Acute Compartment Syndrome
Andrew D. Perron, Christopher T. Bowe, and Christine Irish
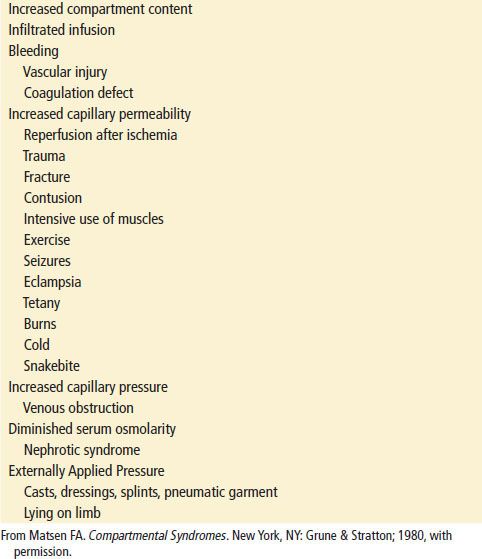
Acute compartment syndrome is a serious life- and limb-threate-ning complication of extremity trauma. Fractures, crush injuries, burns, and arterial injuries all can result in an acute compartment syndrome. Compartment syndrome is defined as the presence of pathologically elevated intramuscular pressures within confined osseofascial compartments resulting first in tissue ischemia and ultimately infarction and subsequent contractures if not treated in a timely and appropriate manner (1). Dr. Richard Von Volkmann first described this entity in 1881; he noted the complication of muscle ischemia, paralysis, and ultimate contracture in a child with a supracondylar fracture (2,3). The various compartments in the extremities are composed of muscle groups bound by dense fascial tissue planes that result in limited ability to accommodate increased pressure. In addition to muscle, these compartments contain various nerves and blood vessels. Elevated pressure in these spaces, above normal physiologic ranges, can compromise capillary blood flow and produce predictable clinical signs and symptoms. Delays in diagnosis and treatment can result in myonecrosis, permanent nerve damage, distal ischemic injury, and muscle contracture. The exact incidence of compartment syndrome is unknown, although it is thought to be relatively rare. Three-quarters of cases are associated with fractures. Fractures of the tibia are the most likely to result in compartment syndrome; the incidence in patients with tibial fractures is reported to range from 1% to 29% (2). The most frequently involved compartments are the anterior compartment of the lower leg and the flexor compartment in the forearm (2). Table 48.1 lists the common locations of compartment syndromes.
TABLE 48.1
Common Locations of Compartment Syndromes
The pathophysiology of compartment syndrome involves local hydrostatic and osmotic pressure conditions within the myofascial compartment. When the intracompartmental pressure increases above a specific level due to the above factors, perfusion to the compartment is impaired, resulting in disruption of skeletal muscle metabolic processes. Cell wall membrane integrity is compromised, leading to cytolysis with the release of osmotically active cellular contents into the extracellular compartment. This draws additional fluid from plasma into the interstitial space. The net effect is increased intracompartmental pressure and further impairment of perfusion to the closed space of the myofascial compartment as well as to distal structures in that vascular distribution. This progressively leads to compromise of circulation and nerve conduction and ultimately to irreversible damage to the contents of the compartment (4).
Normal compartment pressure is below 10 to 12 mm Hg (2). Capillary blood flow depends on the pressure gradient between the arterial and venous systems. With elevated compartmental pressures, this gradient is interrupted, compromising the blood flow across the capillary bed. When the pressure within a compartment rises sufficiently to interrupt this arteriovenous gradient, blood flow will be reduced to the point at which the metabolic demands cannot be met. Then functional abnormalities and compartment syndrome occur (2). Two general mechanisms can result in elevated compartment pressures: Either an extrinsic compressive force constricts the compartment (e.g., a cast) or there is an intrinsic increase in the size of the fascia-bound compartment owing to edema or hemorrhage.
