INTRODUCTION AND EPIDEMIOLOGY
Every year, approximately 6.8 to 8.5 million persons throughout the world1 sustain cardiac arrest. About 70% of cardiac arrests occur out of hospital. The proportion of cardiac arrest patients who are treated varies from about 54.6% (United States) to about 28.3% (Asia). The proportions with ventricular fibrillation (VF) and survival vary from 11% and 2%, respectively, in Asia, to 28% and 6% in North America, 35% and 9% in Europe, and 40% and 11% in Australia.2 About half of cardiac arrest victims are <65 years old.
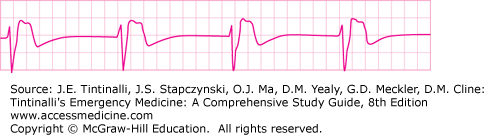
Ventricular tachyarrhythmias are the initiating event in about 80% of patients with out-of-hospital primary cardiac arrest. During ambulatory electrocardiogram (ECG) monitoring of 157 witnessed cardiac arrests, Bayés de Luna et al3 documented 70% with ventricular tachycardia (VT) and VF, 13% with torsades de pointes, and 17% with bradyarrhythmias. Untreated VF deteriorates to asystole in about 15 minutes.4 For patients with sudden cardiac arrest, the rate of survival declines rapidly by about 7% to 10% for each minute without defibrillation.5 If delay to defibrillation exceeds 12 minutes,6 survival is of the order of 0% to 5%.
The structured emergency care system concept for treatment of cardiac arrest is called the Chain of Survival and includes four components: Early Access, Early CPR, Early Defibrillation, and Early Advanced Care. If a community’s prehospital EMS can be activated promptly, reach the patient within 5 minutes of collapse, and deliver the first shock shortly thereafter, survival in excess of 15% to 20% can be expected, with recent reports of >30% survival.7,8 With delayed initiation of CPR, defibrillation, and access to the patient by the emergency services, the impact of advanced life support measures is small (Figure 24-1). Improved survival can only occur if structured emergency care systems allow trained providers to access the patient rapidly and deliver the appropriate treatment in a timely fashion. Delays in initiating the various links weaken the chain and adversely affect the next link, resulting in a decreased chance of a good outcome for the patient.
ADVANCED CARDIAC LIFE SUPPORT (ACLS)
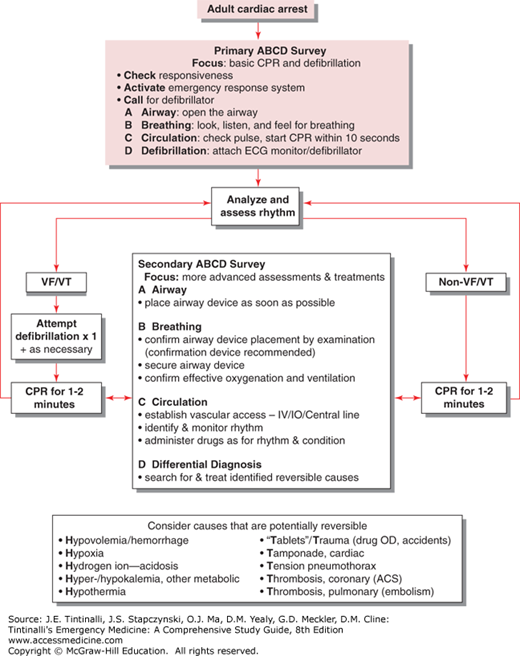
The basic life support assessments and interventions are often called the Primary ABCD Survey, and the advanced life support assessments and interventions are often called the Secondary ABCD Survey.
An organized approach to resuscitation begins with the Primary ABCD and blends smoothly with the Secondary ABCD. These are summarized in the Universal ACLS Algorithm (Figure 24-2). This method helps any ACLS provider remember the sequence of resuscitation actions and, therefore, be less likely to miss any of the vital steps in the care of the patient.
The Primary ABCD Survey addresses the identification of cardiac arrest and performance of good-quality CPR (including ventilation) and defibrillation. The procedures for the ABCs of the primary ABCD are described in chapters 22 and 23.
For ventilation, bag-valve masks deliver 21% oxygen if using room air, 60% oxygen when connected to an oxygen source with flow at 12 L/min, and 90% to 95% with a reservoir bag. Chest compressions need not be stopped to initiate or continue ventilation.
The rescuer also needs to focus on providing good chest compressions (30 compressions for every 2 ventilations [30:2] with compression rate of ≥100/min, compression depth of at least 5 cm or 2 inches, and relaxation of pressure on the chest wall to allow unrestricted chest recoil). Feedback devices are available for the rescuer to provide improved standards of chest compressions.
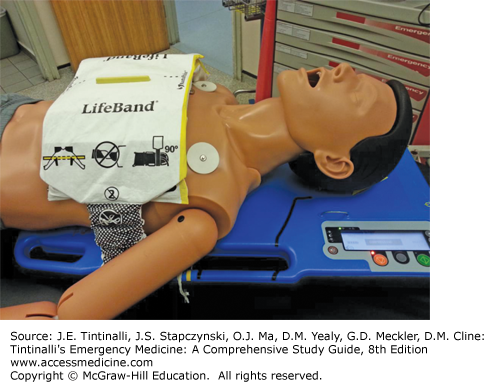
Mechanical CPR devices may also be used. The two most common types of mechanical CPR devices employed in clinical practice are the LUCAS-2 with a piston attached to an active compression-decompression cup (Figure 24-3) and the load-distributing band Autopulse (Figure 24-4). Defibrillator pads must be applied to the bare chest before application of the mechanical CPR devices. These devices allow provision of either 30:2 CPR or continuous chest compressions with interposed manual ventilations.
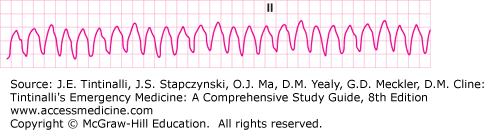
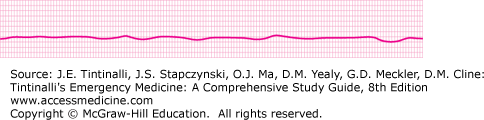
The critical rhythms associated with cardiac arrest are VF (Figure 24-5), pulseless VT (Figure 24-6), asystole (Figure 24-7), and pulseless electrical activity (PEA) (Figure 24-8).
Defibrillation may be done with either an automated external defibrillator (AED) or a manual defibrillator (see chapter 23). Deliver shocks for VF or pulseless VT with minimal interruption of chest compressions only during actual shock delivery. Make sure that the position of the defibrillator pads (Figure 24-9) does not interfere with monitoring leads.
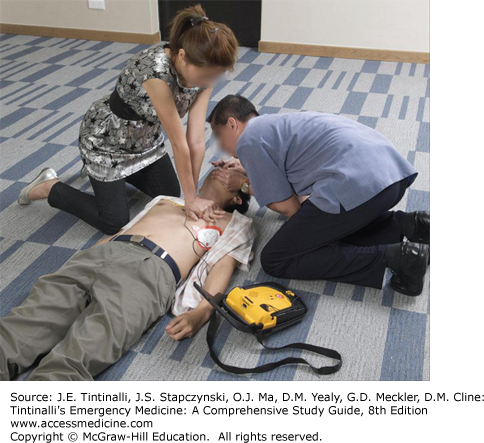
After delivery of the first shock, resume CPR (Figure 24-10) immediately for up to about 2 minutes before reviewing the ECG monitor for a rhythm diagnosis. If a viable rhythm has returned, check for pulse and breathing. If breathing and pulse have returned, begin care for post–return of spontaneous circulation (ROSC) management. If breathing is absent, continue rescue breathing with a bag-valve mask at the rate of about 6 to 10 breaths per minute; if pulse is not present, continue CPR and move to the Secondary ABCD Survey.
Components of the Secondary ABCD Survey are listed in Table 24-1.
| Component and Function | Detailed Components |
|---|---|
| A: Securing the Airway | Endotracheal intubation or other supraglottic airway, eg, Laryngeal Mask Airway |
| B: Breathing (Ventilation) |
|
| C: Maintaining the Circulation |
|
| D: Differential diagnosis |
|
| Specialized Care after ROSC* | Therapeutic hypothermia, glycemic control, early goal directed therapy, percutaneous coronary interventions |
The Secondary ABCD Survey includes endotracheal intubation or the placement of another airway adjunct, assessment of ventilatory status, gaining intravenous access, identifying ECG rhythms, delivering drugs to enhance circulation, and addressing the reasons for the occurrence or persistence of cardiac arrest. While the secondary ABCDs are in progress, continue the basic resuscitative actions of the primary ABCDs. Usually, defibrillation pads placed carefully left of the apex and to the right of the sternum just below the right clavicle (Figure 24-9) can also act as monitoring leads. Otherwise, true monitoring leads may be placed at the front of the right and left shoulders and over the left iliac crest. Such placement does not interfere with defibrillation or cardiac pacing procedures. Further management is based on the cardiac rhythm.
Vascular access techniques are discussed in Chapter 31, “Vascular Access.” A large peripheral vein allows a rapid rate of fluid administration, if needed. If unable to cannulate a peripheral vein, establish intraosseous access. Central venous lines take time to establish and, because of the length of the cannula, cannot deliver fluids as rapidly as a peripheral line, and every bolus dose of drugs requires flushing with at least 20 mL of normal saline. Central lines are useful for central venous pressure monitoring to guide fluid resuscitation and circulatory management.
In cardiac arrest, circulation of blood grinds to a halt. With good-quality CPR, one can expect to generate up to about 30% of normal cardiac output, which is just about what is required to supply vital organs such as the heart, brain, and kidneys. The reduced circulation is associated with a slower circulation time. Therefore, drugs given during cardiac resuscitation are best administered via a proximal peripheral vein. Once drugs are given, flush the line with normal saline, and continue CPR for at least 30 to 60 seconds before repeat external defibrillation, so that the heart is optimally primed to respond.
The optimal infusion fluid is normal saline and not dextrose, Ringer’s lactate, or sodium bicarbonate. However, unless hypovolemia is a contributing factor to cardiac arrest, fluid infusion should be slow, if at all necessary. Drug dosages are the same whether given by the intraosseous, IV, or central line routes. The endotracheal tube route is no longer recommended for drug administration because drug absorption is limited if the airway is filled with pulmonary edema fluid.
DRUGS USED IN RESUSCITATION TO ROSC FROM CARDIAC ARREST
Drugs available for cardiac resuscitation and cardiac dysrhythmia management are also described in chapters 19 and 20. This section will cover those drugs specifically used for resuscitation from cardiac arrest to ROSC. Drugs are an adjunct in the management of cardiac arrest patients. Good CPR, ventilation, and early defibrillation are the cornerstones of management of cardiac arrest. The effectiveness of standard resuscitative drugs on ROSC and survival to hospital discharge has not been well demonstrated.9,10,11 However, consensus documents recommend the standard resuscitative drugs described below with the presumptive rationale that drugs help “restart” the heart and preserve coronary and cerebral circulation.
Epinephrine (adrenaline) is an endogenous catecholamine. It has an important role in cardiac arrest, although the evidence base for improved outcomes in humans is weak.12 Epinephrine seems to improve short-term survival.13 The primary beneficial effect appears to be peripheral vasoconstriction, which improves cerebral and coronary blood flow. Potential adverse effects include an increase in myocardial oxygen consumption and an increase in pulmonary shunting. The most common adverse reaction is tachycardia. Epinephrine may worsen myocardial ischemia and induce ventricular ectopy and VT. Epinephrine is used mainly to treat cardiac arrest from VF or pulseless VT unresponsive to the initial shock, asystole, PEA, and profoundly symptomatic bradycardia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree