Fig. 46.1
Edmund Andrews. (Photograph of portrait, Feinberg School of Medicine Library, courtesy of the EIE collection)
The First Half of the Twentieth Century
The first half of the twentieth century saw the discovery of several new inhaled anesthetics, most being but marginal improvements on ether. Consider ethylene, or ethene, the first member of the alkene series (C2H4), the polymer being polyethylene. In 1908, growers noted that carnations failed to flower in greenhouses where there had been a leak of ethylene, used for illumination. The expression ‘go to sleep’ was used to describe the condition of the ethylene contaminated carnations. This chance finding that ethylene induced ‘sleep’ in carnations prompted Arno Luckhardt to trial its use as an anesthetic. Ethylene entered clinical practice around 1923 [35]. As it was more potent than nitrous oxide, and thus could be administered with greater oxygen concentrations, it transiently became popular in the US. However, ethylene is highly flammable and by the early 1930s, several explosions had occurred. This, along with the introduction of the more potent cyclopropane, caused its use to wane. However, Eger remembers with awe, a presence of history while giving ethylene at Chicago’s Presbyterian Hospital in the early 1950s for emergency surgery. The Presbyterian Hospital was the site of the first use of ethylene in patients.
Cyclopropane’s introduction as a general anesthetic was also initiated by a chance finding. Cyclopropane was synthesized in 1882. George Lucas and Velyien Henderson in Toronto thought that a contaminant of a cylinder of propylene might have resulted in toxic reactions. Two kittens put in a jar with the contaminant, cyclopropane, were anesthetized and recovered uneventfully [36]. Henderson was the first human subject anesthetized with the gas. Cyclopropane had several advantages. It was potent, having a MAC of approximately 10% [37]. Because of its potency, poor blood solubility, and lack of irritant properties, it induced anesthesia quickly. It did not depress the heart; in fact it increased blood pressure. However, it could explode, it caused the heart to sometimes beat irregularly, and it depressed breathing. Indeed, as early as 1956, the Ministry of Health in the UK set up a working party to investigate fires and explosions associated with anesthesia and reported a total of 36 explosions and three deaths between 1947 and 1954. These limitations and the advent of the nonflammable halothane eventually led to the abandonment of cyclopropane. However, as late as the 1980s, it continued to be used, especially in children, and in patients who needed support of their blood pressure. Eger remembers in the 1960s, promising volunteers that if they would breathe 10 breaths of 50% cyclopropane they would fall asleep by the tenth breath. He lied. They all fell asleep by the third breath.
Vinethene (Vinesthine, Vinydan), the commercial name for divinyl ether (CH2CH-O-CHCH2), was the first inhaled anesthetic developed with some notion of a relationship of structure to activity (a precedent sometimes, erroneously in my opinion, accorded halothane). Leake and Chen deliberately combined the advantageous properties of ether (high potency) and ethylene (absent pungency and low solubility), substituting two ethylene moieties for the two ethane moieties in ether to produce divinyl ether [38]. Its primary advantage was that it was one-quarter as soluble in blood as ether [39]. It was used for approximately 40 years, particularly to smooth the induction of anesthesia with ether. Larry Saidman remembers that it was still in use for this purpose in the early 1960s. He recalls that some skill was needed to hold both the divinyl ether bottle and the ether can in the right hand and maintain the airway with the left hand all the time using an open drop ether mask!
In the late 1930s, the degreasing and dry cleaning agent, trichloroethylene (CCl2CHCl) or Trilene, was introduced as an anesthetic by the London anesthetist Langton Hewer, finding favor mostly in the UK [40]. It had been sniffed illicitly by thrill seekers and had found a place in medicine as a treatment for trigeminal neuralgia. Trilene possessed innate analgesic properties, and was inexpensive and easy to administer. Perhaps most attractive, it was non-explosive, a particular advantage because of the increasing use of electrocautery by surgeons to stop bleeding. But Trilene produced a high incidence of postoperative nausea and vomiting and had the potential to be hepatotoxic. It had to be used in an open (high-flow) system because it reacted with carbon dioxide absorbents to produce the nerve gas phosgene. Nevertheless, Trilene continued to be used by cost conscious anesthesiologists for many years after the introduction of halothane.
Changes in society in the early part of the twentieth century drove the search for improved inhaled anesthetics. Doctors wanted to improve the patient experience during and after surgery, and patients expected more. Anesthetics used before World War II were toxic (especially chloroform and Trilene), associated with postoperative nausea and vomiting (all anesthetics), or explosive (ether, ethylene, cyclopropane, Vinethene), or had a combination of these unwanted effects. Nitrous oxide caused nausea and vomiting, had a subtle toxicity, and lacked sufficient potency to produce surgical anesthesia. Chloroform use provided an example of how prevailing societal attitudes influenced anesthetic use. Although chloroform was easy to use, produced a pleasanter induction than ether, and was non-explosive, death from cardiovascular side effects or liver or renal injury were relatively common. As the twentieth century advanced, ‘patient safety’ became a concern of doctors and of society in general. Litigation motivated some of the changes. Chloroform continued to be used commonly in the UK and the Southern US, as opposed to the Northern US where litigation was increasingly an issue. Indeed, I’m unaware of any British anesthetist being sued following a chloroform-induced death even though the jury at Hannah Greener’s inquest clearly believed that chloroform caused her demise.
Even before World War II, we knew where to search for a better inhaled anesthetic. In a prophetic introduction to their studies on fluorine derivatives of chloroform in 1932, Harold Booth and E May Bixby of Western Reserve University in Cleveland stated: “A survey of the properties of 166 known gases suggests that the best possibility of finding a new non-combustible anesthetic gas lay in the field of organic fluoride compounds. Fluorine substitution for other halogens lowers the boiling point, increases stability and generally decreases toxicity [41].” Every time I read this, especially the last sentence, I marvel at Booth and Bixby’s perspicacity. We knew what should be done, but the great electronegativity and reactivity of fluorine made it difficult to study, and we lacked sufficient expertise in its control in the 1930s. Then war broke out, and we found the expertise.
Advances in Fluorine Chemistry During World War II
Scheele identified fluorine in 1771, but it was not isolated until 1886 because fluorine is the most electronegative of all elements, and is very reactive. Like all halogens (five non-metallic elements which form simple salts like sodium chloride or table salt’the word ‘halogen’ derives from the Greek ‘salt producing’) fluorine is not found in the free state in nature. Chemists in the 1930s could synthesize but few fluorine-containing compounds that might have anesthetic activity.
Two military goals greatly advanced fluorine chemistry, and led to the synthesis of the first fluorinated anesthetic, methoxyflurane. First, the huge increase in demand for high octane aviation fuel necessitated production of a catalyst’hydrogen fluoride. Second, in 1942, the best chemists available in the US were recruited to the Manhattan Project to develop the atomic bomb containing the fissile U[235]isotope of uranium. U[235]had to be separated from its natural, non-fissile isotope, U[238]. To do this required making the uranium volatile’a gas! And that could be done by combining uranium with fluorine to make uranium hexafluoride (UF6). The rest was simple: just use a jillion centrifuges to separate U[235]F6from U[238]F6and then remove the fluorine. The atomic bomb detonated 300m above Hiroshima on 6 August 1945, contained U[235]. Thus, great advances in fluorine chemistry occurred, advances enabling the synthesis of diverse, potentially anesthetic compounds. The aphorism ‘Every evil hath its good, every sweet its sour’ was never more apposite (attributed to Oliver Wendell Holmes Jr. whose father, as previously noted, coined the term ‘anaesthesia’).
Two developments linked the Manhattan Project and fluorinated anesthetics. The first led to methoxyflurane (CH3-O-CF2-CHCl2). As part of the Manhattan Project, William Miller, Edward Fager, and Paul Griswold synthesized several fluorinated methyl ethyl ethers [42]. Methoxyflurane was synthesized in 1944 but went unnoticed. Miller and his colleagues were working for the Manhattan Project at SAM Laboratories, Columbia University, under contract number W-7405-Eng-50 and at SAM Laboratories Carbide and Carbon Chemicals Corporation, New York City under contract number W-7405-Eng-26, Supplement No 4. The details of methoxyflurane’s synthesis were published in Volume 1 of Division VII of the Manhattan Project Technical Series. I include the contract numbers to demonstrate that fluorinated anesthetics directly resulted from nuclear weapons research. I’m unaware that this has previously been noted in the anesthetic literature. Miller submitted the details of his synthesis to the Journal of the American Chemical Society, when I was six days old (submitted to JACS 30 April 1947). Ten years were to pass before its rediscovery as an anesthetic. Miller, later of Cornell University, thereby became the first to synthesize a fluorinated inhaled anesthetic. But he did not realize or pursue its anesthetic possibilities; he was pre-occupied in developing weapons of mass destruction.
