Abdominal Trauma
Matthew D. Neal
L. D. Britt
Greg Watson
Alan Murdock
Andrew B. Peitzman
Abdominal injuries are divided into two broad categories: Blunt and penetrating abdominal trauma, based on the mechanism of injury. Expedient diagnosis and treatment of intraabdominal injuries are essential to avoid preventable morbidity and death. Since management guidelines are different for blunt and penetrating abdominal trauma, they will be discussed separately.
Blunt abdominal trauma. Common mechanisms include falls, motor vehicle crashes, motorcycle or bicycle crashes, sporting mishaps, and assaults.
Intraabdominal injuries result from:
Compression causing a crush injury
Abrupt shearing force causing tears of organs or vascular pedicles
Sudden rise in intraabdominal pressure causing rupture of an intraabdominal viscus
Evaluation
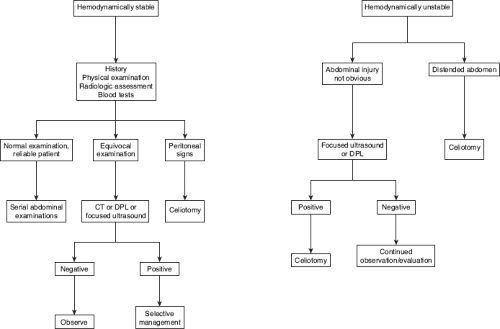
Clinical. Information regarding the mechanism of injury is essential to determine the likelihood of an intraabdominal injury (see Chapter 22). Abdominal examination after blunt trauma is often unreliable. Altered level of consciousness, spinal cord or other distracting injury, and medication or substance effects can further confound the physical examination. Although adjunctive tests are important in the evaluation of blunt abdominal trauma, careful, repeated physical examination of the patient remains essential in the early diagnosis of abdominal injury. The choice of adjunctive diagnostic tests depends, in part, on the hemodynamic stability of the patient, the associated injuries and the patient volume at the treating institution (i.e., extremely busy centers may not have the personnel to perform serial physical examinations reliably) (Fig. 29-1).
In the hemodynamically unstable patient or the patient with ongoing fluid requirements, rapid evaluation of the abdomen while the patient is in the trauma resuscitation area is mandatory. Ultrasound (focused abdominal sonography for trauma [FAST]), diagnostic peritoneal aspiration (DPA), or diagnostic peritoneal lavage (DPL) are appropriate diagnostic tools to determine the presence of hemoperitoneum; in recent years, the safety and rapidity of surgeon-performed focused ultrasound have substantially diminished the role of DPL. In the stable patient without immediate need for the operating room (OR), computed tomography (CT) is the investigation of choice.
Physical examination. Evaluation of the patient will often uncover signs of hypoperfusion (e.g., obtundation, cool skin temperature, mottling, diminished pulse volume, or delayed capillary refill), which should initiate a search for a source of blood loss. Factors associated with abdominal injury requiring laparotomy include chest injury, base deficit, pelvic fracture, or hypotension in the field or trauma resuscitation area.
Evaluation of the abdomen may detect distension or signs of peritoneal irritation (usually associated with injury to a hollow viscus). On the other hand, blood in the peritoneum often does not produce peritoneal signs, and massive hemoperitoneum may be present without abdominal distension.
Commonly injured abdominal organs are generally solid organs: Liver, spleen, bowel mesentery, or kidney. If the patient is a restrained victim in a
motor vehicle crash, particularly with a visible contusion on the abdomen from a lap belt, or a lumbar vertebral body fracture (especially a Chance fracture), suspect hollow viscus injury, an injury commonly missed.
Diagnostic tests. The goal of the initial evaluation of the abdomen is to identify quickly the patient who requires laparotomy. Victims of blunt trauma with hypotension and abdominal distension or peritoneal signs should proceed immediately to laparotomy without further workup.
For patients without an obvious indication for laparotomy, various modalities are available to evaluate the abdomen further. Ancillary evaluation beyond physical examination should be considered for patients with:
Abnormal or equivocal abdominal evaluation
Concurrent injury to the chest or pelvic ring
Gross hematuria
Diminished level of consciousness
Spinal cord injury
Other injuries requiring a long general anesthetic for management, rendering repeat abdominal examination impossible.
