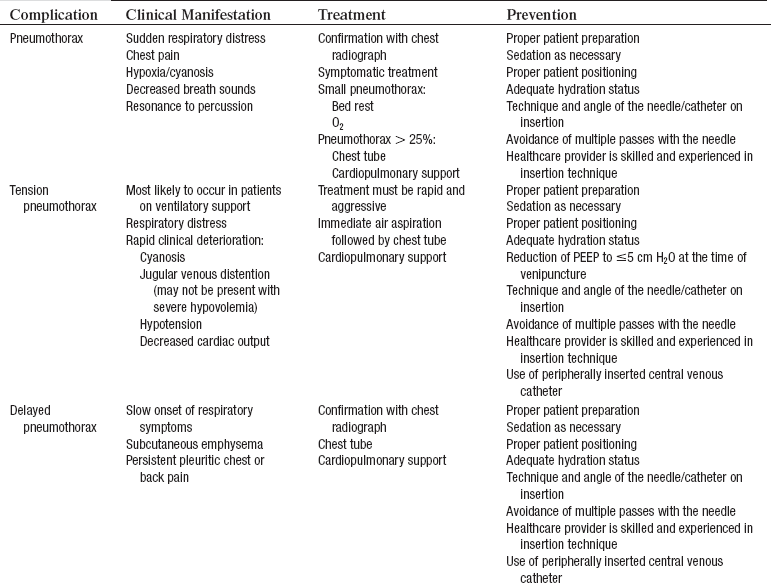
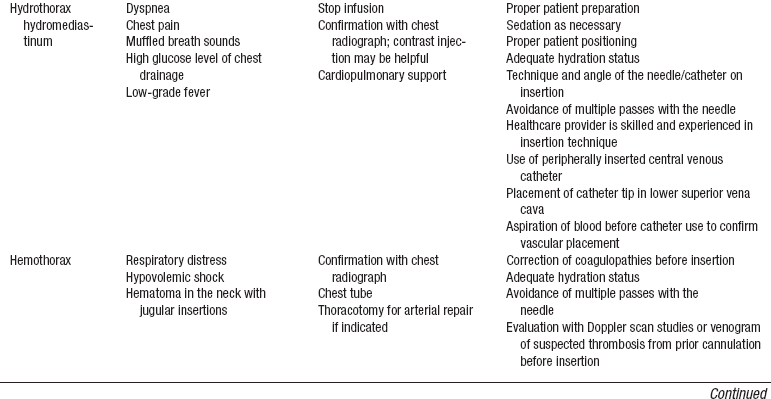
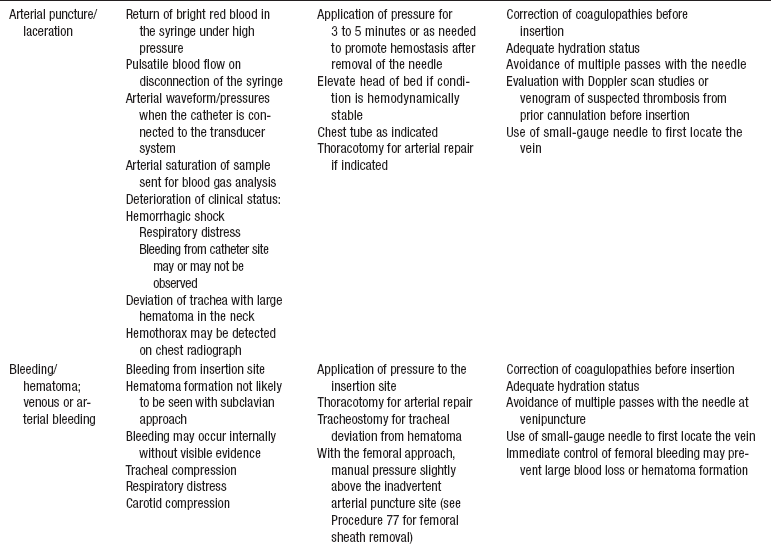
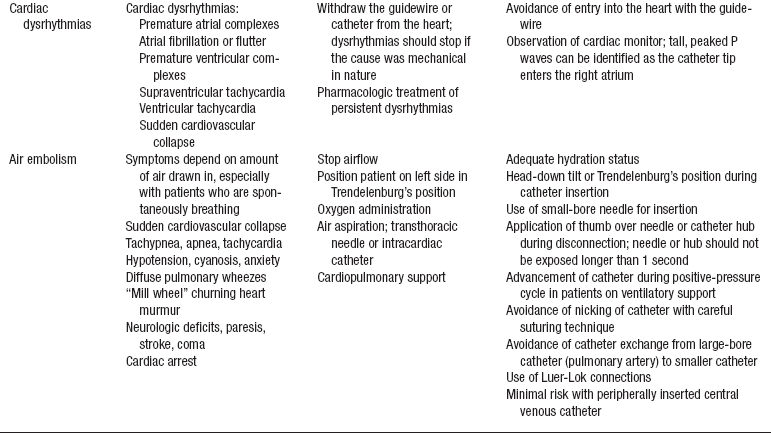
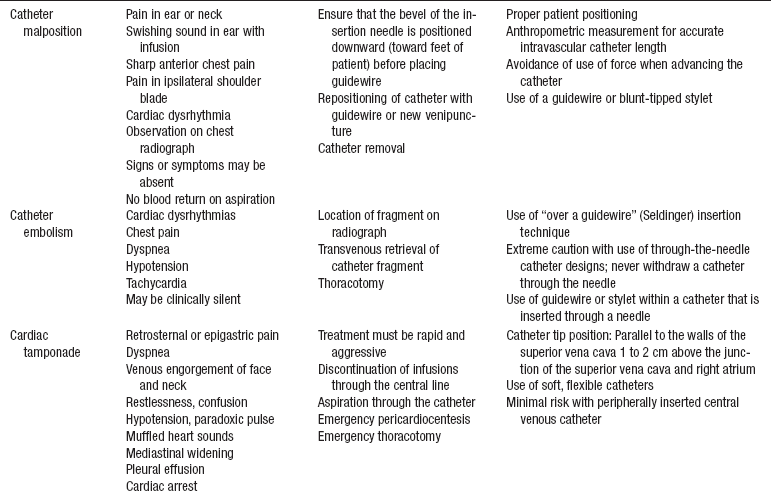
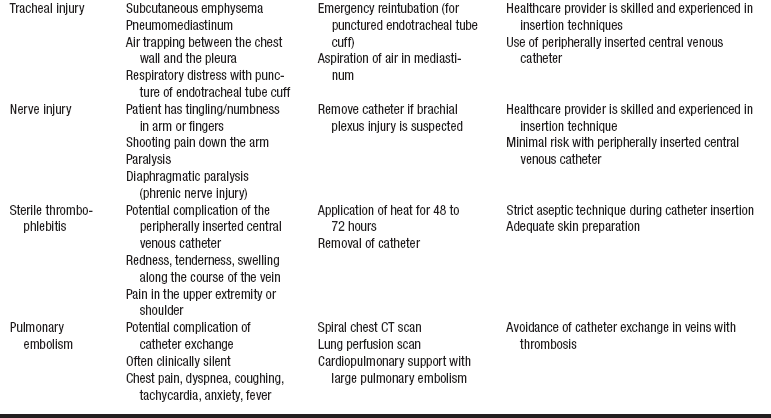
PROCEDURE 81 • Knowledge of the normal anatomy and physiology of the cardiovascular system is needed. • Clinical and technical competence in central line insertion and suturing is important. • Knowledge of the principles of sterile technique is essential. • Knowledge of the anatomy and physiology of the vasculature and adjacent structures of the neck, groin, and arm is needed. • Competence in chest radiographic interpretation is necessary. • Advanced cardiac life support knowledge and skills are needed. • Indications for a central venous catheter (CVC) include the following4,7: • Placement of a CVC can guide treatment after major surgery and during active bleeding. • The central venous pressure (CVP) can be helpful in the differentiation of right ventricular failure from left ventricular failure. • The CVP is commonly elevated during or after right ventricular failure, ischemia, or infarction because of decreased compliance of the right ventricle while the pulmonary artery occlusion pressure is normal. • The CVP can be helpful in the determination of hypovolemia. The CVP value is low if the patient is hypovolemic. Venodilation also decreases CVP. • Relative contraindications of CVC insertion include the following4,7: • The CVP provides information regarding right heart filling pressures and right ventricular function and volume. • The CVP historically was measured with a water manometer system but is now measured with a single-pressure transducer system (see Procedures 70 and 76). • The CVP waveform is identical to the right atrial pressure (RAP) waveform. • The normal CVP value is 2 to 6 mm Hg. • Electrocardiographic (ECG) monitoring is essential in the accurate interpretation of the CVP value. • Understanding is needed of a, c, and v waves. The a wave reflects right atrial contraction; the c wave reflects closure of the tricuspid valve; and the v wave reflects right atrial filling during ventricular systole (see Figs. 70-1 and 73-7). • Dysrhythmias may alter CVP or RAP waveforms. • The risk for a pneumothorax is minimized with use of an internal jugular vein. The preferred site for catheter insertion is the right internal jugular vein. The right internal jugular vein is a “straight shot” to the right atrium. • The right or left subclavian veins are also sites for central catheter placement. Placement of a CVC through the right subclavian vein is a shorter and more direct route than the left subclavian vein because it does not cross the midline of the thorax.4,7 • Femoral veins may be accessed but have the disadvantages of limiting the patient to bed rest with immobilization of the leg and increasing the patient’s risk of infection. • The presence of a pacemaker may alter the choice of placement of a CVC because of a risk for dislodging pacemaker leads with insertion of a CVC. • Complications may occur during or after insertion of a central venous catheter (see Table 81-1).
![]() Central Venous Catheter Insertion (Perform)
Central Venous Catheter Insertion (Perform)
PREREQUISITE NURSING KNOWLEDGE
 Hypotension after major surgery
Hypotension after major surgery
 Right ventricular ischemia or infarction
Right ventricular ischemia or infarction
 Administration of total parenteral nutrition
Administration of total parenteral nutrition
 Lack of peripheral venous access
Lack of peripheral venous access
 Assessment of hypovolemia or hypervolemia
Assessment of hypovolemia or hypervolemia
 Long-term infusions of medications
Long-term infusions of medications
 Placement of pulmonary artery catheters
Placement of pulmonary artery catheters
 Presence of a permanent pacemaker
Presence of a permanent pacemaker
 Obstruction of the superior or inferior vena cava, innominate vein, subclavian veins, or internal jugular veins
Obstruction of the superior or inferior vena cava, innominate vein, subclavian veins, or internal jugular veins
81: Central Venous Catheter Insertion (Perform)