
Airway Management
Tarlan Hedayati and Michael F. Murphy
Airway evaluation and management to ensure continuing and adequate gas exchange remain the first priority of resuscitation, taking precedence over other interventions. Further, it is widely recognized that a conceptual framework focused on rapid airway evaluation, critical action analysis and performance, and facility with an array of airway management techniques minimizes the risk of failure and improves outcome (1).
The failure to maintain a patent airway and the failure to affect adequate gas exchange are the cornerstones of emergency airway management. Decisions regarding how and when the airway will be managed depend on the integration of numerous factors including the skills and knowledge of the physician, the equipment available, the condition of the patient, and the anatomy of the airway.
There are only four ways to provide gas exchange for the patient who is not breathing:
1. Bag–mask ventilation (BMV)
2. Extraglottic device (EGD)
3. Endotracheal intubation (ETI)
4. Surgical airway (usually cricothyrotomy in emergency medicine)
Emergency ETI performed by emergency physicians has been the most discussed, researched, and published over the years (2).
By the early 1970s, ETI had become a skill integral to the practice of emergency medicine. It was generally accomplished either nasally or orally employing varying degrees of brute force. By the mid to late 1990s, most emergency practitioners employed neuromuscular blockade in some form most of the time to facilitate oral ETI. It had become evident that neuromuscular blockade not only made the technical task of intubation easier and faster but that the complication rates were lower and the success rates higher. However, for many practitioners, the need to evaluate the airway for difficulty and the development of a systematic method of doing so lagged behind the clinical introduction of rapid sequence intubation (RSI). There was also the need to expand the rescue options beyond cricothyrotomy.
BMV, long considered to be the cornerstone of airway management (Chapter 2), is a critically important skill in emergency medicine. However, it has become apparent that BMV is a difficult skill to teach and maintain (3). In recent years, EGDs (e.g., laryngeal mask airways [LMA], King LT Airway), which are easily inserted and highly successful at achieving adequate gas exchange, have increasingly emerged as potential first-line gas exchange techniques.
The current challenges facing emergency airway managers include the following:
• Should EGDs supplant BMV as the first-line airway management technique?
• Which patients should not receive paralytics?
• Is cricoid pressure still recommended to prevent passive regurgitation and aspiration of gastric contents?
• How is the airway best rescued in the event intubation and/or ventilation is impossible or has failed?
THE DECISION TO INTUBATE
The following are the five generally accepted indications to secure an airway by ETI in emergency medicine practice:
1. Failure of the patient to maintain a patent airway
2. Failure of the patient to adequately protect the airway from aspiration
3. Failure of the patient to maintain adequate gas exchange (oxygen and carbon dioxide)
4. Need for the initiation of paralytic agents or therapeutic hyperventilation
5. Inability of the patient to adequately clear secretions
A sixth indication that is frequently invoked is intubation prior to transport, when it is reasonably anticipated that although an indication to intubate does not exist now, one may develop during the transport. This risk-to-benefit analysis recognizes the practicalities and challenges of intubating in a transport vehicle.
There are probably few other situations in emergency practice when judgment and knowledge of the anticipated clinical course of a disorder are as crucial to the emergency physician as the decision to intubate a patient (4).
EVALUATION OF THE PATIENT
Human beings protect their airway at all costs, triggering an extreme autonomic response when threatened. ETI stimulates a similar autonomic response. As such, potent medications are generally employed to attenuate the adverse responses to laryngoscopy and intubation such as hypertension, tachycardia, increased intracranial pressure (ICP), and bronchospasm. The emergency physician must attempt to balance the anticipated aggression of the response to intubation by selecting appropriate classes and dosages of medication to mitigate them. Underdosing may fail to mitigate an aggressive response; overdosing may produce hypotension or premature apnea.
The evaluation of the patient to be intubated is focused on the three crucial organ systems: The central nervous system (CNS), the cardiovascular system, and the respiratory system. The patient’s hemodynamic stability, physiologic reserve of vital organ systems, and the anticipated response to laryngoscopy and intubation dictate which medications and what doses are required to maintain stability and mitigate adverse effects during the procedure.
EVALUATION OF THE AIRWAY
Airways that are difficult to manage are fairly common in emergency medicine with some estimates being as great as 20% of all emergency intubations. However, the incidence of intubation failure is quite uncommon (0.5% to 2.5%). Moreover, the disastrous situation of being able to neither intubate nor ventilate rarely occurs (0.1% to 0.5%) (2).
The most important way to avoid airway management failure is to predict when difficulty is likely to be encountered with BMV, ETI, EGD, or cricothyrotomy, particularly if one is relying on the latter two techniques to rescue the airway in the event of ETI or BMV failure.