Diminished capacity to tolerate a delay in diagnosis of abdominal injury (e.g., extremes of age)
The diagnostic test used depends upon the mechanism of injury, associated injuries, and hemodynamic stability. Remember that control of cavitary bleeding takes precedence over further diagnostic testing. Delays to control bleeding increase mortality.
Plain radiographs. The chest radiograph may reveal a ruptured hemidiaphragm or pneumoperitoneum. Plain abdominal films are rarely productive, but may show retroperitoneal gas or findings associated with abdominal injury (e.g., fractures of the lumbar spine or lower rib cage).
Laboratory evaluation. Patients with blunt injury received promptly from the scene may not be anemic or acidotic on presentation. Similarly, amylase levels can be normal with significant pancreatic or intestinal injury, or can be elevated from extra-abdominal injury such as head and neck trauma.
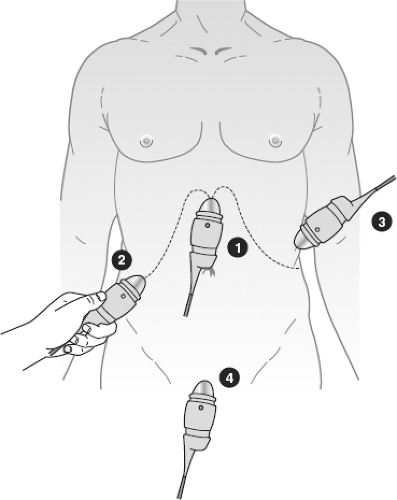
Focused assessment by sonography in trauma (FAST) is a rapid, noninvasive means to identify hemoperitoneum in the trauma resuscitation area and, as such, has replaced DPL in many centers (Fig. 29-2).
Indications include a hemodynamically unstable patient without obvious indication for laparotomy; any patient requiring prompt transfer to the OR for nonabdominal cause; or use as a screening test for all others requiring abdominal evaluation.
Contraindications include obvious need for laparotomy or lack of FAST expertise.
Accuracy. Sensitivity and specificity (60% to 85%) are generally less than those of CT in detection of hemoperitoneum. It is not accurate for the detection and anatomic characterization of solid organ injury. FAST is most valuable when positive in the hemodynamically unstable patient; prompt transfer to the operating room is thus facilitated. On the other hand, with a false-negative rate as high as 40%, a negative FAST should generally be followed by a more definitive diagnostic test (CT or DPL) in the patient incurring high-energy injury.
Advantages. Ultrasound is rapid and noninvasive; no need to transfer the patient to the radiology suite; can be performed by a trained member of the trauma team; can be repeated; is less expensive than CT.
Disadvantages. Can miss solid organ injury in the absence of hemoperitoneum or small amounts of hemoperitoneum; cannot distinguish between ascites, succus entericus and blood; requires specialized training and competency; and is difficult to interpret in the obese or patients with extensive subcutaneous emphysema.
Technique of FAST. A 3 to 5.0 MHz transducer is placed in the subxiphoid region in the sagittal plane to set the machine gain. Sagittal views of
Morison’s pouch and the splenorenal recess are performed, followed by a pelvic transverse view. Free fluid appears anechoic (black) compared with the surrounding structures.
CT can evaluate solid organ injury; intraabdominal fluid, blood, air; and retroperitoneal organ injury in hemodynamically stable patient suspected of intraabdominal injury. CT of the abdomen and pelvis (upper abdominal cuts will show caudad pulmonary parenchyma and may reveal occult pneumothorax; pelvic cuts may reveal dependent hemoperitoneum) should be obtained, using intravenous (IV) contrast, and currently less so, oral contrast.
Indications. Hemodynamically stable patients requiring abdominal evaluation
Contraindications. Hemodynamically unstable patients or those with an obvious need for laparotomy
Accuracy. Recent experience with modern high-resolution CT technology shows accuracy rates of 92% to 98%. Hollow viscus and pancreatic injuries are those most likely to be missed by CT.
Advantages
Noninvasive
Reveals solid organ injury with anatomic characterization
Estimates free fluid volume
Provides assessment of retroperitoneal injuries
Disadvantages
Need for specialized personnel
Cost
Time
Radiation
Not an ideal environment for ongoing evaluation and resuscitation
Variable reliability in detection of hollow viscus injury and pancreatic injury
Intravenous contrast
DPL, a rapid and accurate modality for the diagnosis of intraabdominal injury in blunt trauma victims, has been supplanted by ultrasound at most centers for the rapid evaluation of the hemodynamically unstable patient. Briefly, a catheter is placed into the peritoneal cavity for aspiration of blood or fluid. If this is negative, a liter of warmed normal saline solution is infused (or 10 mL/kg in children) into the abdomen and allowed to drain by gravity. The effluent is sent for laboratory analysis.
Criteria for positive DPL
10 mL gross blood on aspiration
>100,000 red blood cells/mm3
>500 white blood cells/mm3
Bacteria
Bile
Food particles
Indications in general are as for FAST, but the utility of FAST has limited the benefit of DPL to situations where the rapid determination of the nature of free intraabdominal fluid is necessary, such as the patient with FAST- or CT-documented intraperitoneal fluid in the absence of solid organ injury, particularly if physical examination is unreliable for the diagnosis of peritonitis.
Contraindications are obvious need for laparotomy, previous abdominal operations (relative), pregnancy, or pelvic ring fracture (relative, may be performed supraumbilically).
Accuracy. The sensitivity and specificity of DPL approach 95%. The false-negative rate is 4%.
Advantages. DPL is quick, accurate, sensitive, and low cost.
Disadvantages. DPL is invasive and results in nontherapeutic laparotomy in 15% to 27%. DPL can fail to detect diaphragmatic or retroperitoneal injury.
Technique. DPL can be performed in an open or closed technique. In the open technique, skin, subcutaneous tissue fascia, and peritoneum are incised under direct vision for catheter insertion. Seldinger technique is used for the closed method. Pre-DPL gastric and urinary bladder drainage are mandatory, regardless of the technique utilized.
DPA has been used in lieu of DPL at many centers. This is a rapid technique to simply determine the presence of gross hemoperitoneum. Ironically, DPL evolved in 1965, because of the inaccuracy of DPA. Certainly, a grossly positive aspiration is useful information. The false-negative rate of DPA is not well defined in the literature.
Penetrating abdominal trauma is usually by gunshot wound (GSW) or stab wound. The likelihood of injury requiring operative repair is higher for abdominal GSW (80% to 95%) than for stab wounds (25% to 33%) and the management algorithms differ. Abdominal organs commonly injured with penetrating wounds include small bowel, liver, stomach, colon, and vascular structures. Any penetrating wound from the nipple line anteriorly or scapular tip posteriorly to the buttocks inferiorly can produce an intraperitoneal injury.
Gunshot injury. In most instances, patients sustaining transperitoneal GSWs to the abdomen require laparotomy as their diagnostic and therapeutic modality.
Physical examination. Carefully inspect the patient to avoid missing wounds. Bullets that do not strike bone or other solid objects generally travel in a straight line. Trajectory determination is the key to injury identification. Hemodynamically unstable patients with abdominal GSW should not have extensive evaluation before celiotomy. Carefully examine the patient paying special attention to the body creases, perineum, and rectum. Bullet wounds should be counted and assessed. An odd number of wounds suggest a retained bullet; elongated wounds without penetration typify graze injuries. Palpate the abdomen for signs of tenderness. A neurologic examination should be performed to exclude spinal cord injury.
Plain radiographs assist in determining trajectory. Mark cutaneous bullet wounds with radiopaque markers. In addition, the presence of pneumoperitoneum, spinal fractures, pneumo-, or hemothorax can be appreciated.
CT has a limited role in the evaluation of patients with abdominal GSW. However, in the hemodynamically stable patient in whom it is questioned, peritoneal penetration can be excluded by visualizing the path of the bullet on CT. If any doubt exists, laparotomy or laparoscopy is mandatory. In addition, selected patients with right upper-quadrant GSW isolated to the liver may be candidates for nonoperative management (NOM).
FAST, similarly, has a limited role in evaluation of abdominal GSW. It can be useful to assess the pericardium or assist in operative planning in hypotensive patients with multi-cavity wounds.
Laparoscopy can be useful in assessing hemodynamically stable patients with tangential GSW, especially in the thoracoabdominal region.
