Chapter 49
Advanced Cardiac Life Support (ACLS) and Therapeutic Hypothermia
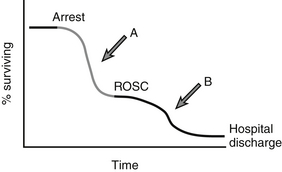
Sudden cardiac arrest (SCA) is defined as the immediate cessation of mechanical cardiac function and the concomitant global loss of blood flow. SCA is a leading cause of death in the United States with approximately 300,000 Americans succumbing to SCA each year. Advanced Cardiac Life Support (ACLS) represents a set of highly time-sensitive therapeutic maneuvers used to support and ultimately restore circulation (see Figure 49.1 for overview of the SCA survival time line). ACLS includes cardiopulmonary resuscitation (CPR), endotracheal intubation, electrical defibrillation for appropriate cardiac rhythms, and the use of specific pharmacologic interventions. ACLS algorithms (see Appendix D for ACLS algorithms) are widely used during both in-hospital SCA (by trained nurses and physicians) and out-of-hospital SCA (by ambulance personnel). ACLS certification is required for a large number of health care providers.
A multisite study from 2008 evaluating cardiac arrest survival outcomes revealed a wide range of survival to hospital discharge rates in the United States, from 3% to 16% with an overall 8% survival for out-of-hospital cardiac arrest. Survival from in-hospital cardiac arrest is somewhat higher, with a large registry study documenting 18% survival to hospital discharge. Since the development and implementation of rapid response teams (RRTs; also known as medical emergency teams or METs [see Chapter 110]) to respond to impending arrest events in the hospital, the demographics of in-hospital cardiac arrest has shifted, with fewer SCA events on the general wards and more events taking place in intensive care units (ICUs). The overall impact of RRTs on SCA survival, however, remains controversial and a topic of ongoing investigation.
Although the sequence of actions required in ACLS had been generally considered complete once a patient had regained a pulse, the introduction of a powerful post-resuscitation treatment option, therapeutic hypothermia (TH), has broadened the scope of resuscitation care. TH, the intentional lowering of core body temperature after initial resuscitation, has been shown to improve both survival and neurologic outcomes following SCA. This chapter provides an overview of cardiac arrest resuscitation care as well as important aspects of post-resuscitation care including TH. Although reference will be made to the ACLS protocols and guidelines established by the American Heart Association (AHA), they will not be restated here. Clinicians should consult ACLS manuals and AHA reference materials for specific protocol information (see Appendix D for 2010 ACLS algorithms).
Cardiopulmonary Resuscitation
A crucial first step to restoring circulation is the immediate performance of cardiopulmonary resuscitation (CPR), a technique that took its modern form in the 1960s. Promptly delivered CPR, performed correctly and effectively, can increase the chances of survival two- to threefold. Consensus resuscitation guidelines promulgated by the AHA recommend chest compressions at a rate of 100 per minute and ventilations, using mouth-to-mouth or bag-valve-mask technique, with approximately 8 to 10 breaths per minute. The AHA recommends “pushing hard and fast,” with compression depth of 1.5 to 2 inches of chest deflection in adults, ensuring full chest recoil and minimizing interruptions in chest compressions (see Table 49.1 for key aspects of correct CPR performance). Recommendations for basic life support (BLS) care changed in 2005, from compression-to-ventilation cycles of 15:2 to the currently recommended 30:2 for adult patients, in order to circulate as much oxygenated blood to vital organs as possible. It is estimated that CPR only generates 20% to 30% of normal cardiac output, and blood flow depends greatly on the quality of this intervention. For every minute CPR is not performed after the heart has stopped, the chances of survival decrease approximately 10% to 15%.
TABLE 49.1
Cardiopulmonary Resuscitation Quality Parameters
| Parameter | Guideline |
| Ventilation rate (intubated) | 8–10 breaths per minute |
| Compression to ventilation ratio (nonintubated) | 30:2 CCs to breaths |
| Compression rate | 100 CCs per minute |
| Compression depth | 1.5–2 inches for each CC |
| Release/recoil | Full release from chest after CC |
| Pauses | Minimize all pauses |
Monitoring the Quality of CPR
Although CPR seems simple to perform, both in-hospital and out-of-hospital investigations have shown that incorrectly or suboptimally performed CPR is common in actual practice and can compromise patient survival. One study found that rescuers’ chest compression rates were less than 90 per minute 28% of the time, compression depth was too shallow in 61% of compressions, and ventilation rates were often too high. A number of studies have shown that defibrillation efficacy and successful restoration of a pulse are sensitive to compression rate and depth. Additionally, an out-of-hospital investigation showed that hyperventilation during CPR may significantly decrease survival. To address these major discrepancies in cardiac arrest care, a variety of devices have been developed with a goal of improving CPR quality by providing rescuers with immediate audio or visual feedback on CPR performance. These devices are either freestanding or incorporated into standard defibrillators; they have a “pad” or “puck,” which is outfitted with an accelerometer and force detector. The rescuers perform CPR through these sensing pads, placed on the chest of the patient in the same place rescuers normally put their hands for CPR. Another modality used to improve CPR quality has been simple metronome devices—for example, a ventilatory-assist device currently in use flashes an indicator light at a rate of 10 per minute, prompting appropriate ventilation rates by rescuers.
Defibrillation
Automatic external defibrillators (AEDs) are commonly found installed in airports or other public settings and have been shown to dramatically improve survival from out-of-hospital cardiac arrest. Although often successful when administered promptly and correctly, defibrillation success diminishes quickly when the shock is delayed. This results because shockable rhythms tend to decay within several minutes toward a less shockable form of ventricular fibrillation or asystole. Delayed defibrillation occurs during both out-of-hospital and in-hospital cardiac arrest resuscitation and is associated with poor outcomes from SCA.
CPR Interactions with Defibrillation
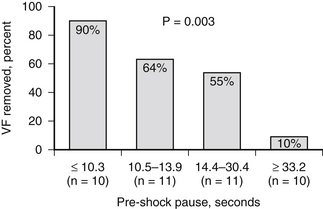
Unless immediate defibrillation is available within 4 to 5 minutes of VF/VT onset, studies have suggested that a patient’s chance of survival increases when CPR is performed before attempting defibrillation. In addition, the quality of the delivered CPR affects defibrillation success. Specifically, pauses in CPR and chest compressions with inadequate depth decrease the probability of successful defibrillation (Figure 49.2). This indicates that the longer myocardial tissue remains without blood flow, the less likely a defibrillatory shock will succeed in restoring a normal sinus rhythm. CPR may therefore act as a primer by restoring some circulation to the heart before defibrillation. The 2005 AHA consensus guidelines for CPR recommend that high-quality compressions continue while the defibrillator is being prepared and charged. This is a safe, proven method to reduce preshock pauses.
Ever since the introduction of defibrillation, common sense has dictated that physical contact with the patient should be avoided during a shock in order to prevent stray electrical current from injuring the rescuer. Although the risk of inadvertent shock to a rescuer exists if a rescuer is still in contact with the patient during defibrillation, the chance of this occurring is very small and new evidence suggests that the risk may be negligible. Some experts suggest that defibrillation could be performed, in theory, by a gloved rescuer without stopping CPR and therefore maximizing the chance for successful shock. Current guidelines still recommend that all rescuers cease contact with the patient before defibrillation, as further research is needed to examine the safety of hands-on defibrillation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree