AIRWAY
AARON DONOGHUE, MD, MSCE, JOSHUA NAGLER, MD, MHPEd, AND LOREN G. YAMAMOTO, MD, MPH, MBA
GOALS OF EMERGENCY THERAPY
Tracheal intubation (TI) is a fundamental procedure during resuscitation of a critically ill child. The goals of therapy are the placement of an artificial airway in the trachea in a safe, expedient fashion, while simultaneously avoiding physiologic deterioration (hypoxia, hypercapnia, bradycardia, hypotension).
TI is indicated for any clinical state where existing or impending failure exists of oxygenation, ventilation, neuromuscular respiratory drive, or airway protective reflexes. Reports in pediatrics have shown that the most frequent indications for TI in children involve neurologic failure (traumatic brain injury, cardiac arrest, status epilepticus) as opposed to primary respiratory failure, with trauma accounting for more than half of all cases of pediatric TI in the ED. TI should be considered the definitive method of managing existing or impending respiratory failure from any cause in the ED (see Chapter 4 Cardiopulmonary Resuscitation).
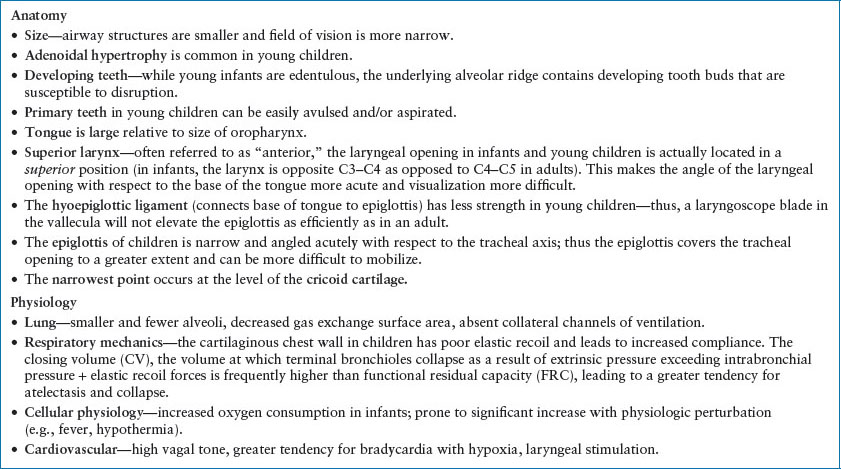
Pediatric anatomy and physiology has direct influence on intubation technique, equipment selection, and prevalence of adverse physiologic events during TI. Table 3.1 summarizes the anatomic and physiologic features in children that are important to consider when approaching TI in a child. The summary effects of the various respiratory physiologic phenomena described above are a greater tendency for hypoxemia and arterial desaturation, which must be kept in mind during the preintubation and intubation phases of the procedure.
Quality and Safety
Despite the fact that TI is a fundamental, essential skill for emergency providers, pediatric TI is an uncommon occurrence when measured at the level of an individual provider. A recent survey of pediatric ED directors found that the annual incidence of TI in the PED ranged from 12 to 64 cases per year. Sixty-two percent of surveyed PED directors believed that their faculty did not encounter sufficient exposure to TI in their clinical duties to maintain competence at this essential procedure. Additionally, the same survey found that there was a negligible difference in the median number of TI cases per faculty at the PEDs where their directors thought exposure was insufficient (five cases per faculty per year) and those where their directors thought exposure was sufficient (seven cases per faculty per year). Data from tertiary PEDs published in the past few years has shown low-frequency exposure to TI for PED faculty, with fewer than half of PED faculty performing TI during a year of typical clinical experience, and supervising TI performance a median of four times per year.
Published data on exposure to pediatric TI among trainees in pediatrics and pediatric EM also shows scant—and possibly diminishing—experience. Multiple studies have shown that pediatric residents are exposed to opportunities for attempting TI less often. A study of video recorded TI attempts from a tertiary PED demonstrated success rates of 33% for residents and 50% for PEM fellows. Multihospital registry data on pediatric TI in the ICU has shown a significant positive association between residents attempting TI and the occurrence of adverse events. In 2013, the Accreditation Council for Graduate Medical Education removed nonneonatal TI from the core competencies for housestaff training in pediatrics.
Finally, while historically reported as uncommon, physiologic deterioration during intubation may be more common than previously appreciated in children. In the previously mentioned study of video recorded cases of pediatric emergency intubation, oxyhemoglobin desaturation (defined as pulse oximetry of <90%) has been shown to occur in up to one-third of cases of emergency TI in the PED. Cardiovascular instability (bradycardia, hypotension) have been noted to occur in up to 8% of patients, with cardiac arrest from asphyxia occurring in 2%. This combination of high clinical risk, infrequent occurrence, and dwindling exposure among trainees has led to widespread reconsideration of what operators are appropriate to perform TI in the PED. Careful attention should be paid to training exposure and cumulative clinical experience among personnel in the PED who may be required to perform TI on children.
Bridging the gap between the infrequent nature of TI and the need for ongoing skill maintenance is a challenge to be met as PEM moves forward. Multiple novel approaches to this challenge have been reported in published literature. The use of retrospective review of TI data from individual centers and multicenter databases, both from medical records and from video-recorded patient encounters, has been reported as a technique to identify areas for improvement. Simulation education is well suited to this uncommon, high-stakes procedure; data on the effectiveness of simulation in educational and affective outcomes (e.g., learner satisfaction) have been promising, but additional research is necessary to determine the optimal means of using simulation to improve clinical outcomes in the PED during TI.
