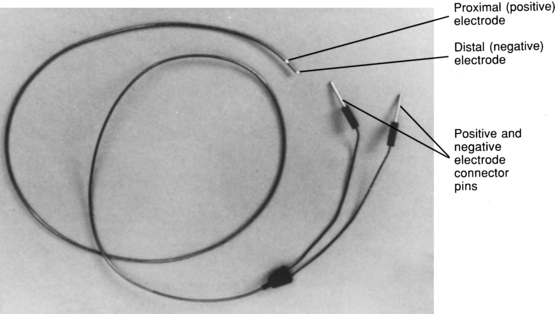
PROCEDURE 53 • Knowledge of the normal anatomy and physiology of the cardiovascular system, principles of cardiac conduction, and basic and advanced dysrhythmia interpretation is needed. • Knowledge of temporary pacemaker function and expected patient responses to pacemaker therapy is necessary. • Clinical and technical competence in central line insertion, temporary transvenous pacemaker insertion, and suturing is needed. • Clinical and technical competence related to use of temporary pacemakers is necessary. • Competence in chest radiograph interpretation is needed. • Advanced cardiac life support knowledge and skills are needed. • Principles of general electrical safety apply with use of temporary invasive pacing methods. Gloves always should be worn when handling electrodes to prevent microshock. • The insertion of a temporary transvenous pacemaker is performed in emergency and elective clinical situations. Temporary transvenous pacing may be used to: • Temporary transvenous pacing is indicated for the following: • When temporary transvenous pacing is used, the pulse generator is attached externally to a pacing lead wire that is inserted through a vein into the right atrium or right ventricle. • Veins used for the insertion of a transvenous pacing lead wire are the subclavian, femoral, brachial, internal jugular, or external jugular. • Single-chamber ventricular pacing is the most appropriate method in an emergency because the goal is to establish a heart rate as quickly as possible. • The transvenous pacing lead is an insulated wire with one or two electrodes at the tip of the wire (Fig. 53-1). • The pacing lead can be a hard-tipped or a balloon-tipped pacing catheter that is placed in direct contact with the endocardium. Most temporary leads are bipolar with the distal tip electrode (seen as a metal ring) separated from the proximal electrode by 1 to 2 cm of pacing catheter (also seen as a metal ring; see Fig. 53-1). • Basic principles of cardiac pacing include sensing, pacing, and capture. • Sensing refers to the ability of the pacemaker device to detect intrinsic myocardial electrical activity. Sensing occurs if the pulse generator is in the synchronous or demand mode. The pacemaker either is inhibited from delivering a stimulus or initiates an electrical impulse. • Pacing occurs when the temporary pulse generator is activated and the programmed level of energy travels from the pulse generator through the temporary pacing lead wire to the endocardium, which is known as pacemaker firing and is represented as a vertical line or spike on the electrocardiogram (ECG) recording.
![]() Temporary Transvenous Pacemaker Insertion (Perform)
Temporary Transvenous Pacemaker Insertion (Perform)
PREREQUISITE NURSING KNOWLEDGE
 Stimulate the myocardium to contract in the absence of an intrinsic rhythm
Stimulate the myocardium to contract in the absence of an intrinsic rhythm
 Establish adequate cardiac output and blood pressure
Establish adequate cardiac output and blood pressure
 Ensure tissue perfusion to vital organs
Ensure tissue perfusion to vital organs
 Reduce the possibility of ventricular dysrhythmias in the presence of bradycardia
Reduce the possibility of ventricular dysrhythmias in the presence of bradycardia
 Supplement an inadequate rhythm, such as when transient decreases in heart rate occur (e.g., chronotropic incompetence in shock)
Supplement an inadequate rhythm, such as when transient decreases in heart rate occur (e.g., chronotropic incompetence in shock)
 Allow the administration of medications that may cause a rhythm or conduction abnormality (e.g., beta blockers) in the symptomatic bradycardia, complete heart block, new bundle-branch block with transient complete heart block, alternating bundle-branch block)
Allow the administration of medications that may cause a rhythm or conduction abnormality (e.g., beta blockers) in the symptomatic bradycardia, complete heart block, new bundle-branch block with transient complete heart block, alternating bundle-branch block)
 Third-degree atrioventricular (AV) block
Third-degree atrioventricular (AV) block
 Dysrhythmias that are complicating acute myocardial infarction (e.g., symptomatic bradycardia, complete heart block, new bundle-branch block with transient complete heart block, alternating bundle-branch block)
Dysrhythmias that are complicating acute myocardial infarction (e.g., symptomatic bradycardia, complete heart block, new bundle-branch block with transient complete heart block, alternating bundle-branch block)
 Sinus node dysfunction (e.g., symptomatic bradydysrhythmias, treatment of bradycardia-tachycardia syndromes, sick sinus syndrome)
Sinus node dysfunction (e.g., symptomatic bradydysrhythmias, treatment of bradycardia-tachycardia syndromes, sick sinus syndrome)
 Ventricular standstill or cardiac arrest
Ventricular standstill or cardiac arrest
 Long QT syndrome with ventricular dysrhythmias
Long QT syndrome with ventricular dysrhythmias
 Prophylaxis with cardiac diagnostic or interventional procedures
Prophylaxis with cardiac diagnostic or interventional procedures
 Chronotropic incompetence in the setting of cardiogenic shock
Chronotropic incompetence in the setting of cardiogenic shock
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


53: Temporary Transvenous Pacemaker Insertion (Perform)