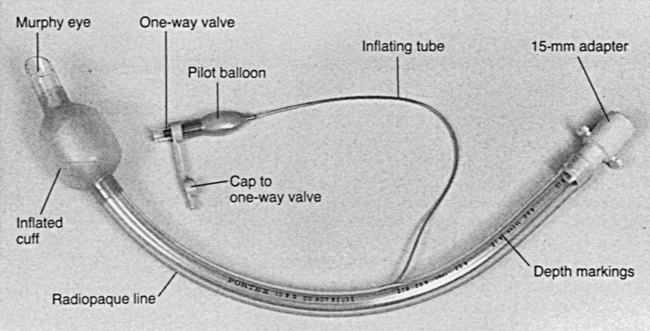
PROCEDURE 2 • Anatomy and physiology of the pulmonary system should be understood. • Indications for endotracheal intubation include the following5,12: • Pulse oximetry should be used during intubation so that oxygen desaturation can be detected quickly. • Preoxygenation with 100% oxygen and a self-inflating manual resuscitation bag-valve-mask device with a tight-fitting face mask should be performed for 3 to 5 minutes before intubation. • Intubation attempts should take no longer than 15 to 20 seconds. If more than one intubation is necessary, ventilation with 100% oxygen and a self-inflating manual resuscitation bag-valve-mask device with a tight-fitting face mask should be performed for 3 to 5 minutes before each attempt. If intubation is not successful after three attempts, consider use of other airway options, such as the Combitube or King Airway. • Application of cricoid pressure (Sellick maneuver) may increase the success of the intubation. This procedure is accomplished with applying firm downward pressure on the cricoid ring, pushing the vocal cords downward so that they are visualized more easily. Once begun, cricoid pressure must be maintained until intubation is completed (Fig. 2-1). • Two types of laryngoscope blades exist: straight and curved. The straight (Miller) blade is designed so that the tip extends below the epiglottis, to lift and expose the glottic opening. The straight blade is recommended for use in obese patients, pediatric patients, and patients with short necks because their tracheas may be located more anteriorly. When a curved (Macintosh) blade is used, the tip is advanced into the vallecula (the space between the epiglottis and the base of the tongue), to expose the glottic opening. • Laryngoscope blades are available with fiberoptic light delivery systems. These systems provide a brighter light than bulbs, which can become scratched or covered with secretions. • Endotracheal tube size reflects the size of the internal diameter of the tube. Tubes range in size from 2.5 mm for neonates to 9 mm for large adults. Endotracheal tubes that range in size from 7 to 7.5 mm are used for average-sized adult women, whereas endotracheal tubes that range in size from 8 to 9 mm are used for average-sized adult men (Fig. 2-2).8,9,12 The tube with the largest clinically acceptable internal diameter should be used to minimize airway resistance and assist in suctioning.4 • Endotracheal intubation can be done via nasal or oral routes. The skill of the practitioner who performs the intubation and the patient’s clinical condition determine the route used. • Nasal intubation is relatively contraindicated in trauma patients with facial fractures or suspected fractures at the base of the skull and after cranial surgeries, such as transnasal hypophysectomy. • Improper intubation technique may result in trauma to the teeth, soft tissues of the mouth or nose, vocal cords, and posterior pharynx. • In patients with suspected spinal cord injuries, in-line cervical immobilization of the head must be maintained during endotracheal intubation. • Primary and secondary confirmation of endotracheal intubation should be performed.1,4 • End-tidal CO2 (PetCO2) monitoring devices have been shown to be reliable indicators of expired CO2 in patients with perfusing rhythms.1,5,11,13,15 During cardiac arrest (nonperfusing rhythms), low pulmonary blood flow may cause insufficient expired CO2.14 CO2 detected with an end-tidal CO2 detector is a reliable indicator of proper tube placement.6 If CO2 is not detected, use of an esophageal detector device is recommended.1,3,11,15 • Disposable end-tidal CO2 detectors are chemically treated with a nontoxic indicator that changes color in the presence of CO2 and indicates that the endotracheal tube has been placed successfully into the trachea. • Continuous end-tidal CO2 monitors may be used to confirm proper endotracheal tube placement after intubation attempts and allow for the detection of future tube dislodgment. • Esophageal detector devices work by creating suction at the end of the endotracheal tube with compressing a flexible bulb or pulling back on a syringe plunger. When the tube is placed correctly in the trachea, air allows for reexpansion of the bulb or movement of the syringe plunger. If the tube is located in the esophagus, no movement of the syringe plunger or reexpansion of the bulb is seen. These devices may be misleading in patients who are morbidly obese, patients in status asthmaticus, patients late in pregnancy, or patients with large amounts of tracheal secretions.1 • Double-lumen endotracheal tubes are used for independent lung ventilation in situations with bleeding of one lung or a large air leak that would impair ventilation of the good lung. • The endotracheal tube also provides a route for the administration of emergency medications (e.g., lidocaine, epinephrine, atropine, and naloxone) when no other routes of administration are available.4 • Personal protective equipment, including eye protection • Endotracheal tube with intact cuff and 15-mm connector (women, 7-mm to 7.5-mm tube; men, 8-mm to 9-mm tube) • Laryngoscope handle with fresh batteries • Laryngoscope blades (straight and curved) • Spare bulb for laryngoscope blades
![]() Endotracheal Intubation (Perform)
Endotracheal Intubation (Perform)
PREREQUISITE NURSING KNOWLEDGE
 Altered mental status (head injury, drug overdose)
Altered mental status (head injury, drug overdose)
 Anticipated airway obstruction (facial burns, epiglottitis, major facial or oral trauma)
Anticipated airway obstruction (facial burns, epiglottitis, major facial or oral trauma)
 Upper airway obstruction (e.g., from swelling, trauma, tumor, bleeding)
Upper airway obstruction (e.g., from swelling, trauma, tumor, bleeding)
 Ineffective clearance of secretions (i.e., inability to maintain or protect airway adequately)
Ineffective clearance of secretions (i.e., inability to maintain or protect airway adequately)
 Primary confirmation of proper endotracheal tube placement includes visualization of the tube passing through the vocal cords, absence of gurgling over the epigastric area, auscultation of bilateral breath sounds, bilateral chest rise and fall during ventilation, and mist in the tube.
Primary confirmation of proper endotracheal tube placement includes visualization of the tube passing through the vocal cords, absence of gurgling over the epigastric area, auscultation of bilateral breath sounds, bilateral chest rise and fall during ventilation, and mist in the tube.
 Secondary confirmation of proper endotracheal tube placement is necessary to protect against unrecognized esophageal intubation. Methods include use of disposable end-tidal carbon dioxide (CO2) detectors, continuous end-tidal CO2 monitors, and esophageal detection devices.
Secondary confirmation of proper endotracheal tube placement is necessary to protect against unrecognized esophageal intubation. Methods include use of disposable end-tidal carbon dioxide (CO2) detectors, continuous end-tidal CO2 monitors, and esophageal detection devices.
EQUIPMENT
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


2: Endotracheal Intubation (Perform)