Second, in a search for a better anesthetic, Earl McBee (who worked on U[235]) synthesized 46 fluorine-containing ethanes, propanes, butanes, and an ether for the Mallinckrodt Chemical Works. Mallinckrodt gave these compounds to Benjamin Robbins, the first Chairman of Anesthesia at Vanderbilt University and a member of the Pharmacology Department, to test for anesthetic activity. The Pharmacology Department at Vanderbilt had historical close links with the Mallinckrodt Chemical Works which is why Robbins was involved with their assessment. The Mallinckrodt Chemical Works manufactured ether and cyclopropane, and thus had an interest in anesthesia. The founder, Edward Mallinckrodt Jr., went to school with Paul Lamson, who became Chairman of Pharmacology at Vanderbilt. He gave his old school friend a grant of $25,000 a year, to fund research related to anesthesia.
In 1946, Robbins published his preliminary report [43]. Although no compound was a useful anesthetic, three compound structures differed but slightly from halothane. In two, a single chlorine substitution for either hydrogen or bromine would have produced halothane’as would the addition of a single fluorine and alteration of the position of chlorine in the third. The race was still on.
Julius Shukys synthesized the first fluorinated anesthetic to enter practice, an ethyl vinyl ether (CF3-CH2-O-CHCH2) named fluroxene (Vinamar, Fluoromar). John Krantz in Maryland studied it in the late 1940s [44], and it entered practice in 1953. However, it was not ideal, producing rapid breathing and heart rate, it was flammable, and it could injure the liver. Indeed, although toxicity in primates was small, it was lethal to many other species [45]! Larry Saidman also remembers its propensity to cause nausea and vomiting, hence its alternative names ‘Vomomar’ and “Fluorobarf” Had fluroxene been subjected to today’s standards, it never would have been tested in humans. The search for a better agent crossed the Atlantic back to Britain.
Chance and Science Come Together: The Story of Halothane
Imperial Chemical Industries (ICI), in Cheshire in the North of England, founded a pharmaceutical division in 1944, having previously synthesized fluorine containing compounds in the 1930s for use as refrigerants. Chance again played a crucial role. In the 1930s, John Ferguson, later to become ICI’s Research Director of the General Chemical Division, tested agrochemical agents that might be used to fumigate grain silos to rid them of weevils and beetles. Some of the agents stunned but did not kill the weevils. Remembering this in 1951, he prompted a young fluorine chemist working at ICI, Charles Suckling (with whom I have discussed the subject) to explore fluorinated compounds as anesthetics. Suckling set about searching for an anesthetic, combining the multi-perspectives of patient, surgeon, anesthetist, and manufacturer. Although Suckling synthesized and selected the compounds for testing, recognize that Ferguson’s earlier chance observations set Suckling on the road leading to the synthesis of the halogenated alkane (CF3-CHClBr) called halothane. Suckling succeeded surprisingly quickly, halothane being the ninth of twelve compounds tested for anesthetic activity [46]. Suckling then asked the pharmacologist, James Raventos, to determine the relevant pharmacology. Suckling described Raventos as: “Wise with an impish sense of humour and an infectious chuckle, cautious until sure of his facts”. Raventos found in animals that the new hydrocarbon had desirable properties; non-flammability, absent pungency, high potency (close to that of chloroform), no obvious toxicity, and could produce a rapid induction of and recovery from anesthesia [47]. Although halothane had significant cardiovascular effects (it could predispose to irregular beating of the heart and could depress the heart), its dangers were far less than those of the other eleven ‘highly cardiotoxic’ compounds synthesized by Suckling.