The distinction among the terms difficult laryngoscopy, difficult ETI, difficult BMV, difficult EGD, difficult cricothyrotomy, and difficult airway is important. For instance, difficulty with BMV or an EGD when ETI is easily performed would not be described as a difficult airway. Rather, the narrative would describe each independently.
The failed airway is clearly defined as three failed attempts at intubation and/or failure to maintain oxygen saturations. The difficult airway is not so easily defined. Rather than a strict definition, the concept of the difficult airway has the following five “dimensions.”
1. Difficult BMV
2. Difficult laryngoscopy
3. Difficult intubation
4. Difficult EGD
5. Difficult cricothyrotomy
These five dimensions can be reduced to the following four technical operations:
1. Difficult BMV
2. Difficult EGD
3. Difficult laryngoscopy and intubation
4. Difficult cricothyrotomy
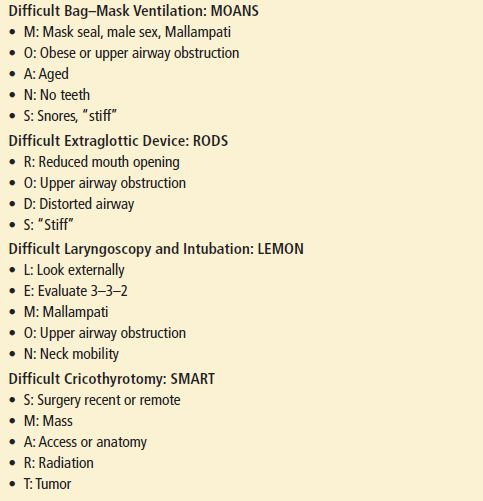
The evaluation of the airway for difficulty in an emergency must be done quickly, with care taken not to omit anything important. Mnemonics are efficient memory aid strategies, so one for each technical operation has been crafted to permit a rapid and complete evaluation (Table 1.1).
TABLE 1.1
Mnemonics Useful in Evaluating the Airway for Difficulty
Difficult Bag–Mask Ventilation
If the emergency physician is uncertain that neuromuscular blockade-facilitated orotracheal intubation (RSI) will be successful, he or she must be confident that BMV or EGD-facilitated ventilation is possible or at the very least that a cricothyrotomy can be performed rapidly.
The five indicators of difficult BMV (5,6) can be easily recalled for rapid use in the emergency setting by using the mnemonic MOANS (Table 1.1) (7).
• Mask seal, Male sex, Mallampati. Bushy beards, crusted blood on the face, or a disruption of lower facial continuity are the most common examples of conditions that may make an adequate mask seal difficult. Male sex and Mallampati scores of 3 or 4 have also been associated with difficult mask ventilation.
• Obese or obstructed. Patients who are obese (body mass index [BMI] >26 to 28 kg/m2) are often difficult to ventilate adequately by bag and mask. Parturients at term; patients with angioedema, Ludwig angina, upper airway abscesses (e.g., peritonsillar), or epiglottitis; and others ought to be considered at this juncture.
• Advanced age. Patient age older than 55 to 57 years is associated with a higher risk of difficult BMV, perhaps because of a loss of muscle and tissue tone in the upper airway with age.
• No teeth. An adequate mask seal may be difficult in the edentulous patient, perioral tissues tend to cave into the structurally unsupported mouth.
• Stiff or snores. Patients with high airway resistance or diminished pulmonary compliance are exceedingly difficult to adequately manage with a bag and mask, as are patients who snore.
Difficult Extraglottic Devices
Four factors may indicate that EGDs may be unsuccessful at rescuing the airway and may be remembered using the RODS mnemonic (Table 1.1) (8):
• Restricted mouth opening. Depending on the EGD to be employed, a certain amount of oral access is critical to employ the device.
• Obstruction. Upper airway obstruction at the level of the larynx or lower will not be bypassed through the use of an EGD.
• Disrupted or distorted anatomy. The “seat and seal” of the EGD may be compromised by a disrupted or distorted airway. In addition, a seal may be exceedingly difficult or impossible to achieve in the face of a fixed flexion deformity of the neck (9).
• Stiff lungs or cervical spine. Ventilation with an EGD may be difficult or impossible in the face of substantial increases in airway resistance (e.g., severe asthma) or decreases in pulmonary compliance (e.g., pulmonary edema). In addition, patients unable to fully extend the neck may prove to be difficult to ventilate with EGDs due to improper positioning of the EGD.
Difficult Laryngoscopy and Intubation
Difficult laryngoscopy and intubation ordinarily implies that the operator had a poor view of the glottis. Cormack and Lehane (10) provided some clarity to the way physicians think of the “difficult airway” by parsing the act of intubation into its two subcomponents: Laryngoscopy and intubation. They also introduced the most widely used system of categorizing the degree of visualization of the larynx during laryngoscopy (Fig. 1.1) (7). Cormack–Lehane view grades 3 (epiglottis only visible) and 4 (no glottic structures at all visible) are often used as surrogates to represent difficult laryngoscopy and to predict difficult intubation. View grades 1 (visualization of the entire laryngeal aperture) and 2 (visualization of the posterior cords and arytenoids) are not typically associated with difficult intubation, although some grade 2’s may be very anterior and difficult or impossible to intubate.
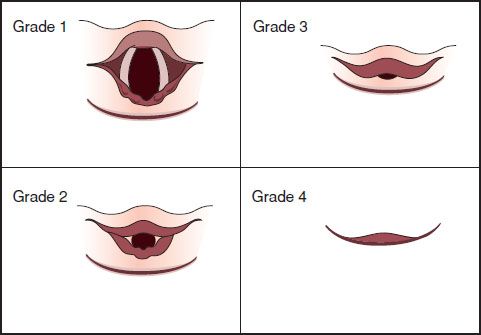
FIGURE 1.1 Cormack and Lehane system of categorizing the degree of visualization of the larynx during laryngoscopy.
The mnemonic LEMON (Table 1.1) is a useful guide to identifying as many of the risks as quickly as possible to meet the demands of an emergency situation.
• Look externally. If the airway looks difficult, it probably is! A litany of physical features is associated with difficult laryngoscopy and intubation, making the glottic aperture difficult to visualize. A small mandible may indicate that the tongue is “retrofitted” over the larynx; a large mandible elongates the pharyngeal axis, serving to extend the distance to the larynx beyond the visible horizon. Buck teeth block access to the oral cavity and also elongate the length of the oral axis. A high, arched palate is often associated with a long narrow oral cavity, making access a problem. A short neck may mean the larynx is positioned higher in the neck relative to the base of the tongue, making it more difficult to bring the glottis into view. Lower facial disruption interferes with adequate mask seal and may make the glottis impossible to find.
• Evaluate 3–3–2. This step recognizes the importance of the geometric relationships of various parts of the airway to successful intubation (11). One ought to be able to open one’s mouth with the width of three of their own fingers, accommodate three of their own fingers between the tip of the mentum and the hyoid bone, and fit two fingers between the hyoid bone and the thyroid notch. The first “three” assesses the adequacy of oral access. The second “three” addresses the capacity of the mandibular space to accommodate the tongue on laryngoscopy. More than or less than three fingers are both associated with greater degrees of difficulty in visualizing the larynx at laryngoscopy. The former because the length of the oral axis is elongated; the latter because the mandibular space may be too small to accommodate the tongue, leaving it to obscure the view of the glottis. The final “two” identifies the location of the larynx in relation to the base of the tongue. If more than two fingers are accommodated, the larynx is further below the base of the tongue beyond the visible horizon. Fewer than two fingers may mean that the larynx is tucked up under the base of the tongue and may be difficult to expose. This condition is often called anterior larynx.
• Mallampati score. Mallampati determined that the degree to which the posterior oropharyngeal structures are visible is loosely associated with intubation success (12). He had patients sit on the side of the bed, open their mouths as widely as possible, and protrude their tongues as far as possible, without phonating. Figure 1.2 depicts how the scale is constructed. Although classes I and II patients are associated with low intubation failure rates, the importance with respect to the wisdom of using neuromuscular blockade rests with those patients in classes III and IV, particularly those in class IV where intubation failure rates may exceed 10%. By itself, the scale is neither sensitive nor specific; however, it is easily performed in an emergency and may reveal important information about access to the oral cavity and the potential for difficult glottic visualization.
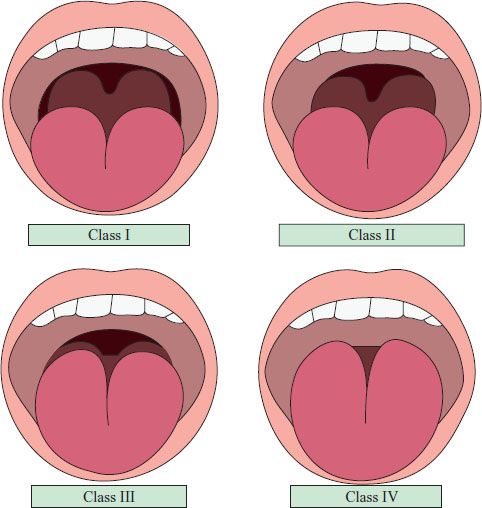
FIGURE 1.2 Mallampati score.