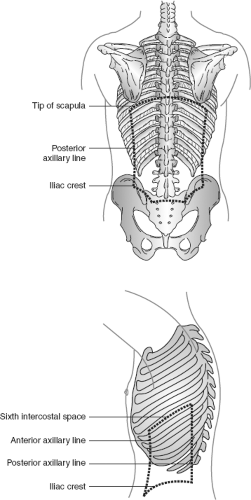
Stab wounds. Indications for immediate exploration include hypotension, peritoneal signs, and evisceration. If these are not present, a selective management approach is justified. Anterior stab wounds refer to those in front of the anterior axillary line. One-third is extraperitoneal, one-third is intraperitoneal requiring repair, and one-third is intraperitoneal not requiring visceral repair. Flank stab wounds lie between the anterior and posterior axillary lines from the scapular tip to the iliac crest. Back stab wounds are posterior to the posterior axillary line (Fig. 29-3). Abdominal organs are at risk with thoracic wounds inferior to the nipple line anteriorly (ICS 4) and scapular tip posteriorly (ICS 7).
Serial examination (selective management) can be used to detect the development of peritoneal signs in a hemodynamically stable patient. The same surgeon should repeat abdominal examinations also documenting temperature, pulse rate, and white blood count.
Local wound exploration can be performed in the trauma resuscitation area on patients without indication for operation after anterior abdominal stab. The skin is prepared and anesthetized and the original wound is enlarged. Exploration is considered positive if anterior fascial penetration is observed. Patients with positive local wound explorations progress to laparoscopy or laparotomy.
CT with triple contrast (oral, IV, and rectal) can be used to evaluate back and flank SW with a sensitivity of 89%, specificity of 98%, and accuracy of 97%. CT is not very helpful in the evaluation of anterior abdominal stab wounds, especially in thin patients with slight abdominal musculature.
FAST is minimally useful in the workup of stable patients with abdominal stab wounds. If positive, visceral injury can be inferred.
DPL can be performed to evaluate abdominal stab wounds. The criteria for red blood cell (RBC) counts are generally lower than that for patients with blunt injury (i.e., 1,000 vs. 100,000/mm3). Lower threshold values will improve the sensitivity of the modality, but increase the negative or nontherapeutic laparotomy rate.
Shotgun wounds. Close-range shotgun wounds are high-velocity injuries. As such, they can result in blast and penetrating abdominal wounds. Shotgun wounds with peritoneal penetration mandate laparotomy. Those delivered from a distance can be evaluated with CT to determine peritoneal penetration by pellets.
Impalement injuries. The impaled object is secured in place and removed in the OR under direct visualization with the abdomen open.
Conduct of an exploratory laparotomy. Refinements in diagnostic capabilities have allowed a more selective application of laparotomy, reducing the number of nontherapeutic laparotomies.
Indications for exploratory laparotomy. Performed on the basis of physical examination findings or on the results of diagnostic tests.
Clinical
Obvious peritoneal signs on physical examination
Hypotension with a distended abdomen on physical examination
Abdominal GSW with peritoneal penetration
Abdominal stab wound with evisceration, hypotension, or peritonitis
Diagnostic tests
Positive FAST with hemodynamic instability or DPL
Findings with any other diagnostic intervention (e.g., chest x-ray [ruptured diaphragm, pneumoperitoneum], abdominal ultrasound, abdominal CT, or laparoscopy suggestive of an intraabdominal injury requiring repair)
General setup
An OR appropriately stocked with appropriate anesthesia, nursing, and support staff should be immediately available 24 hours a day.
Once the decision is made to operate, the patient must be rapidly transported directly to the OR with appropriate airway support personnel, trauma team surgeons, and trauma team nursing staff in attendance. This is direct transfer to the operating room—not the preoperative holding area.
If possible, informed consent is obtained from the patient or relative before laparotomy. This is not always possible or practical; the operation should proceed without delays to obtain consent in life-threatening circumstances.
Intravenous lines, tubes, and spinal precautions
The patient should already have at least two large-bore IVs placed; other IV and arterial access can be placed as necessary in the OR. Control of cavitary bleeding should not be delayed by attempts at fluid resuscitation.
Administer broad-spectrum, Gram-negative, and anaerobic antibiotic coverage (e.g., an extended spectrum penicillin or a third-generation cephalosporin).
Place chest tubes to underwater seal, not clamped, during transport and to suction drainage on arrival in the OR. Place the canisters where they are readily visible and blood loss from the chest tubes can be observed.
Place nasogastric or orogastric tube and a bladder catheter before laparotomy. No procedure should be performed in such a way as to delay control of bleeding and contamination.