Clinically significant reduction of blood flow and blood oxygenation can occur at tissue pressures above 20 mm Hg (5,6). Cellular metabolic derangements are closely associated with the difference between mean arterial blood pressure and compartment pressure. This difference is known as the delta P. In one study, the lowest delta P that was compatible with a normal metabolic state was 30 mm Hg in normal muscle (7). The length of time that tissue can tolerate elevated pressures before pathologic changes occur is less clear. Sensory changes including paresthesias and hypesthesia can develop within 30 minutes of ischemia, whereas irreversible nerve damage begins as soon as 6 hours and almost universally after 12 to 24 hours (2).
Other factors should also be considered when assessing potential compartment syndrome. Externally applied pressure (i.e., casting) tends to produce less elevation in compartment pressures as compared to similar levels of internally developed pressures (i.e., edema or hemorrhage) (8). Postischemic compartment syndrome is caused by revascularization after a prolonged period of ischemia (2), leading to the release of vasoactive factors that result in fluid extravasation and elevated pressures. Concurrent hypotension, hypoxia, and associated premorbid conditions such as peripheral vascular disease adversely affect the ability of ischemic tissue to tolerate even mildly elevated tissue pressures.
CLINICAL PRESENTATION
Pain out of proportion to examination findings is the classically described clinical finding in acute compartment syndrome. This assumes an awake, neurologically intact patient. Unfortunately, many patients at risk for compartment syndrome are severely injured or impaired and cannot relate the degree of pain they are experiencing. When reported, the pain is often described as deep, aching, and poorly localized and does not typically respond to immobilization or analgesic medications alone. Increasing analgesic requirements may be the only clue to a developing compartment syndrome. Classically, passive stretching of involved muscles produces intense pain, as does compression of an affected compartment. Weakness or paresis of muscle function is a late finding. Distal hypesthesias or paresthesias may be noted in the distributions of nerves passing through the compartment. Two-point discrimination and light touch are considered more sensitive than pinprick when assessing sensation. Tenseness of externally palpable compartments is the earliest and most objective finding, although tenseness of compartments such as the deep posterior compartment of the lower leg and the iliacus compartment can be difficult to assess due to anatomic location. Findings of compartment syndrome can present within 2 hours of injury but may first appear up to 6 days later (2). Progressive worsening over time helps to distinguish compartment syndrome from other injuries that cause primary nerve and muscle damage.
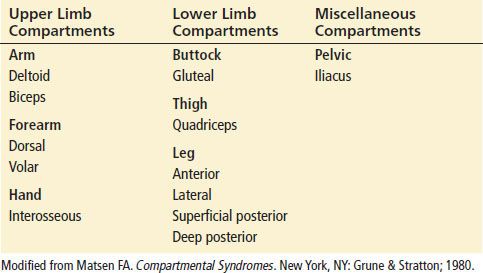
Griffith’s mnemonic, the five Ps (pain, pallor, pulselessness, paresthesias/paresis, and poikolothermia), is traditionally used for this clinical entity. However, pulses are most often maintained, and the skin does not typically develop pallor (1). The presence of all five of these signs more accurately reflects the late findings of acute arterial obstruction or insufficiency. As noted previously, the reliance on the clinical examination makes it difficult to assess emergency department (ED) patients with altered sensorium, acute intoxication, spinal cord injuries, or overlying extensive burns, as well as children. Moreover, obtunded patients are often at risk for compartment syndrome by compression, entrapment, or unknown mechanisms of trauma. Overdose-related compartment syndromes tend to affect the lower extremities (9,10). Critically ill pediatric and adult patients may experience iatrogenic causes of compartment syndrome produced by intravenous and intraosseous infiltrations, transfusions under pressure, or tourniquet malfunction. Table 48.2 lists common etiologies of compartment syndrome. Owing to dense eschar, severely burned patients lose most, if not all, clinical signs of compartment syndrome. In these more complex cases, the clinician should have a lower threshold for using invasive monitoring.
TABLE 48.2
Common Etiologies of Compartment Syndromes Seen in Emergency Medicine