The laboratories of ICI are in Widnes, Cheshire, close to the Manchester Royal Infirmary where an anesthetist, Michael Johnstone, worked. Johnstone had witnessed the limitations of ‘rag and bottle’ chloroform anesthesia and this experience determined his career choice, believing that as an anesthetist he could improve the lot of the patient. On January 20, 1956, Suckling received a telephone call from Raventos, who was in the operating theater with Johnstone to witness the first use of halothane in a patient. Ethical approval was not sought, and preclinical investigation had not been undertaken as was standard practice for the time. Raventos related that everything had gone satisfactorily, and in turn, Suckling relayed the message to Ferguson. Unknown at that moment, chance had played yet another role in the successful development of halothane. The first patient scheduled for operation, the one that would have received halothane, had awakened unwell, and her surgery was postponed. The second patient received halothane in her stead. The next morning the first scheduled patient developed jaundice! Had the patient received halothane, surely the halothane would have been blamed, ending halothane’s use forever. To paraphrase Lefty Gomez, an American baseball player, “it is better to be lucky than good”.
Johnstone continued the early trials [48], and by September of 1956, over 500 patients had received halothane. The trials were widened before its release in the UK in 1957, and the US in 1958. In the initial trials, halothane was given by the open drop method, but a calibrated vaporizer, the Fluotec, was soon developed by a small engineering firm, Cyprane, and this vaporizer facilitated the commercial success of halothane. In the US, fortuitously, another vaporizer, the Copper Kettle had already been developed [49]. Both of these vaporizers allowed anesthetists to control the depth of anesthesia, quickly and predictably. Due to the combination of high vapor pressure, lower blood solubility, and high potency, precise control was essential to the safe delivery of this new potent inhaled anesthetic.
The advantages of the new alkane rapidly placed it as the anesthetic of choice world wide. But within four years of its release, cases of unexplained postoperative liver failure emerged. Bunker and Blumenfeld reported that a 16 year old school girl had died in the Sutter Community Hospital in Sacramento, of liver failure, 13 days after being exposed to halothane for a minor surgery [50]. Gerald Brody (pathologist) and Robert Sweet (anesthesiologist) reported four cases of severe hepatic injury after halothane anesthesia [51]. Such observations prompted Bunker to propose that the National Academy of Sciences in Washington organize a study of the safety of halothane, a study that would define the risk imposed on our patients by this extraordinarily useful anesthetic. One thing seemed clear: although halothane might cause severe injury to the liver, the incidence appeared to be less than that seen with chloroform. But how much less? A large epidemiological study would be needed to sort out the incidence and the characteristics, the phenotype, associated with “halothane hepatitis”. A large scale retrospective analysis was undertaken and the results published in 1966 [52], with more detailed results published in 1969 [53]. Only 3 patients out of 367,000 given halothane gave clear evidence of a direct cause and effect relationship. The anesthesia community breathed a sigh of relief.
Mounting evidence indicated that halothane-induced liver damage took two forms [54]. One was mild, transient and sub-clinical, measurable only by changes in liver function tests. The rare second form resulted in fulminant injury to the liver and a high mortality. Between 1978 and 1985, the UK Committee on Safety of Medicines (CSM) received 84 reports of liver injury after halothane with adequate histories in 62 patients. Of the 62, 41 had been exposed to halothane more than once. The mortality rate was 29% in patients given but one anesthetic with halothane; 41% after two exposures; and 56% in those given more than two. Not only did mortality increase with repeated exposures, the time to the appearance of injury shortened. These relationships suggested an immune-mediated, allergic-type reaction, with the following sequence mediating injury [55]. The liver metabolizes halothane to a reactive form of trifluoracetyl (CF3-COO-) which by virtue of its reactivity can combine with liver proteins (liver proteins because they are nearby). The addition of the trifluoracetyl group to the protein changes the immune character of the protein which is no longer recognized as “self” or normal, but as “foreign”. The body’s immune system produces antibodies that attack the “foreign” proteins and, thereby, injure the liver. A greater immune response is mounted with repeated exposures to halothane, as would occur with repeated vaccinations. The precise sequence of events is complicated. Although the incidence of fatal halothane-induced hepatitis was small, it enormously impacted on the use of halothane. Halothane is now available in the UK only to special order. Use of halothane continues in developing countries where costs trump the rare risk of severe injury of the liver.
ICI did not attempt to produce a better inhaled anesthetic to follow up on their success with halothane. However, in 1983 they introduced an alternative to thiopental, propofol (isopropylphenol) for intravenous induction and maintenance of anesthesia. Thus, the early 1980s saw the end of a nearly 150 year era, in which inhaled agents were the invariable foundations of general anesthesia and total intravenous anesthesia became a viable alternative.
The introduction of halothane also marked a new era in anesthetic pharmacology. Twenty years earlier, Booth and Bixby had predicted part of halothane’s beneficial and detrimental effects: fluorine substitution produced an anesthetic that was non-explosive and less toxic than chloroform. The rare association with hepatic failure initiated epidemiological surveys (outcome studies, studies required for our present goal of evidence-based medicine) and extensive studies into the immunological basis of unpredicted side effects.
Methoxyflurane
Although Miller (later at Cornell) and colleagues synthesized methoxyflurane under a Manhattan Project contract in 1944, only in 1960 did Joseph Artusio and Alan Van Poznac, also at Cornell publish their results of studies of methoxyflurane in humans [56]. Methoxyflurane was non-explosive, extremely potent with a MAC of 0.16%, and purportedly a good analgesic. This latter property gave it a place in obstetric analgesia (licensed for use in obstetrics in 1970 in the UK). But problems with methoxyflurane limited its use. It was too soluble in blood to allow a rapid induction and recovery [57]. The liver metabolized more than 50%, perhaps even 75% of the methoxyflurane taken into the body [58], with metabolites excreted in the urine for up to 12 days postoperatively. Prolonged use’3 MAC-hours or longer’could cause high output kidney failure [59]. The French had a nice term for this ‘Diabetes Insipidus Fluorique’. Methoxyflurane never gained widespread acceptance in the US, and its use slowly withered away. Licenses for its use have lapsed in the UK and North America. However, in Australia, paramedical personnel, the military, and emergency departments still use it regularly for analgesia. Self-administered by means of a disposable device allowing a maximum dose of 6 ml over 50 to 55 min, it remains registered for use in Australia, New Zealand and the Middle East. The only manufacturing facility is now in Australia [60].
The next fluorinated anesthetic to be introduced came from the efforts of the chemist Ross Terrell (Fig. 46.2), from a sustained project, underwritten by the Ohio Chemical Corporation, dedicated to the development of a better inhaled anesthetic [61]. But first we need to review the topic of depth of anesthesia and how to measure it. The discovery of the measurement was concurrent with and partially driven by the rise of halothane as the predominant anesthetic of the day.
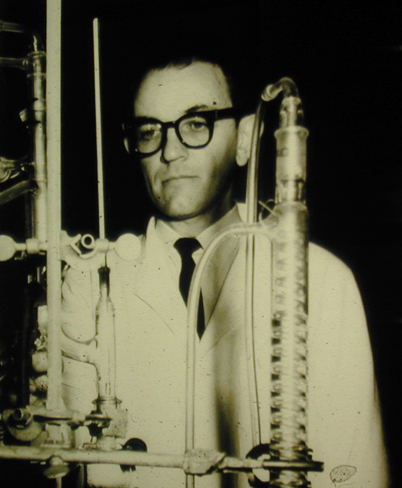
Fig. 46.2
A young Ross Terrell, probably in the 1960s. (Courtesy of Airco files)
Defining Anesthetic Depth: The Minimum Alveolar Concentration or MAC
In 1847, by dint of painstaking observation, John Snow defined depth as a succession of five degrees, the fourth being the degree commonly used to facilitate the progress of surgery. During World War I, Arthur Guedel refined Snow’s concepts, arriving at a scheme of four stages, the third being that used for surgery [62]. The introduction of premedication, the use of opioids and then muscle relaxants provoked a debate concerning what the term ‘anesthesia’ meant’what did it encompass and could depth be scientifically measured? Cedric Prys-Roberts observed that anesthesia is the state in which, as a result of drug induced unconsciousness, the patient neither perceives nor recalls noxious stimuli [63]. The motor response to noxious stimuli is essentially an all or none one with motor activity resulting from stimulation of the inadequately anesthetized patient. Snow observed that his third degree permitted such movement but the fourth degree did not [64].
Eger, Saidman and Brandstater used this motor reflex as an end point in defining the minimum alveolar concentration (MAC) of anesthetic needed to inhibit movement in 50% of subjects [65]. This concentration is greater than that required to produce unconsciousness. The concept of MAC, developed by Eger and his colleagues in San Francisco, was an important contribution to the anesthetist’s ability to conceptualize and thus modify depth of anesthesia and use different inhaled agents safely. It enabled quantitative comparisons of the effects of inhaled anesthetics and the ability to define factors affecting the depth of anesthesia.
A Search for Metabolically Stable Ethers
Like his predecessors searching for a better anesthetic, Ross Terrell synthesized several series of fluorinated compounds including alkanes, alcohols and various ethers. A potentially useful compound would produce a “smooth” anesthetic state, preferably without also producing convulsions. A useful compound would be stable, would resist degradation by the liver or by carbon dioxide absorbents, and would not be toxic. He quickly discarded alkanes because they predisposed to irregular beating of the heart, and focused (because they did not so predispose) on ethers, particularly methyl ethyl ethers. Terrell worked with dogged persistence’remember halothane was Suckling’s 9th compound. In 1963 Terrell synthesized a methyl ethyl ether (CHF2-O-CF2-CHFCl) that had the code name Investigational Compound Number 347 or I-347 because it was the 347[th]structure he synthesized. A first report of its anesthetic characteristics appeared in 1966 [66], and it was given the generic name ‘enflurane’.
Enflurane
Compared with halothane, enflurane had two immediately apparent, indeed predictable advantages, and other disadvantages that became clearer with time. First, it was a fluorinated methyl ethyl ether, and ethers, unlike alkanes, tend not to cause cardiac arrhythmias. Second, only 2–3% of the enflurane taken up was metabolized, and thus it was less likely to cause injury from potentially toxic metabolites. That is, the relatively low metabolism meant that defluorination was small, far smaller than with methoxyflurane, and cases of postoperative renal insufficiency did not appear. So enflurane provided a potentially safer alternative to either halothane or methoxyflurane. Not predicted, was the early finding of an association of enflurane anesthesia with tonic and clonic muscular activity [67]. Indeed, EEG epileptiform activity was common, although frank seizure activity was uncommon.
By the mid 1970s, enflurane supplanted halothane in much of the developed world except that halothane continued to be used for anesthesia in children because of halothane’s absence of pungency. Methoxyflurane and Trilene had hardly any followers and a few stalwarts refused to give up ether. The non-flammable, minimally toxic, potent characteristics of enflurane increasingly made it the leader.
At this juncture two trends increasingly influenced anesthetic practice, trends ensuring a persistent search for alternatives to halothane and enflurane. First, advances in anesthetic and surgical techniques, coupled with economic considerations, increased the demand for and scope of day case (patients being both admitted and discharged the day of surgery) surgery. By the 1980s, surgery was increasingly being performed on a day case basis, and in the US, by the 1990s, this increased to a majority. Second, obesity rates in prosperous nations steadily increased. In 1980, I left the UK to work at the University of Michigan Medical Center in Ann Arbor. I remember being stunned at the high proportion of obese patients. Eventually, the rest of the world caught up with this epidemic of obesity. The increasing use of day case surgery and increasing girth of the population dictated a need for anesthetics that were eliminated rapidly to speed the rate of recovery. Those were not the only goals of the ideal anesthetic. Additionally, it should be non-flammable, lack toxicity (for both patient and operating room personnel), and have minimal cardiorespiratory effects. Also, it should be inexpensive. Both enflurane and halothane fell short of the ideal.
A Search for Less Soluble Anesthetics
Terrell’s team synthesized more than 700 compounds in the 1950s and 60s, in pursuit of a better inhaled anesthetic. They synthesized the 469[th]compound in 1965, two years after having synthesized the structural isomer enflurane. I-469 (CHF2-O-CHCl-CF3) was given the generic name, isoflurane (from the term ‘isomer’).
Isoflurane
Isoflurane continued the trend towards a lower solubility and a greater resistance to metabolism (Table 46.1). In animals, it had a good “anesthetic syndrome” without evidence of the convulsive activity seen with enflurane. It was stable to UV light and alkali, including soda lime. It thus looked promising. However, the manufacturing process required purification by distillation, and the isomers of I-469 have boiling points close together. Thus a large number of distillations were initially needed to obtain the pure compound, and the expense of such distillations nearly led to the abandonment of isoflurane.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