Move the patient onto the operating table with appropriate cervical spine and thoracolumbar spine precautions; in many cases, spinal injury will not be excluded before arrival in the OR. If the patient is still immobilized on a backboard, logroll the patient and remove the board before beginning the operation. Occult penetrating wounds must be sought before beginning laparotomy.
Sequential compression devices can be used for hemodynamically stable patients, if readily available.
Rapid-infusion system. Prime the infusion system to infuse blood products and “cell-saved blood” quickly via large-bore lines before the incision releases the tamponade. Ascertain that packed RBC are in the OR and plasma and platelets are available for the patient with active hemorrhage. In the exsanguinating patient, the massive transfusion protocol should be activated to facilitate availability of blood products.
Preparation of the patient. The patient is shaved (if time allows), and the entire anterolateral neck (remove anterior portion of cervical collar and then sandbag to maintain cervical spine immobilization), chest to the table bilaterally, abdomen, groin, and thigh region (to the knees bilaterally) are prepared and draped in sterile fashion (see Fig. 17.1).
Initial goals. Stop bleeding and control gastrointestinal contamination. The exploratory laparotomy for trauma is a sequential, consistently conducted, operative procedure.
Incision. For urgent laparotomy, a generous midline incision is preferred. Alternative abdominal incisions can be useful for known injuries in stable patients. Adequate exposure is critical. Self-retaining retractor systems and headlights are invaluable.
Bleeding control. Scoop-free blood and rapidly pack all four quadrants to control bleeding as a first step. With blunt injuries, the likely sources of bleeding are the liver, spleen, and mesentery. Pack the liver and spleen, and quickly clamp the mesenteric bleeders. With penetrating injuries, the likely sources of significant bleeding are the liver, retroperitoneal vascular structures, and mesentery, based on trajectory of the weapon or bullets. Pack the liver and retroperitoneum, and quickly clamp mesenteric bleeding vessels. If packing does not control a bleeding site, this source of hemorrhage must be controlled as the first priority.
Contamination control. Quickly control bowel content contamination using Babcock clamps, Allis clamps, a stapler, rapid temporary sutures, or ligatures.
Systematic exploration. Systematically explore the entire abdomen, giving priority to areas of ongoing hemorrhage to definitively control bleeding:
Liver
Spleen
Stomach
Right colon, transverse colon, descending colon, sigmoid colon, rectum, and small bowel, from ligament of Treitz to terminal ileum, looking at the entire bowel wall and the mesentery
Pancreas, by opening lesser sac (visualize and palpate)
Kocher maneuver to visualize the duodenum, with evidence of possible injury
Left and right hemidiaphragms and retroperitoneum
Pelvic structures, including the bladder
With penetrating injuries, exploration should focus on following the track of the weapon or missile.
Injury repair (section V)
Closure
Running non-absorbable or absorbable monofilament suture (e.g., No. 1 nylon or No. 1 looped absorbable suture)
Leave skin open with delayed secondary closure if there is contamination or shock
If gross edema of abdominal contents precludes closure, absorbable mesh, sterileIV bags, or intestinal bags can be used with moist gauze and an impermeable dressing (e.g., Op-Site, VAC dressing) to prevent possible abdominal compartment syndrome. Recognize the combination of complex injuries (often liver, pelvis, or major vascular injury) and physiologic signs (“the lethal triad”: Hypothermia, acidosis, and coagulopathy) that dictate abbreviated laparotomy (damage control).
V. Specific Organ Injuries
Treatment of an organ injury is similar whether the injury mechanism is penetrating or blunt. An exception to the rule is a retroperitoneal hematoma. Explore all retroperitoneal hematomas caused by penetrating injury.
Diaphragm
The diaphragm, a dome-shaped muscular structure with an aponeurotic sheath (“central tendon”), effectively separates the thoracic and abdominal cavities. It attaches to the first three lumbar vertebrae, the ribs, and the posterior aspect of the lower sternum. Because of the decussation of its crura and hiatal architecture, the diaphragm provides an avenue for many vital structures, including the aorta, esophagus, thoracic duct, vagus nerves, azygos vein, and the inferior vena cava. Physiologically, the wide excursion of the diaphragm during inspiration and expiration contributes to both respiratory function and venous return.
Blunt Injury
Blunt trauma accounts for up to 30% of diaphragmatic ruptures in the United States. Motor vehicle collisions and falls from heights are the most common mechanisms of injury. Diaphragmatic rupture occurs as a result of an acute increase
in the intraabdominal pressure. Right-sided diaphragmatic ruptures occur less frequently than those on the left.
