Chapter 49 Abuse and Neglect
An attentive emergency nurse undresses the one year old for examination of symptoms related to a runny nose and cough. During her assessment, she identifies round marks about the size of a dime that look like burns. Her assessment and documentation may have saved the life of this child who was not only being burned with cigarettes, but also was not consistently fed. The child is now 11 years old, thriving in his adoptive home, because of the assessment and intervention of an emergency nurse. This child was just one of the estimated 872,000 children in the United States that are identified as victims of abuse and neglect.1
Although child maltreatment has always existed, Western culture has recognized it as a problem only since the 1962 landmark article “The Battered Child Syndrome.”2 What surprises many emergency health care workers is that most of these patients are victims of neglect rather than abuse. An estimated 3.5 million American children received an investigation or assessment by Child Protective Services in 2007.3 Of these, 22.5% were validated as maltreatment, 59% were categorized as neglect, 10.8% as physical abuse, 7.6% as sexual abuse, and 4.2% as emotional abuse.3 Data from 2007 also revealed that approximately 1760 children died because of abuse or neglect.3 More than 75% of the children who were killed were younger than 4 years of age.4
Child Maltreatment
Types of Maltreatment
Neglect
Neglect involves failure (intentional or unintentional) to provide basic needs such as food, shelter, clothing, schooling, and medical care. Figure 49-1 depicts failure to thrive as a consequence of neglect. Neglect commonly is subcategorized as follows:
• Medical: This type of neglect consists of failure to provide medical care, including immunizations, necessary surgical procedures, and emergency interventions. Cases of alleged medical neglect because of a family’s philosophical or religious beliefs may require resolution in court.
• Physical: This type of neglect exists when caregivers either fail to protect the child from harm or do not provide for basic needs.
• Emotional: The caregiver fails to maintain a nurturing environment that will meet the emotional and developmental needs of the minor. This type of neglect is difficult to recognize and define.
• Educational: Poor school attendance or failure to provide necessary specialized education constitutes educational neglect.
• Mental health: Caregivers may fail to obtain necessary care for a child with emotional or behavioral problems.
Sexual Abuse
According to the American Academy of Pediatrics, sexual abuse “occurs when a child is engaged in sexual activities that he or she cannot comprehend, for which he or she is developmentally unprepared and cannot give consent, and/or that violate the law or social taboos of society.”6 Abusive behaviors may be violent, coercive, or even nontouching (e.g., pornographic photography).
Emotional Abuse
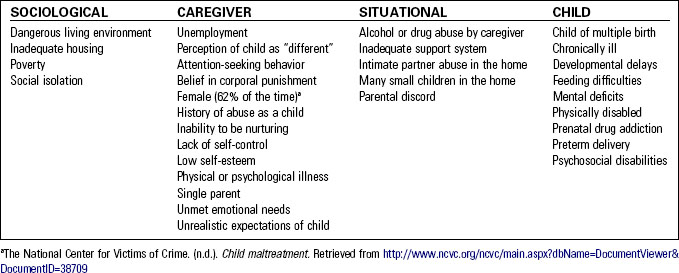
Unlike emotional neglect, in which the child’s needs are simply not met, emotional abuse is deliberate. In reality, it may be difficult to draw a distinction between the two. Table 49-1 lists emotionally abusive strategies used by abusers and common responses to abuse. Table 49-2 describes factors that contribute to child maltreatment.
| ABUSIVE ACTION | CHILD’S RESPONSE |
|---|---|
| Verbal abuse | Withdrawal |
| Verbal threats | Eating disorders |
| Constant criticism | Head banging |
| Unreasonable and outrageous expectations | Rocking Learning difficulties Enuresis Suicidal behavior Self-destructive or risk-taking behaviors |
| Use of child to manipulate other adults | |
| Extreme behaviors (anger, passivity) | |
| Lack of affection toward child | |
| Use of the child as a bargaining tool between parents |
Duty to Report
The duty of health care providers to report actual or suspected child maltreatment exists in all 50 states. Local law enforcement or child welfare agencies must be notified of any suspicion of abuse or neglect. Persons who disclose suspected maltreatment in good faith are immune from prosecution. Refer to Chapter 1, Legal Issues for Emergency Nurses, for a more detailed discussion of the responsibilities and ramifications associated with duty to report. Be sure to document to whom this information was transmitted and the date and time the information was relayed. Importantly, the reporter is under no obligation to prove the allegation but only to describe it. Abuse laws vary from state to state; become familiar with regulations in your practice area. Reporting procedures also vary by institution. Know how to access facility-specific protocols.
In general, the following information should be included in a maltreatment report:
• The child’s name (and any other names the child may be using)
• The child’s address and telephone number
• Where the child is now living (if this is different from the stated address)
• The names of the child’s parents or other caregivers
• The reasons for your suspicions
• The alleged cause of injury or the nature of the neglect
• The circumstances surrounding the incident
• Where the alleged incident occurred
• A description of the child, including any injuries or other signs of maltreatment
• The extent of abuse or neglect
• The name or any description of the suspect
• The suspect’s address and telephone number
• The name, work address, and work telephone number of the person making the report
Signs and Symptoms of Child Maltreatment
Behavioral Signs
Behavioral signs of child maltreatment include the following:
• The caregiver delays seeking treatment for illness or injury in the child
• The caretaker is also a child
• Evidence of caregiver ignorance or carelessness exists
• Descriptions of events are confusing, conflicting, ever-changing, or improbable
• The caregiver focuses on the child’s behavior instead of the child’s injury or presenting illness
• The caregiver denies knowledge of how the injury occurred
• A change in caregivers has occurred recently
• The caregiver emphasizes unimportant details or minor problems not directly related to the present situation
• The caregiver focuses on self-absorbed concerns rather than on the needs of the child
• The caregiver bypassed a closer emergency department to seek treatment
• Tension or outright hostility exists between caregivers
• Caregivers exhibit tension, hostility, or aggressiveness toward emergency department staff members
• The caregiver is uncooperative and demanding
• The child has a history of multiple emergency department visits
• Caregivers describe the child as clumsy or accident prone
• The child exhibits low self-esteem
• The child displays attention-seeking behavior
• The caregiver lacks any sense of guilt, remorse, or culpability for the incident (rather than the caregiver stating, “If only I had …”)
• The child appears fearful of adults or is unusually unafraid
• The child is fearful of the caregiver
• The caregiver displays anger toward the child regarding the injury or illness
• Answers to questions are vague
• The caregiver refuses to leave a verbal child alone with health care providers
• The child’s age (chronological or developmental) does not correlate with the reported history of injury
Physical Manifestations
The list of physical manifestations suggestive of abuse or neglect is extensive. Table 49-3 describes many possible assessment findings. Figures 49-2 to 49-4 provide examples of retinal hemorrhage, cigarette burns, and pattern bruises related to abuse.
TABLE 49-3 POSSIBLE MANIFESTATIONS OF PHYSICAL ABUSE AND NEGLECT
| AREA OR INJURY | MANIFESTATIONS |
|---|---|
| Fractures | |
| Head | |
| Ear, eye, nose | |
| Throat | |
| Burns | |
| Bruising | In various stages of healing |
| Ecchymosis | In the shape of identifiable objects (hand print, extension cord, belt buckle) |
| Lacerations | Human bite marks |
| Genitalia and perineal | Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|