngeal axis is perpendicular to the oral axis and forms a 45-degree angle with the pharyngeal axis. The provider must position the patient to align these axes for optimal airway patency and for successful intubation.
 To provide successful and safe airway management, providers must have an appreciation of the unique developmental anatomy and physiology of the child’s airway.
To provide successful and safe airway management, providers must have an appreciation of the unique developmental anatomy and physiology of the child’s airway. Successful acute airway management requires that providers anticipate the development of a difficult airway and have a primary and secondary plan for management.
Successful acute airway management requires that providers anticipate the development of a difficult airway and have a primary and secondary plan for management. The difficult pediatric airway is best managed not by heroic intervention and uncommonly used techniques but, rather, by anticipation and planning, careful patient positioning, effective bag-mask ventilation, and advanced airway insertion, as needed.
The difficult pediatric airway is best managed not by heroic intervention and uncommonly used techniques but, rather, by anticipation and planning, careful patient positioning, effective bag-mask ventilation, and advanced airway insertion, as needed. Successful airway support requires careful choice of equipment (type and size), appreciation of the pathology requiring intubation, and presence of personnel with the requisite skills.
Successful airway support requires careful choice of equipment (type and size), appreciation of the pathology requiring intubation, and presence of personnel with the requisite skills.