INTRODUCTION AND EPIDEMIOLOGY
Bacterial and viral infections of the respiratory tract can result in a wide range of clinical syndromes including acute bronchitis, the common cold, influenza, and respiratory distress syndromes. Uniform definitions for the most common of these clinical syndromes are lacking because the symptoms associated with upper respiratory tract infections (URIs) frequently overlap and their causative pathogens are similar. The broad definition of acute bronchitis is as follows: a self-limited inflammation of the large airways characterized by cough without evidence of pneumonia, without an alternative medical disorder to explain the symptoms, or without a history of chronic lung disease.1
The common cold is a viral infection of the upper respiratory tract, primarily affecting the nasal mucosa, causing congestion, rhinorrhea, and sneezing. Influenza, or the “flu,” is a respiratory illness caused by influenza viruses. Symptoms of influenza infection range from mild to severe and include fever, chills, myalgias, headache, malaise, cough, and fatigue. Severe acute respiratory syndrome is a unique respiratory illness that has clinical characteristics similar to other URIs but confers a high rate of mortality. Reported in 2012, Middle East respiratory syndrome coronavirus is novel viral respiratory infection that became a concern to the World Health Organization due to its fatality rate. Infections of the upper respiratory tract also cause specific clinical conditions like otitis media, pharyngitis, epiglottitis, bronchiolitis, laryngitis, tracheitis, and sinusitis (see corresponding chapters that discuss these diseases).
In ambulatory care settings nationwide, URIs are the third most common diagnosis.2 Annually, the estimated direct costs of noninfluenza viral URI in the United States is $17 billion, with indirect costs exceeding $22 billion.3 Acute bronchitis is among the most commonly diagnosed outpatient illnesses in the United States every year, with an annual incidence of about 5%,4 predominantly during fall and winter.1 The disorder accounts for approximately 10 million office visits per year, or 10 ambulatory visits per 1000 people per year. Symptom relief is the primary reason for office visits among adults within the first 2 weeks of illness, and many of these visits result in the unnecessary prescription of antibiotics by clinicians.5 The common cold afflicts adults three or three times every year, whereas children suffer up to eight colds annually.6,7,8 The incidence of colds caused by rhinovirus peaks during autumn months.9 Responsible for 22 million missed school days and 23 million lost work days, the common cold generates an enormous economic burden.4
Influenza affects millions of people worldwide every year during seasonal outbreaks (typically November through March in the northern hemisphere). An annual average of 41,000 Americans died from influenza infection from 1979 to 2001.10 The Centers for Disease Control and Prevention reported influenza-associated annual death rates between 1976 and 2007 that ranged from 1.4 to 16.7 deaths per 100,000 persons. Deaths associated with influenza have increased in recent decades in the United States. With 90% of influenza-associated deaths occurring among people 65 years or older, influenza poses a particular threat to the elderly.11,12 In 2009, an outbreak of swine-origin influenza A (H1N1) virus, known as “swine flu,” occurred in Mexico and the United States.13,14
Influenza viruses are classified into three genera: A, B, and C. Of these, influenza A has the greatest impact on human populations and has the greatest potential to cause pandemics. Influenza A has many serotypes, including H1N1 and H3N2, both of which are currently active among humans. Influenza viruses are unique pathogens because their evolution involves a complex process of antigenic shifts and sporadic cross-species transmissions between humans, swine, and birds. The intensity of seasonal influenza varies from one year to the next, and localized influenza outbreaks can occur during interpandemic years.15 Furthermore, seasonal influenza outbreaks tend to occur simultaneously in countries on similar latitudes. Population immunity against influenza can be achieved by natural infection or vaccination; however, antigenic shifts allow influenza viruses to survive from year to year and preserve their capacity to cause global pandemics.
ACUTE BRONCHITIS
Etiologic studies of acute bronchitis are difficult to interpret because the disease lacks a precise definition and the cause is undetermined in 31% to 84% of cases vigorously tested.16,17,18,19,20,21,22,23 Respiratory viruses are the most common causative agents, with confirmed cases in 9% to 63% of patients studied, depending on the criteria used to make the diagnosis and the population.16,17,18,19,20,21,22,23 Influenza A and B viruses are the most common cause, accounting for 6% to 35% of cases.16,17,18,19,20,21,22,23 Parainfluenza virus, respiratory syncytial virus, coronavirus, adenovirus, rhinovirus, and human metapneumovirus combined account for another third of cases.16,17,18,19,20,21,22,23 Bacterial causes of acute bronchitis range from less than 10%16 to as much as 44% of cases in studies of older populations with comorbidities and severe symptoms.21 Streptococcus pneumoniae (0% to 30% of cases), Haemophilus influenzae (0% to 9% of cases), and Moraxella catarrhalis (0% to 2% of cases) have been isolated in patients with acute bronchitis.16,17,18,19,20,21,22,23 Atypical bacterial species such as Bordetella pertussis (0% to 1%),24 Chlamydia pneumoniae (0% to 17%), and Mycoplasma pneumoniae (1% to 10%) also cause acute bronchitis.16,17,18,19,20,21,22,23
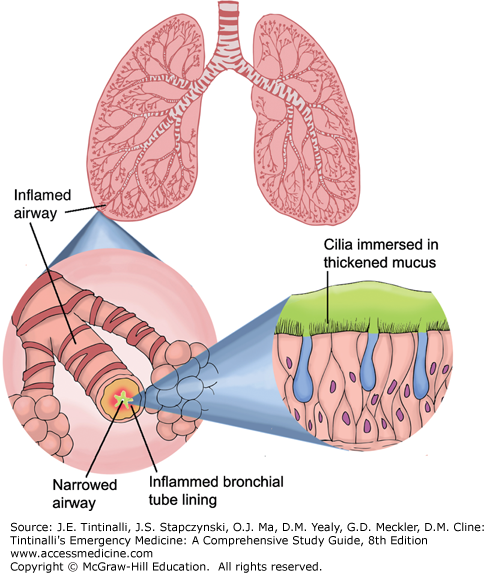
There are two overlapping sequential phases in the pathophysiology of acute bronchitis.25 The first phase results from the direct inoculation of the tracheobronchial epithelium, yielding variable constitutional symptoms of fever, myalgias, malaise, and organism-specific upper respiratory symptoms, lasting 1 to 5 days, the severity of which depends on the infectious agent. The second phase is characterized by hypersensitivity of the tracheobronchial epithelium and airway receptors resulting in persistent, productive cough and lasting 1 to 3 weeks, peaking at 7 to 14 days. It is this second phase that best characterizes the illness. Sloughed epithelial cells and increased mucus produce sputum in most patients; sputum is not an indication of ongoing bacterial infection as frequently suspected by clinicians.25 Inflammation and thickening of the bronchial and tracheal mucosa (Figure 64-1) result in airflow obstruction and decreased forced expiratory volume in 1 second, manifesting as wheezing and dyspnea in many patients.
The clinical manifestations of acute bronchitis depend on the infectious agent, especially in the first phase of the illness. Therefore, the initial symptoms are variable and may include fever, dyspnea, myalgias, malaise, sore throat, nasal congestion, and cough. The hallmark of acute bronchitis is cough (with or without phlegm production) persisting into the second phase of the illness lasing more than 5 days and up to 3 or 4 weeks.1,25 The mean duration of cough is 18 days.26 During this phase, the patient may or may not have dyspnea and/or chest discomfort. Physical exam may be completely normal, or the patient may have tachypnea, tachycardia, fever, wheezing, rhonchi, or rales. One important etiology of acute bronchitis to identify is Bordetella pertussis, because antibiotic treatment is recommended (see later discussion).25,27 Suspect pertussis in patients with posttussive emesis or inspiratory whoop27; consider pertussis in any patient with cough lasting greater than 2 weeks if exposed to a known case or presenting during an epidemic.1,25
The diagnosis of acute bronchitis is made using clinical findings and historical information: when acute cough (dry or productive) is present for more than 5 days and when evidence of pneumonia, acute asthma, or an alternative explanation for the symptoms is are absent. Patients with chronic obstructive pulmonary disease are excluded from the diagnosis (see chapter 70, Chronic Obstructive Pulmonary Disease).
The primary objective in patient evaluation is carefully excluding pneumonia, either clinically or radiographically. Physicians are poor at differentiating patients with pneumonia from patients with bronchitis based on history and physical exam.28,29,30,31 The addition of C-reactive protein testing does not improve diagnostic accuracy.29,32 Identification of patients at low risk for pneumonia may be accomplished based on the absence of vital sign abnormalities and physical exam findings.30,31,33 See Table 64-1 for criteria suggesting pneumonia; patients meeting none of these criteria have a probability of pneumonia of 5% or less, and further testing is not required provided the patient has follow-up in the next 3 days and is able to return to the ED if symptoms worsen.30,31,33 Patients with hypoxia or unstable vital signs (in the setting of respiratory symptoms) are at high risk for pneumonia and require further testing and treatment (see chapter 65, Pneumonia and Pulmonary Infiltrates). Obtain a chest radiograph in patients at intermediate risk for pneumonia. Although chest radiography remains the most common confirmatory test for pneumonia,34,35 the sensitivity of a standard two-view chest film ranges from 69% in symptomatic patients suspected of pneumonia in the community,36 to as low as 43.5% in patients being evaluated for pulmonary embolism in the ED37 (both studies using high-resolution CT scan as the criterion reference). Therefore, if pneumonia is suspected on clinical grounds, treat accordingly regardless of a negative chest radiograph (see chapter 65) especially in the elderly, among whom distinctive signs and symptoms of pneumonia may be lacking.1 Laboratory tests should be obtained if treatment for B. pertussis is being planned; tests include a culture, using a Dacron swab specimen, collected from the posterior nasopharynx; performing direct fluorescent antibody staining; collecting a polymerase chain reaction test; or testing for serum antibodies by enzyme-linked immunosorbent assays or Western blot.27 Otherwise, further testing for acute bronchitis is not necessary unless alternative diagnoses require investigation. The differential diagnosis of cough is broad; see Table 64-5, Differential of Consequence: Cough, in chapter 62, Respiratory Distress.
| Criteria | Clinical Finding |
|---|---|
| 1 | Heart rate >100 beats/min |
| 2 | Respiratory rate >24 breaths/min |
| 3 | Temperature of >38°C (100.4°F) |
| 4 | Chest examination findings of focal consolidation, egophony (increased resonance of voice sounds heard when auscultating the lungs), or fremitus (tactile vibrations felt over the chest when the patient repeats “boy oh boy”) |
| 5 | Age > 64 y old |
Case definitions of acute bronchitis that specify constitutional or respiratory symptoms including characteristics of sputum are used by research investigators and can define the spectrum of microbiologic causes but have not identified a patient subset that clearly benefits from antibiotics (see Acute Bronchitis, Treatment, later in this chapter).
Despite the fact that some patients with acute bronchitis have evidence of a bacterial infection in epidemiologic studies, antibiotics are not beneficial and are not indicated except in isolated cases.1,5,38,39 A Cochrane analysis reviewed 15 randomized controlled trials, involving 2618 patients, including smokers and nonsmokers, comparing any antibiotic versus placebo or no treatment for acute bronchitis. At follow-up, patients receiving antibiotics were less likely to have cough (relative risk 0.64; 95% confidence interval 0.49 to 0.85), were less likely to have abnormal lung exam findings (relative risk 0.54; 95% confidence interval 0.41 to 0.70), experienced fewer days of feeling ill (mean difference –0.64; 95% confidence interval –1.16 to –0.13), and had fewer days with limited activity (mean difference –0.49; 95% CI –0.94 to –0.04).39 Although the differences between these outcome measures reached statistical significance, the benefits demonstrated were modest (less than 1-day benefit in an illness lasting 10 to 21 days). Consider potential medication side effects, cost, and the potential for microbial resistance when using antibiotics to achieve these modest benefits for an otherwise self-limiting illness. Despite the lack of evidence supporting their use, the majority of acute bronchitis patients receive antibiotics, especially elderly patients and smokers.1,5,38,40,41,42
To counter public perception and patients’ prior experiences with antibiotics, offer patient education.43 Both printed and computer-assisted patient educational intervention reduce antibiotic prescriptions in the primary care setting.44 Give azithromycin (500 milligrams on day 1, 250 milligrams on days 2 to 5) or similar macrolide for patients with presumed or confirmed B. pertussis infection to prevent transmission to contacts.1,5,27 For influenza, if the patient presents very early in the course and influenza is suspected as the cause, consider influenza-specific antiviral therapy (see later section, Influenza).
There is little evidence to support the routine use of β2-agonists for acute bronchitis in the absence of wheezing on physical exam.1,5,39 A Cochrane Review reported no significant differences in daily cough scores or in duration of cough among adults with acute bronchitis who received β2-agonists versus placebo or no treatment. Adults treated with β2-agonists were more likely to report adverse effects such as tremor, shakiness, and nervousness (relative risk 7.94; 95% confidence interval 1.17 to 53.94).45 However, among patients with evidence of airflow obstruction, β2-agonists result in lower symptom scores and faster cough resolution.45 Therefore, consider bronchodilators in acute bronchitis patients with wheezing.46 Antihistamines do not reduce mean cough scores in acute bronchitis. Limited data are available on the efficacy of antitussives for acute bronchitis, and no data exist on the value of oral corticosteroids in nonasthmatics with acute bronchitis.47 Dextromethorphan and codeine preparations may be no more effective than placebo in improving symptoms or reducing cough severity in acute bronchitis.38 If used, limit antitussive therapy to those patients with a cough causing discomfort where inhibition of airway secretion clearance will not compromise breathing.46
COMMON COLD
The pathogens responsible for causing the common cold include rhinovirus, adenovirus, parainfluenza virus, respiratory syncytial virus, enterovirus, and coronavirus. The rhinovirus, a species of the Enterovirus genus of the Picornaviridae family, is the most common cause of the common cold and causes up to 80% of all respiratory infections during peak seasons.8,9,48 Dozens of rhinovirus serotypes and frequent antigenic changes among them make identification, characterization, and eradication exceedingly complex. After deposition in the anterior nasal mucosa, rhinovirus replication and infection are thought to begin upon mucocilliary transport to the posterior nasopharynx and adenoids. As soon as 10 to 12 hours after inoculation, symptoms may begin. The mean duration of symptoms is 7 to 10 days, but symptoms can persist for as long as 3 weeks.9 Nasal mucosal infection and the host’s subsequent inflammatory response cause vasodilation and increased vascular permeability. These events result in nasal obstruction and rhinorrhea, whereas cholinergic stimulation prompts mucus production and sneezing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree