Chapter 97
Abdominal Trauma 
The initial assessment of trauma patients is described in Chapter 96, and this chapter focuses on traumatic abdominal injuries.
Initial Assessment
Many patients have absolute indications for surgery that are apparent early in the evaluation (Box 97.E1).
Most instances of hypotension in the immediate peri-trauma period should be treated aggressively with volume, using saline or blood products as needed. Although a secondary survey is always necessary, in the setting of life-threatening injuries requiring immediate transfer to the operating room, the exam may have to be delayed until the patient arrives to the intensive care unit (ICU). On arrival to the ICU and after the patient is hemodynamically stable, it is imperative to review all identified injuries and complete the physical exam and diagnostic workup. The tertiary survey should also be performed in the ICU, generally within 24 to 48 hours after admission to identify any missed injuries. In severely injured patients, the secondary survey is often hindered by life-threatening priorities, and a missed injury rate of 0.3% to 12% has been reported. Although these missed injuries are rarely life threatening, they may be clinically debilitating and can significantly impact the patient’s long-term outcome.
Diagnostic Evaluation of the Patient with Blunt Abdominal Trauma
In the hemodynamically stable patient with blunt abdominal trauma, additional diagnostic studies are often necessary to assess the need for less urgent operative intervention. The choice of study may depend on the availability of equipment, the information sought, and the preference of the clinician (Table 97.1). Diagnostic evaluation, however, should never delay operative intervention in patients with a clear indication for urgent abdominal exploration.
TABLE 97.1
Comparison of Utility of Diagnostic Modalities
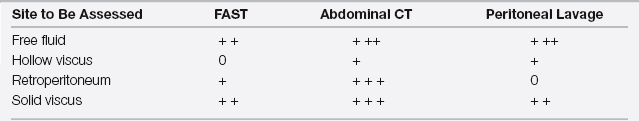
0, no utility; +, fair utility; + +, good utility; + + +, excellent utility.
FAST, Focused Assessment of Sonography for Trauma; CT, computed tomography.
Computed Tomography
The advent of computed tomography (CT) has revolutionized the care of patients with abdominal trauma. In addition to identifying the presence of intra-abdominal fluid or air, established criteria allow one to grade the severity of solid organ injury based on the CT findings, thereby helping to determine the necessity of laparotomy. CT also readily visualizes the retroperitoneum, including genitourinary and major vascular structures, as well as osseous structures such as the bony pelvis and thoracic, lumbar, and sacral spines. Newer CT scans possess enhanced image resolution and reduced image acquisition time, rendering this modality almost indispensable in stable patients with abdominal injuries. With newer technology, the ability of CT angiograms to image the vasculature rivals conventional aortography and venography in many cases.
Ultrasonography: The Focused Assessment of Sonography for Trauma (FAST)
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