EQUIPMENT
Anticipating the need for increasing airway support and having necessary advanced airway equipment available is critical. An oxygen supply source, devices for passive oxygen delivery, and a bag-valve-mask device are needed for preparation as well as during advanced airway management procedures. Adjunctive devices such as oral and nasal airways should be available. Equipment in a range of sizes suitable for children from birth to adolescence should be available. Monitoring equipment including capnography should be available. For advanced airway management, additional equipment should include endotracheal (ET) tubes, stylets, and traditional laryngoscope blades and handles and/or an indirect or videolaryngoscope.
TABLE 3.1
ANATOMIC AND PHYSIOLOGIC FEATURES IN CHILDREN PERTINENT TO LARYNGOSCOPY AND INTUBATION
Endotracheal Tubes
Both cuffed and uncuffed ET tubes are available for use in pediatrics. Historically, uncuffed tubes were preferentially used in young children to allow use of the maximal tube size that would be accommodated by the anatomic narrowing at the level of the subglottis. More recent bronchoscopic and radiologic data suggest that the pediatric airway may be more elliptically shaped at this level rather than circumferentially narrowed. In addition, newly designed cuffed pediatric ET tubes are manufactured with balloons that are low profile and moved distally on the tube to avoid laryngeal structures when appropriately positioned. Use of these new cuffed tubes has been shown to decrease the need for tube exchange secondary to inappropriate sizing, with no increase in postextubation stridor, need for racemic epinephrine, or long-term complications. Pediatric Advanced Life Support Guidelines as well as anesthesia literature now supports that, beyond the newborn period, cuffed ET tubes are equally as safe as uncuffed tubes. In addition, cuffed tubes are favored in clinical circumstances where airway diameter may change over the course of treatment (e.g., inhalational injury, angioedema), as a protective measure for children at risk for aspiration, and in any child in whom underlying lung disease may necessitate high ventilator pressures (e.g., bronchiolitis, status asthmaticus, chronic lung disease). The risk associated with the use of cuffed ET tubes is inadvertent excessive cuff pressures, which could lead to ischemia of the tracheal mucosa. Various recommendations suggest that pressures higher than 20 to 30 cm H2O should be avoided. This can be achieved either through listening for an air leak while applying positive pressure through the ET tube, or by using an ET tube cuff manometer.
ET tube sizes are reported based on the internal diameter, measured in millimeters (mm). Available sizes range from 2.5 mm (suitable for a preterm infant) to adult sizes of 7.0 mm or more. Resistance to airflow as well as risk of tube obstruction are both increased in smaller tubes. Tube selection in pediatrics therefore aims to balance these risks associated with smaller tubes, with the need to select a tube that will pass easily through the vocal cords and not create excessive pressure on the tracheal wall. Methods of selecting the appropriate tube size include use of a length-based resuscitation tape, pediatric sizing programs available online or on mobile devices, and use of an age-based formula. Each has been shown to be effective, though inclusion of options for cuffed tube sizing is not offered in each. For uncuffed ET tube sizing, the age-based formula: 4 + (age in years/4) has been shown to be accurate in children. For newer, low profile cuffed ET tubes, selecting a tube one-half size smaller is recommended. Thus, for cuffed tubes, the formula is 3.5 + (age in years/4). Regardless of the method chosen in selecting the initial tube size, it is important to have additional tubes available, one size smaller in the event that tube passage is difficult and one size larger if a large air leak results in inadequate ventilation, despite inflation of the cuff where appropriate.
ET tube stylets provide rigidity and shape to the ET tube, offering facility in guiding the tube through the glottic opening. Various sizes exist to accommodate both pediatric- and adult-sized ET tubes. Most stylets are manufactured with a friction reducing surface coating, however water-soluble lubricant can be utilized to facilitate passage as needed. The stylet should not project past the tip of the tube or through the Murphy eye. Bending the stylet over the adapter at the proximal end of the tube prevents inadvertent movement during intubation.
Direct Laryngoscopes
There are two components to traditional direct laryngoscopes, the handle and the blade. Pediatric- and adult-sized handles are available that differ in diameter and length. Smaller diameter handles tend to be favored with smaller blades, though selection is ultimately based on operator’s preference. Laryngoscope blades are either curved or straight. The choice of curved or straight blade is best made based on the experience and preference of the operator. Curved blades are designed to follow the base of the tongue into the vallecula. They often have a beaded tip to allow pressure against the hyoepiglottic ligament which helps elevate the epiglottis. They also have a large flange which facilitates displacement of the tongue. Straight blades allow direct lifting of the epiglottis to expose the glottic opening. This type of blade may be preferred in infants and younger children in whom the epiglottis is often larger and more likely to fall into the line of sight.
Selecting the appropriate laryngoscope blades size allows the operator to control the tongue and reach the glottic structures. A number of approaches can be used to select the appropriate sized equipment for airway management. Resources include age-based guidelines, length-based resuscitation tapes, anatomic landmarks, and electronic applications. Although size 00 and 0 blades are used in neonatology, blades smaller than size 1 are rarely required in emergency medicine. Size 1 blades can be used in patients less than 2 years of age. Size 2 blades are commonly used in children starting at 2 years of age. Size 3 blades are commonly used beginning around 10 to 12 years of age. Selecting a laryngoscope blade that approximates the distance between the upper incisors and the angle of the mandible can be used as a guide in patients whose age is not known or when the anatomy appears incongruous with proposed blade size based on other available references.
Videolaryngoscopy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