Penetrating Injury
Table 29-1 Absolute Indication for Celiotomy/Thoracotomy
- Hemodynamic lability
- Peritoneal signs
- Free air
- Bleeding from an orifice
- Massive hemothorax (thoracotomy required)
Chest tube >1,500 cc initial output
Chest tube >200 cc/h for more than 4 h
- Impaled object
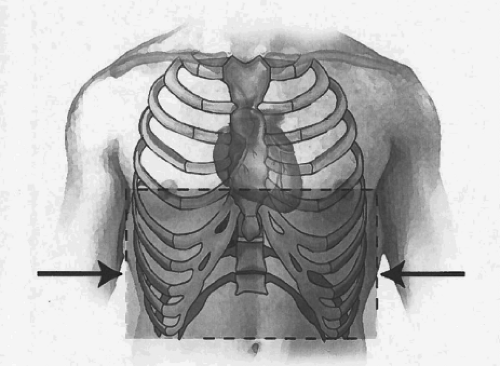
In addition to excluding possible cardiac injury if the penetrating wound is more central, the paramount reason that the thoracoabdominal region (Fig. 29-4) presents such a diagnostic challenge to the acute care surgeon is the possibility of an occult diaphragmatic injury. Patients who are hemodynamically labile or have peritoneal signs require mandatory exploration. Clinically stable patients should undergo a more selective approach. No conventional diagnostic modality consistently makes the definitive diagnosis of diaphragmatic injury. Making the diagnosis of a diaphragmatic injury is important for two reasons. First, the presence of an acute injury to the diaphragm mandates abdominal exploration with high risk for an associated intraabdominal injury. Second, there are risks, both acutely and long-term, of diaphragmatic herniation and possible incarceration/strangulation. Because of this diagnostic challenge, the thoracoabdominal region was correctly underscored as “the ultimate blind spot” in penetrating trauma. Patients who present with indications for exploration (Table 29-1) require no essential
diagnostic studies. An expectant approach (observation only) does not address potential for the presence of an injury to the diaphragm and its sequela, such as the increased risk for the development of a herniation of abdominal viscera. Although the injury occurs acutely, clinical signs of a hernia are usually lacking and a “high index of suspicion” is imperative to prompt optimum investigation. The time from injury to presentation of a symptomatic diaphragmatic hernia may vary from days to years postinjury. The patient may present with signs and symptoms of bowel obstruction or even peritoneal signs due to necrosis of the incarcerated bowel; mortality rate is high in this setting. This further emphasizes the importance to diagnose and repair these injuries in the acute setting.
- Hemodynamic lability
Several diagnostic modalities have been used in the evaluation of thoracoabdominal trauma in both the blunt and penetrating settings.
Chest x-ray is the usual screening diagnostic modality. However, the diagnostic accuracy for diaphragmatic injury ranges from 13% to 94%. The accuracy may increase when the CXR is repeated after the placement of a radiopaque nasogastric tube.
Computed tomography has a sensitivity of 63% and a specificity of 100% for diaphragmatic “rupture” with blunt injury. Computed tomography fails to diagnose diaphragmatic injuries without associated visceral herniation. Patients with penetrating injuries are less likely to have visceral herniation and, therefore, their injuries can easily be missed on CT.
Diaphragm injury as a result of penetrating trauma ranges from 0.8% to 15%. Mandatory exploration of all penetrating thoracoabdominal injuries has been advocated for many years on the premise that it is the only way to assess definitively the diaphragm. Adequate visualization is critical, considering the increased morbidity and mortality as a result of a missed diaphragmatic injury.
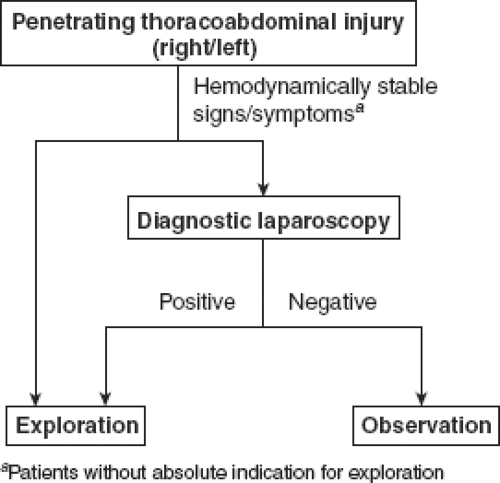
However, mandatory celiotomy for an injury with such a low incidence results in a high number of nontherapeutic explorations, prompting the need for an alternative approach. Thus, diagnostic laparoscopy has been applied as the definitive modality for identification of diaphragmatic injury in penetrating thoracoabdominal trauma. In the acute setting of penetrating thoracoabdominal injuries, there are few (if any) indications for diagnostic thoracoscopy to determine the integrity of the diaphragm. Such an intervention would likely require a double-lumen endotracheal tube insertion and lateral decubitus positioning of the patient. Diagnostic laparoscopy is more appropriate and efficient management for these injuries. The ability to evaluate adequately the diaphragm with the laparoscope provides an attractive diagnostic modality that benefits those patients with diaphragmatic injury and avoids an unnecessary celiotomy.
Table 29-2 Diaphragmatic Injury
Organ
Incidence
Diagnosis
Specific management
Outcome
Diaphragm
6% of all intraabdominal injuries resulting from penetrating trauma
- Physical examination: Chest pain and shortness of breath Scaphoid abdomen Bowel sounds on auscultation of the hemithorax
- Plain radiography Hollow viscus noted in the left hemithorax Nasogastric tube in the left hemithorax
- FAST examination Unreliable
- DPL Inconclusive; high false-negative
- CT scan Inconclusive
- Laparoscopy, the diagnostic modality of choice
- Preoperative antibiotics
- Primary closure is the preferred definitive management
- With documentation of a diaphragmatic rent (laceration), exploratory laparotomy is necessary
- Associated injuries dictate morbidity and mortality
Treatment
In the acute setting, diaphragmatic injury is preferentially repaired primarily with a heavy non-absorbable suture. Although the indications are infrequent, a non-absorbable mesh can be incorporated in the diaphragmatic closure where there is significant tissue destruction, which usually occurs in blunt trauma. In the event of a gross contamination, endogenous tissue can be utilized for a definitive repair. Such tissue includes a latissimus dorsi flap, tensor fascia lata, or omentum. There are some who advocate using biologic tissue grafts, such as AlloDerm (human acellular tissue matrix; Life Cell Corporation). The durability of such a repair is questionable. Irrigate the thoracic cavity through the defect in the diaphragm; leave a chest tube. Figure 29-5 is a treatment algorithm for penetrating thoracoabdominal injury, the most common mechanism for diaphragmatic injury.
Outcomes
Overall, the expected outcomes for diaphragmatic injuries are good (Table 29-2). Mortality and significant morbidity are related to associated organ injury.
Stomach
The stomach is the second most common intraperitoneal hollow viscus injury. Its size and intraperitoneal location makes this organ a vulnerable target, with size being affected by the intraluminal volume. Gastric injury secondary to blunt trauma
is infrequent. When it does occur, it is often the result of increased intraluminal pressure and distension; seat belt injuries and direct blows to the epigastrium are common causes. Penetrating wounds of the stomach are a more frequent mechanism of injury; the anterior and posterior aspects of the stomach need to be meticulously inspected for through-and-through injuries. Injury of the stomach should be repaired
primarily after debridement of nonviable edges. The primary repair can be performed in either a single layer with non-absorbable suture or as a double-layer closure with an absorbable suture with the first layer and the second layer with non-absorbable sutures (e.g., silk). It is unlikely that primary repair of a through-in-through stomach injury would compromise the gastric lumen. It is uncommon that gastric injuries require a major resection. Since gross contamination is usually associated with stomach wounds, copious irrigation of the abdominal cavity is an essential component of the operative strategy.
Small Intestine
Small bowel wounds are the most common intraperitoneal hollow viscus injury. As with other hollow viscus injuries, there is no place for NOM of a small bowel perforation or rupture.
Table 29-3 CT Findings of Blunt Bowel Injury
Direct
Indirect
Oral contrast extravasation
Mesenteric hematoma
Free air
Mesenteric blush
Bowel wall edema
Unexplained free fluid
Fat streaking
Unopacified (vascular contrast media) bowel loops
The small bowel is commonly injured from penetrating trauma; 5% to 15% of small bowel injury is as the result of blunt trauma. CT evaluation can be helpful in detection of a possible blunt bowel injury. There are two basic types of findings of bowel injury on CT: Direct and indirect (Table 29-3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree