Chapter 38 Acute liver failure
DEFINITION AND AETIOLOGY
Acute liver failure (ALF) is a complex multisystemic illness that evolves after significant liver insult. The liver damage is manifest by the development of coagulopathy and encephalopathy within days or weeks of the liver injury. ALF is a heterogeneous condition incorporating a range of clinical syndromes. The dominant factors that give rise to this heterogeneity are the variable aetiology, the age of the patient and concomitant comorbidity and the duration of time over which the disease evolves. There are multiple definitions used in this disease but the one used by O’Grady et al. is most commonly used, utilising the description of acute, hyperacute and subacute.1 This system uses a trigger of jaundice and encephalopathy whilst others have used symptoms of encephalopathy. All the definitions used recognise that the syndrome may have a rapid presentation or a somewhat slower presentation, and the clinical features and outcomes are significantly different in the two presentations.
The O’Grady et al. definitions are given below.
SUBACUTE DISEASE
The aetiology of ALF must always be sought, not just for prognosis but for treatment options (Table 38.1).
Table 38.1 Causes of liver failure
| Cause | Agent responsible |
|---|---|
| Viral hepatitis | Hepatitis A, B, D, E, cytomegalovirus, herpes simplex virus, seronegative hepatitis (14–25% of cases in the UK) |
| Drug-related | Dose-related, e.g. paracetamol, and idiosyncratic reactions, e.g. antituberculous drugs, statins, recreational drugs, anticonvulsants, non-steroidal anti-inflammatory drugs, cyproterone and many others |
| Toxins | Carbon tetrachloride, Amanita phalloides |
| Vascular events | Ischaemic hepatitis, veno-occlusive disease, Budd–Chiari Heatstroke |
| Other | Pregnancy-related liver diseases, Wilson’s disease, lymphoma, carcinoma, trauma |
The relative incidence of aetiologies varies across the world. Paracetamol is common in the UK, USA and Denmark, whereas hepatitis B is more common in France. A recent paper from the USA Acute Liver Failure group highlights the increasing incidence of paracetamol toxicity and also the potential role it plays as a covert agent in patients with no history of excess ingestion and non-specific symptoms that would otherwise be attributed to the seronegative group.2 The rate of hepatitis B virus-induced ALF is decreasing with immunisation but is still highly prevalent and should always be considered.
Acute viral hepatitis accounts for 40–70% of patients with ALF worldwide. Clinical characteristics are shown in Table 38.2. Acute hepatitis A (HAV) infection rarely leads to ALF (0.35% of infections), but continues to account for up to 10% of cases; morbidity increases with the age of infection. It is hoped that the rate will decrease with improving hygiene standards generally and the uptake of vaccination. It is diagnosed by the presence of the immunoglobulin (Ig) M antibody to HAV. HAV-related ALF has a relatively good prognosis, although age and comorbidity are relevant.
Table 38.2 Aetiology of acute liver failure and initial investigations
| Hepatitis A (HAV) | Immunoglobulin M (IgM) anti-HAV |
| Hepatitis B + D (HBV, HDV) | HBsAg, IgM anti-core, HBeAg, HBeAb, HBV DNA, delta antibody |
| Hepatitis E (HEV) | IgM antibody |
| Seronegative hepatitis | All tests negative: diagnosis of exclusion |
| Paracetamol | Drug levels in blood and clinical pattern of disease – may be negative on third or subsequent days after overdose; markedly elevated aspartate and alanine serum transaminase (often > 10 000) |
| Idiosyncratic drug reactions | Eosinophil count may be elevated, although most diagnoses are based on temporal relationship |
| Ecstasy | Blood, urine, hair analysis and history |
| Autoimmune | Autoantibodies, immunoglobulin profile |
| Pregnancy-related syndromes | |
| Fatty liver | Uric acid elevated, neutrophilia, often first pregnancy, history, CT scan for rupture and assessment of vessels |
| HELLP syndrome | Platelet count, disseminated intravascular coagulation a prominent feature; CT scan as above |
| Liver rupture | May be seen in association with pre-eclampsia, fatty liver and HELLP |
| Wilson’s disease | Urinary copper, ceruloplasmin (although low in many causes of acute liver failure), present up to second decade of life, Kayser–Fleischer rings, low alkaline phosphate levels |
| Amanita phalloides | History of ingestion of mushrooms, diarrhoea |
| Budd–Chiari syndrome | Ultrasound of vessels (HV signal lost, reverse flow in portal vein), CT angiography, ascites, prominent caudate lobe on imaging, haematological assessment |
| Malignancy | Imaging and histology; increased alkaline phosphate and LDH; often imaging may be interpretated as normal |
| Ischemic hepatitis | Clinical context, marked elevation of transaminases (often > 5000); may demonstrate diated hepatic veins on ultrasound, echocardiogram |
| Heatstroke | Myoglobinuria and rhabdomyolysis are often prominent features |
CT, computed tomography; HELLP, haemolysis (microangiopathic haemolytic anaemia), elevated liver enzymes and low platelets; HIV, human immunodeficiency virus; LDH, lactate dehydrogenase.
Acute hepatitis B (HBV) has been the cause of 25–75% of instances of ALF from viral hepatitis. The liver injury is immunologically mediated with active destruction of infected hepatocytes. Diagnosis is by the presence of the IgM antibody (HBcAb) to hepatitis B core antigen. Hepatitis B surface antigen (HbsAg) is frequently negative by the time of presentation. Hepatitis B DNA should also be assayed. ALF may also be seen with hepatitis D, as either a coinfection or suprainfection. Reactivation of hepatitis B is an increasing cause of ALF and should always be considered in a patient who has received steroids or chemotherapy. High-risk patients should be screened for sAg and HBV DNA and treated with antiviral agents if they are positive. This is a recognised problem in oncology and haematology but it is also a potential risk to patients in intensive care where steroids may be administered.
Seronegative hepatitis (so called) is seen in patients in whom there are no identifiable viral causes nor obvious candidate drugs. Such patients may present with a prodromal illness and with acute or subacute maniifestations of the disease. Prognosis is less good than those with an identifiable virus and once they have poor prognostic criteria the chances of survival without liver transplant are exceptionally small. A subgroup may represent an acute autoimmune form of ALF, although many will not have any positive immmune markers such as elevated IgG or positive smooth-muscle or liver kidney antibodies. The pattern of markers shows an increased incidence of autoantibody positivity in seronegative cases and viral cases with elevated IgM in viral causes.2,3
Drug-induced hepatitis is responsible for approximately 15–25% of cases of ALF. In some patients there appears to be a true hypersensitivity reaction, and symptoms develop after a sensitisation period of 1–5 weeks, recur promptly with readministration of the drug and may be accompanied by fever, rash and eosinophilia. In others the clinical pattern is less acute. Some herbal remedies are implicated as putative hepatotoxins but their role is made more difficult to assess by the variable nature of the constituent parts. Halothane hepatitis is now almost unheard of.
FULMINANT WILSON’S DISEASE
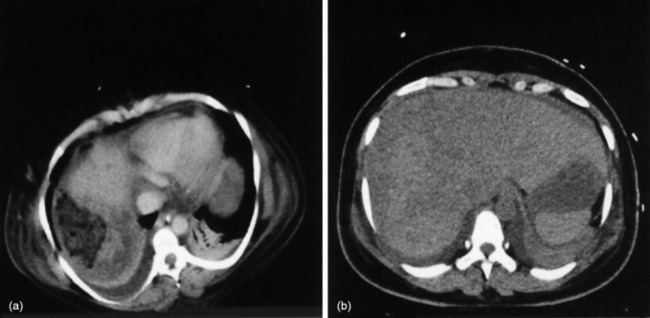
Pregnancy-related liver failure includes HELLP (haemolysis (microangiopathic haemolytic anaemia), elevated liver enzymes and low platelets), acute fatty liver of pregnancy and liver rupture, often in association with pre-eclampsia. The prognosis of pregnancy-related ALF is usually good, although some develop severe liver injury with small-vessel disease, liver ruptures may require packing and occasionally transplantation is required (Figure 38.1).
Heat shock injury is now relatively rarely seen but the ischaemic hepatitides remain relatively common. They are normally associated with a congested liver that is subjected to a secondary insult – hypoxia or decreased-flow arterial inflow. This is seen with hypoxaemic respiratory failure, cardiac arrhythmias and hypotension.
Hepatic venous obstruction (Budd–Chiari syndrome) may cause ALF. There are symptoms and signs of liver of necrosis, often with capsular pain from congestion and ascites. In Asia this may be associated with anatomical anomalies of the inferior vena cava, whereas in Europe and the USA the experience is normally of thrombosis of the hepatic veins, often with an underlying procoagulant condition (Figures 38.2 and 38.3).
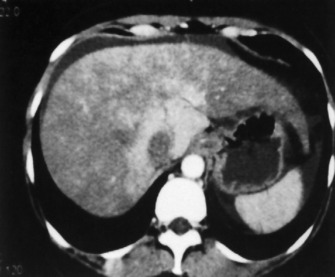
Figure 38.2 CT of Budd Chiari demonstrating arterio portal shunting and clot in Hepatic veins and IVC.
DIAGNOSIS
The aetiology of ALF must be accurately identified; some specific investigations are outlined in Table 38.2. History and clinical examination are paramount in this disease and the clinical course of biochemical and haematological parameters is important in assessing course and management. All patients should have routine chemistry, haematology and coagulation assessment; viral and autoimmune profiles should similarly be undertaken in all.
The biopsy is normally undertaken by the transjugular route.
SPECIFIC TREATMENTS
SPECIFIC CONSIDERATIONS
Chelating agents are not of benefit in patients with established ALF secondary to Wilson’s disease but play an important role in chronic presentations. Withdrawal of such treatments, or indeed non-compliance, especially in teenagers, may precipitate ALF.
Steroid therapy is beneficial in acute autoimmune hepatitis but its role in autoimmune ALF has been less clear. A recent publication from the Paris group suggests that steroids for those with established ALF are potentially detrimental.4
CLINICAL COURSE, COMPLICATIONS AND MANAGEMENT
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree