Chapter 8 Airway Management
Assessment
Airway Emergencies
Soft Tissue Swelling or Edema in the Airway
Allergic Reaction
An allergic reaction is a hypersensitive response by the immune system from exposure to a previous antigen. The initial antigen exposure causes the immune system to develop antibodies that are activated with subsequent exposures. Reactions may range from mild to severe. The most severe reaction, anaphylaxis, occurs suddenly causing complete airway obstruction. Significant airway swelling requires immediate airway management. Anaphylaxis can lead to anaphylactic shock (see Chapter 20, Shock, for more information).
Therapeutic Interventions
• If patient is alert, allow position of comfort optimizing good air exchange.
• Administer high flow oxygen (O2).
• Establish intravenous access.
• Continuously monitor cardiac rhythm and oxygen saturation.
• Obtain emergency airway equipment including cricothyrotomy tray.
• Prepare for early endotracheal intubation; do not delay if symptoms are severe.
• Anticipate administration of the following:
Infectious Process or Mass
Therapeutic Interventions
• Allow patient to assume a position of comfort.
• Provide supplemental oxygen by any means the patient will tolerate.
• Establish intravenous access.
• Continuously monitor cardiac rhythm and oxygen saturation.
• Obtain emergency airway equipment including cricothyrotomy tray.
• Anticipate administration of corticosteroids and antibiotics.
Angioedema
Therapeutic Interventions
• Provide supplemental oxygen by any means the patient will tolerate.
• Establish intravenous access.
• Continuously monitor cardiac rhythm and oxygen saturation.
• Obtain emergency airway equipment including cricothyrotomy tray.
• Prepare for early endotracheal intubation; do not delay if symptoms are severe.
• Proceed to surgical airway management if intubation is not possible.
• Consider administration of fresh frozen plasma for hereditary angioedema.
Foreign Body Aspiration
Therapeutic Interventions
• Rapidly assess airway for patency and spontaneous breathing.
• Facilitate emergent endotracheal intubation in the unconscious, nonbreathing patient.
If the patient is not moving air:
• Perform abdominal thrusts (chest thrusts in infants) to attempt to remove the object.
• Direct visualization of the upper airway with a laryngoscope may facilitate observation and removal of the foreign object.
• If unable to remove object, attempt oral intubation. If unable to intubate, immediately proceed to surgical airway.
• Encourage coughing, leaning forward to facilitate expulsion of object.
• Remove any objects visible in the mouth (with fingers, suction, or Magill forceps). Do not perform a blind finger sweep.
• Provide supplemental oxygen by any means the patient will tolerate.
• Continuously monitor cardiac rhythm and oxygen saturation.
• Obtain emergency airway equipment including cricothyrotomy tray.
• Chest and soft tissue lateral neck radiographs can be used to localize objects but should never delay care.
Airway Management
Common Airway Adjuncts
Oxygen
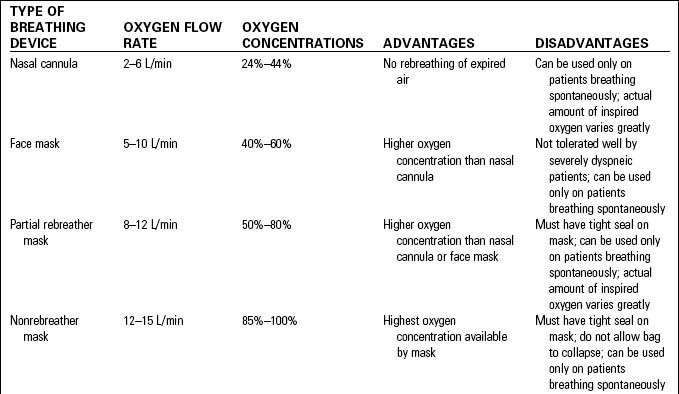
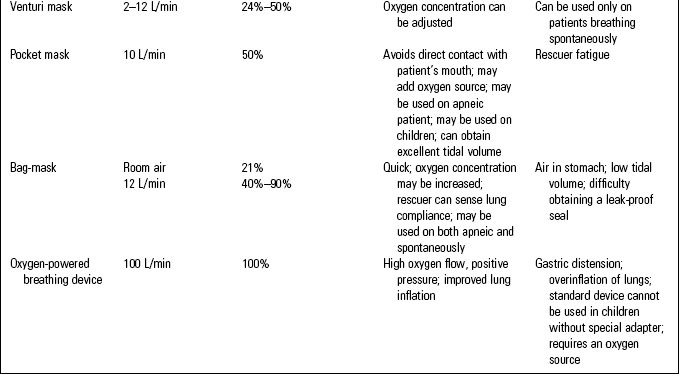
Oxygen administration is a fundamental therapy used to treat many conditions. Oxygen therapy can be administered by a variety of methods delivering low to high concentrations. Potential side effects include dryness of the airways and irritation of the nose, face, or ears from the delivery device. Table 8-1 summarizes common oxygen therapy devices.
Oropharyngeal Airways
• An oropharyngeal airway (OPA) is a curved plastic device that is inserted over the tongue into the posterior pharynx.
• The OPA is used to prevent the tongue or epiglottis from falling back against the posterior pharynx and occluding the airway in an unconscious or heavily sedated patient.
• Oral airways facilitate suctioning of the pharynx and prevent patients from biting their tongues or grinding their teeth. In the intubated patient the OPA can also serve as a bite block to prevent biting on the endotracheal tube
• This device should not be used in patients with an intact gag reflex. It may induce gagging and possible aspiration.
• The OPA comes in a variety of sizes. To select the correct size, measure from the corner of the patient’s mouth to the tip of the earlobe. Be sure the correct size is used.
• If the device is too short, it will push the tongue back and occlude the airway. If the device is too long, it may stimulate gagging and emesis.
• There are two methods used for insertion. First, insert the device upside down (curved side up) until the soft pallet is reached, then rotate the device 180° and advance over the tongue. Do not use this method in children.
• Another method is to use a tongue blade to depress the tongue and insert the device (curved side down) into the posterior pharyngeal area.
• When correctly inserted the plastic flange should rest against the outer surface of the patient’s teeth.
Nasopharyngeal Airway
• Nasopharyngeal airways (NPA, nasal trumpet) are made of soft semirigid rubber and are inserted through a nonobstructed nostril to provide air passage between the nose and nasopharynx.
• This device is preferred for conscious patients because it is better tolerated and less likely to produce a gag reflex.
• Select a size that extends from the nares to the tragus of the ear. If the device is too long, the tip can stimulate laryngospasm.
• Be sure the NPA is well lubricated with a water soluble lubricant or topical anesthetic (lidocaine jelly 2%).
• Insert it into the nostril with the bevel toward the septum and advance into the posterior pharyngeal area.
• The NPA can also be useful for endotracheal suctioning in the nonintubated patient and can improve ventilation when used in conjunction with bag mask ventilation.
• Complications may include epistaxis, laryngospasm, or vomiting.
• The NPA is contraindicated in patients who are anticoagulated, have confirmed or suspected facial or basilar skull fractures, or have nasal deformities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree