Chapter 59
Acute Liver Failure 
Etiology of Acute Liver Failure
The prognosis of ALF is dependent on its etiology, so every effort should be made to look for the underlying cause of the liver injury (Table 59.1). However, up to 20% of cases will have no discernable cause. The most common cause of ALF in the United States is acetaminophen toxicity, most recently accounting for approximately 39% to 50% of all cases of ALF. Idiosyncratic drug reactions account for 13% of cases of ALF. Viral hepatitis (acute hepatitis A and B combined) has become a less frequent cause of ALF in the United States, accounting for only 12% of all cases. Acute hepatitis C does not appear to lead to ALF. Hepatitis E is a significant cause of liver failure in endemic countries (Russia, Pakistan, Mexico, and India) and should be considered in any patient who travels to these countries and in any pregnant woman, as hepatitis E has a more severe course during pregnancy.
TABLE 59.1
| Category | Examples |
| Drugs | Acetaminophen, halothane, phenytoin |
| Miscellaneous | Acute fatty liver of pregnancy, Reye syndrome, Wilson disease, malignant infiltration, autoimmune hepatitis |
| Toxins | Amanita phalloides, carbon tetrachloride |
| Vascular | Budd-Chiari syndrome, cocaine, heat stroke, ischemia (“shock liver”), veno-occlusive syndrome |
| Viral hepatitis | Hepatitis A, B, D, E, C,∗ G,∗ CMV, HSV, EBV, varicella |
CMV, cytomegalovirus; HSV, herpes simplex virus; EBV, Epstein-Barr virus.
Wilson disease and autoimmune hepatitis account for 3% and 4% of all cases of ALF, respectively, and are unique in that patients can still be considered as having ALF even though there is a preexisting chronic liver disease if the disease previously had been unrecognized. Mushroom toxicity (usually Amanita phalloides) may cause ALF, and the initial history should always include recent mushroom ingestion. Acute fatty liver of pregnancy and hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome (Chapter 72) typically occur during the third trimester, and prompt delivery of the fetus is essential to achieve good outcomes.
Diagnosis and Initial Evaluation
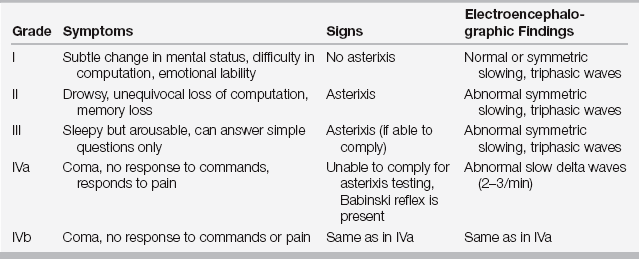
History taking should include a careful review of possible medication overdoses (especially acetaminophen and acetaminophen-containing products), medications newly started within the last 6 months, toxins (Amanita phalloides mushrooms in particular), herbal supplements, and risk factors for exposure to an acute viral hepatitis. Physical examination should focus on any stigmata of chronic liver disease; the prognosis is improved in a patient with acute on chronic liver injury compared to a patient with ALF alone. Observe patients frequently for the development of hepatic encephalopathy; once grade I or II encephalopathy has developed, transfer patients to a transplant center as they may deteriorate rapidly (Table 59.2).
Initial laboratory examination must be extensive and include tests to evaluate for the severity and etiology of the ALF (Table 59.3). Plasma ammonia (venous or arterial), although not very useful in patients with chronic liver disease, can help determine the risk for cerebral herniation in patients with ALF. Although no definite threshold ammonia level has been established, patients with arterial ammonia levels > 200 mcg/dL have a significant risk (close to 100%) of developing severe hepatic encephalopathy and a 55% risk of developing increased intracranial pressure. The utility of a liver biopsy is marginal, as it will usually not change therapy; if indicated, it is typically done via the transjugular approach because of a patient’s coagulopathy.
TABLE 59.3
Acetaminophen level
Ammonia level
Arterial blood gas
Autoimmune markers: ANA, ASMA, immunoglobulin levels
CBC
Ceruloplasmin level
Comprehensive panel
HIV
Pregnancy test (females)
Prothrombin time/INR
Toxicology screen
Type and screen
Viral hepatitis serologies: anti-HAV IgM, HepBsAg, anti-HepBcore IgM, HCV Ab
Wilson disease requires special consideration, as it may be difficult to diagnose because the low ceruloplasmin levels that are characteristic of the disease are present in most patients with ALF, regardless of etiology. Kaiser-Fleischer rings are not uniformly present and serum copper levels require several days to obtain. In these cases, a very low alkaline phosphatase with a marked hyperbilirubinemia resulting from profound hemolytic anemia is relatively specific for Wilson disease. An alkaline phosphatase-to-total bilirubin concentration less than 4 is consistent with Wilson disease and may aid in the diagnosis. Rapid diagnosis is essential; these patients will require a liver transplant as spontaneous recovery is estimated at 0%.