Weaning and Discontinuation of Mechanical Ventilation
KEY POINTS
1 A continuing need for ventilator assistance may arise from oxygen desaturation of hemoglobin during spontaneous breathing, cardiovascular instability during machine withdrawal, psychological dependence, or most commonly, imbalance between ventilatory capability and demand.
2 The minute ventilation requirement bears a quadratic relationship to the work of breathing. Three primary factors determine the minute ventilation requirement: the CO2 production, the efficiency of ventilation, and the central drive to breathe.
3 Ventilatory power is the product of minute ventilation and the mechanical work of breathing per liter of ventilation. For any specific tidal volume and flow rate, the primary determinants of the inspiratory work per liter of ventilation are the resistance and elastance of the respiratory system and auto-positive end-expiratory pressure, a reflection of dynamic hyperinflation.
4 Ventilatory capability is determined by the central drive to breathe and the bulk, strength, and endurance of the ventilatory muscles. The induction of fatigue by excessive effort impairs muscular performance for at least 12 to 24 h afterward. Sleep is essential for optimal neuromuscular performance and for preparing the patient for the weaning attempt.
5 Prediction of success or failure of a weaning trial involves the assessment of oxygen exchange, cardiovascular status, and muscular endurance. Although individual measures of strength, gas exchange, or workload aid in this assessment, “integrative” weaning indices observed during a brief trial of unaided breathing (e.g., rapid shallow breathing index, interpreted in conjunction with the minute ventilation and chest compliance) as well as “integrative” tests of ventilatory reserve (breathing pattern variability, cough-induced inspiratory capacity) are perhaps the most physiologically sound indicators. Expiratory performance is especially important to evaluate when there is a high secretion load.
6 Persistent failure to wean despite adequate respiratory parameters should prompt consideration of cardiac ischemia, congestive heart failure, psychological dependence or delirium, gas exchange deterioration, lingering effects of sedation, or other nonrespiratory explanation for the failure. A common culprit is net fluid balance that is markedly positive.
7 After the patient has had optimal preparation, the weaning sequence involves estimation of the likelihood of success, a trial of spontaneous ventilation, gradual withdrawal of ventilatory assistance (when indicated), a brief period of observation with minimal pressure support, extubation, and close follow-up after ventilator discontinuance and extubation.
8 Patients experiencing protracted difficulty during removal of ventilatory support should receive adequate ventilator assistance at night to permit sleep. The patient must never be forced to work beyond his or her ability to comfortably sustain it.
9 Reintubation occasionally is necessary in the first few days after extubation. These delayed weaning failures usually arise because of an inability to swallow normally (resulting in oropharyngeal aspiration), glottic swelling, inability to clear thick airway secretions, or congestive heart failure. Appropriate precautions during this period may avert failure. Noninvasive ventilation may provide a useful bridge across this difficult period.
10 Weaning from tracheostomy should be considered when the patient no longer requires frequent airway suctioning, high inspired fractions of O2, or periodic
(nocturnal) connection to the ventilator. Conversion to noninvasive ventilation and/or assisted coughing is possible for many patients previously assigned to permanent tracheostomy.
(nocturnal) connection to the ventilator. Conversion to noninvasive ventilation and/or assisted coughing is possible for many patients previously assigned to permanent tracheostomy.
Once the underlying reason for initiating ventilator support has been successfully addressed, many patients tolerate abrupt termination of mechanical assistance without needing to gradually adjust to spontaneous breathing. However, evaluating readiness is always a clinical judgment, and in that minority of patients for whom withdrawing machine support proves difficult, a strategy for transferring the respiratory workload to the patient must be developed (Table 10-1). Weaning is the graded removal of ventilator support from patients who cannot tolerate immediate conversion to fully spontaneous breathing. The weaning process often takes place in several stages: weaning from positivepressure ventilation, weaning from positive endexpiratory pressure (PEEP), weaning from the endotracheal (ET) or tracheostomy tube, and weaning from supplemental oxygen.
PHYSIOLOGIC DETERMINANTS OF VENTILATOR DEPENDENCE
A continuing need for breathing assistance may arise from O2 desaturation of hemoglobin during unaided breathing, cardiovascular instability during machine withdrawal, psychological dependence, or from imbalance between ventilatory capability and demand. Often, several of these causes operate simultaneously.
TABLE 10-1 WHO BENEFITS FROM GRADUAL WITHDRAWAL OF MACHINE SUPPORT? | |
|---|---|
|
Psychological Factors
Prolonged mechanical ventilation is a harrowing experience that may elicit anxiety, depression, or psychosis. Delirium, manifested by inattentiveness, paranoid behavior, and disorientation, occurs very commonly in sleep-deprived and elderly patients receiving medications that interfere with normal mental functioning (e.g., corticosteroids, benzodiazepines). A careful evaluation of mental status often is fruitful, because cooperation and avoidance of panic reactions during the weaning attempt may depend on control of the delirium. Ensuring sleep and the use of appropriate psychotropic agents (e.g., haloperidol or quetiapine) can speed up the process (see Chapter 17).
Arterial Hypoxemia
Mechanical ventilation can improve arterial oxygenation by providing large tidal breaths that oppose atelectasis, sealing the airway to allow delivery of high inspired concentrations of oxygen and PEEP, reducing or offsetting the effects of pulmonary edema, improving the output requirements and loading conditions of a compromised heart, and improving the balance between tissue oxygen delivery and demand. Under a high breathing workload, the respiratory muscles consume a great deal of oxygen. Vigorous expiratory activity reduces end-expiratory lung volume. Stressful breathing may also increase the oxygen demand of other organs by causing agitation or discharge of catecholamines. When cardiac output is compromised, this increased oxygen demand may force greater O2 extraction. The admixture of the desaturated mixed venous blood that results may then contribute to hypoxemia. Moreover, increased metabolic demands may cause myocardial decompensation, ischemia, or diastolic dysfunction. Mechanical ventilation mitigates these problems by relieving much of the ventilatory workload.
Cardiovascular Instability
Resuming a high ventilatory workload often presents a cardiovascular challenge in the setting of ischemic disease, heart failure, or reduced cardiac reserve. Inappropriately low cardiac output can contribute directly to hypoxemia and weakness of the ventilatory pump. Cardiovascular instability overtly limits the pace of ventilator withdrawal when chest pain, diastolic dysfunction, or arrhythmias develop during the reloading of the respiratory pump. Hypoxemia, abruptly altered cardiac loading conditions, and stress-related release of
catecholamines frequently provoke rhythm disturbances in the transition to spontaneous breathing. Resuming spontaneous breathing simultaneously increases both preload and afterload of the left heart, as well as increases anxiety and the respiratory workload. Oxygen consumption (VO2) and cardiac output can easily double at a time when the heart is least able to provide it. The stress of breathing may trigger coronary ischemia. Careful consideration must be given to optimal preparation of these patients before the weaning attempt.
catecholamines frequently provoke rhythm disturbances in the transition to spontaneous breathing. Resuming spontaneous breathing simultaneously increases both preload and afterload of the left heart, as well as increases anxiety and the respiratory workload. Oxygen consumption (VO2) and cardiac output can easily double at a time when the heart is least able to provide it. The stress of breathing may trigger coronary ischemia. Careful consideration must be given to optimal preparation of these patients before the weaning attempt.
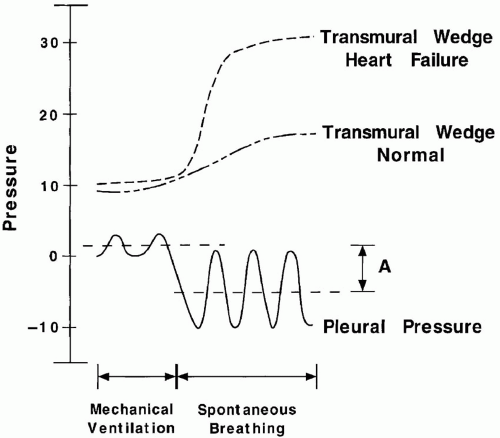
Oxygen administration, establishing electrolyte and pH balance, antiarrhythmic therapy, afterload reduction, anti-ischemic measures, diuresis, and more gradual conversion to fully spontaneous breathing may be instrumental to the success of machine withdrawal. For patients with coexisting airflow obstruction, assuming a high ventilatory workload can be associated with a fall (rather than a rise) in mean intrapleural pressure. As forceful inspiratory efforts lower intrathoracic pressure, central vascular congestion and effective left ventricular afterload increase (Fig. 10-1). In such circumstances, it is essential to reduce total ventilatory demands by measures that improve lung mechanics and reduce minute ventilation. The use of continuous positive airway pressure (CPAP) or noninvasive ventilatory support may be strikingly effective. Prior pharmacotherapy to improve cardiac performance and/or relieve ischemia before weaning is often helpful.
Imbalance of Ventilatory Capability and Demand
To sustain spontaneous ventilation, both ventilatory drive and endurance must be adequate. Impaired ventilatory drive often contributes to CO2 retention or hypoxemia, especially when excessive sedation or chronic hypercapnia is present. The most common reason for ventilator dependence, however, is the inability to maintain appropriate ventilation without intolerable dyspnea. Ventilatory workload is determined by the product of minute ventilation requirement ([V with dot above]E) and the energy expended per liter of gas flow.
Ventilatory Demand: Minute Ventilation Requirement
Reducing the minute ventilation requirement is an important goal because [V with dot above]E bears a quadratic (rather than linear) relationship to the work of breathing. Three primary factors determine the [V with dot above]E requirement: the CO2 production, the efficiency of ventilation, and the sensitivity of the central drive mechanism (Table 10-2).
CO2 Production
Fever, shivering, pain, agitation, increased work of breathing, sepsis, and overfeeding are common causes of increased CO2 production in the intensive care unit (ICU). In the weaning phase, cautious anxiolysis and pain relief can dramatically reduce the ventilatory requirement. Carbon dioxide production is also influenced by underlying nutritional status, as well as by the number and composition of the calories administered. The semistarvation that often precedes critical illness suppresses CO2 production. Despite the importance
of adequate nutrition, patients should not be overfed. Excess calories may be converted to fat, generating CO2 as a metabolic by-product unlinked to energy production. Carbohydrate evolves more CO2 per calorie than fat or protein. However, even though large calorie loads can contribute to ventilatory failure, the importance of calorie composition to ventilator dependence remains to be shown convincingly. Overfeeding also may lead to abdominal distention and discomfort that may adversely impact a patient poised at the boundary of ventilatory failure.
of adequate nutrition, patients should not be overfed. Excess calories may be converted to fat, generating CO2 as a metabolic by-product unlinked to energy production. Carbohydrate evolves more CO2 per calorie than fat or protein. However, even though large calorie loads can contribute to ventilatory failure, the importance of calorie composition to ventilator dependence remains to be shown convincingly. Overfeeding also may lead to abdominal distention and discomfort that may adversely impact a patient poised at the boundary of ventilatory failure.
TABLE 10-2 FACTORS AFFECTING VENTILATORY DEMAND | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Ventilatory Efficiency
Alveolar ventilation (VA), the component of ventilation that is effective in eliminating carbon dioxide, is the total minute ventilation adjusted for the fraction of wasted ventilation. Breathing efficiency can be characterized by the following expression:
where VD/VT is the physiologic dead space fraction (see Chapter 5). Virtually, all the diverse processes that damage the lung or airways of the critically ill patient increase the wasted fraction of ventilation. Certain reversible factors unrelated to underlying lung pathology also can prove to be important. For example, thromboembolic or vasculitic pulmonary arterial occlusion, excessive PEEP, and hypovolemia may reduce perfusion to the ventilated lung, expanding the alveolar dead space. Small tidal volumes are characterized by a high anatomic dead space percentage. By adding “apparatus dead space,” disposable heat and moisture exchangers and other devices or tubing interposed between the ET tube and the “Y” of the ventilator circuit may contribute marginally to ventilatory inefficiency.
Central Drive
Although it is unusual for a patient to remain persistently ventilator dependent solely because of a lack of breathing effort, inappropriately depressed or enhanced drive to breathe may limit weaning progress. As a rule, old and debilitated patients are the most susceptible to drive suppression. Suppressed ventilatory drive may be explained by neurologic impairment, hypothyroidism, lingering sedation (very commonly the predominant cause), sleep deprivation, poor nutrition, and metabolic alkalosis (primary or compensatory). Starvation impairs hypoxic and, to a lesser extent, hypercapnic sensitivity. Interestingly, drive is restored rapidly within a few days of reinitiating adequate feeding, perhaps in advance of improved muscle function. The drive to breathe is generally higher, and the breathing pattern is different in the waking state. Minute ventilation occasionally falls markedly during sleep or sedation and accelerates with the return to alertness. (This pattern often applies to the recovering drug overdose victim.) When infused benzodiazepines are given continuously for days to weeks, sufficient drug and drug metabolites may store in brain and fat tissues to suppress consciousness and/or drive for long periods after they are discontinued (occasionally as long as 7 to 10 days). Such unintended effects argue forcefully for the practice of once daily interruption of sedation to assess the need for and rate of their ongoing use. The administration of pharmacologic stimulants such as doxapram or progesterone has been advocated when depressed drive impedes weaning. These drugs, however, usually are not helpful.
Enhanced central drive arising from neurogenic, psychogenic, reflex, or metabolic stimuli augments ventilatory demand and workload. In asthma and acute pulmonary edema, drive-stimulating reflexes arising from the lung or chest wall downregulate after correction of the underlying disorders. Hypoxemia, hypotension, developing sepsis, and acidosis also accentuate ventilatory demands. Correction of metabolic acidosis is one of the most important ways to reduce central drive. It is also important not to force PaCO2 below the patient’s usual resting value, as the ensuing bicarbonate diuresis redefines the [V with dot above]E needed to maintain (cerebral pH) homeostasis. In fact, PaCO2 somewhat higher than normal for that patient may help minimize the [V with dot above]E requirement. Anxiety and disorientation influence ventilatory demand and often can be addressed successfully by counseling, co-opting the patient into the weaning plan, and cautious use of anxiolytics or major tranquilizers. Haloperidol (Haldol) is a good first option but often proves inadequate. Quetiapine (Seroquel), risperidone, olanzepine (Zyprexa), and occasionally Depakote may work for delirious or combative patients when more usual approaches fail. The ECG must be monitored, however, to avert the possibility of dangerous QT prolongation and arrhythmia induction. Dexmedetomidine (Precedex) is an infused sedative that does not markedly suppress consciousness or drive to breathe. Given the difficulty of removing the dissociative sedatives (e.g., lorazepam, midazolam) without precipitating delirium, such properties often prove useful in weaning applications. Supplementing the inspired O2 fraction is often an effective way to reduce drive and interrupt a panic reaction accompanied by worsening hypoxemia.
Ventilatory Demand: Work per Liter of Ventilation
Intrinsic Factors
Ventilatory power is the product of [V with dot above]E and mechanical work of breathing per liter of ventilation. The quotient of this mechanical workload and neuromuscular efficiency defines how much energy must be expended in breathing. Once tidal volume and inspiratory time are set, the frictional and elastic properties of the respiratory system determine the pressure generated per breath, as well as the external work output per liter of ventilation. The average inspiratory pressure developed by the respiratory system per breath can be approximated by a simple formula:
P = R (VT /ti) + VT/2CRS) + auto-PEEP
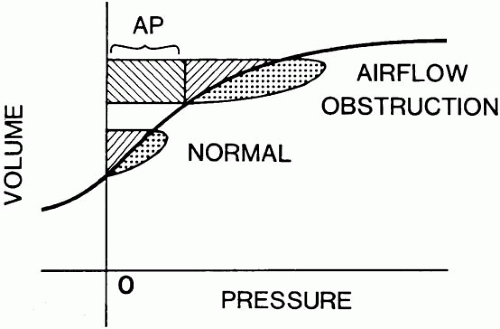
where R and CRS are the inspiratory resistance and compliance of the respiratory system, VT is tidal volume, and ti is the time required for inspiration (see Chapter 5 and Fig. 10-2). Therefore, for the same level of [V with dot above]E, more external work must be done if CRS falls or if VT, auto-PEEP, mean inspiratory flow (VT/ti), or R increase. Bronchospasm, retained secretions, and mucosal edema are the primary reversible factors that increase R. Retained secretions greatly amplify the inspiratory workload in patients with already narrowed airways. Lung edema and infiltration, high lung volumes, pleural effusions, abdominal distention, and supine posture reduce CRS. Air trapping and auto-PEEP are highly dynamic phenomena influenced powerfully by minute ventilation and the ease with which gas empties from the lungs (see Chapter 25). Auto-PEEP varies with changes in the breathing impedance (e.g., bronchospasm, secretion retention, minute ventilation, body position, alteration of inspiratory time fraction, and expiratory muscle activity).
These are not the only factors that determine the energy needed by the respiratory muscles, however. For the same tidal volume, the respiratory muscles consume more oxygen (become less effective) when they begin contraction from a mechanically disadvantageous high lung volume or when the pattern of muscle contraction is poorly coordinated. For example, patients with diaphragmatic weakness may allow the abdominal contents to be drawn upward with each inspiratory effort, so that much of the tension developed by the inspiratory muscles of the chest cage fails to translate into the negative pleural pressure that draws air into the lungs.
Extrinsic Factors
The external properties of the ventilator circuit also can play an important role in determining the ventilatory workload. ET tube resistance exceeds the normal resistance of the upper airway. Frictional pressure losses increase rapidly when high flows are driven through small-caliber tubes. Kinks and encrusted secretions may encroach on an otherwise adequate lumen. In some instances, it may be wise to exchange an orotracheal tube for a larger one (e.g., via a tube changer; see Chapter 6) or replace a nasotracheal tube with an orotracheal one. Tracheostomy is worth considering to reduce resistance and to facilitate extraction of airway secretions in particularly difficult patients. In theory, all pressure-support ventilation (PSV) and CPAP should be withdrawn before extubation to test the marginal patient’s ventilatory reserve (the “T-piece trial,” see following). Even in marginal candidates however, extubation from modest pressure support and CPAP often succeeds, especially when the patient bites the tube or experiences extreme discomfort or a narrow bore tube hinders airflow.
Tracheostomy offers larger tube diameter, shorter axial length, lower resistance and improved secretion clearance. The resistance of other circuit components varies widely and can add significantly to the ventilatory burden. Although the valves of older machines frequently presented problems, they are rarely limiting when using modern equipment.
Ventilatory Capability
The ability to sustain the effort of breathing is determined by respiratory drive, muscle strength and endurance.
Central Drive
Although it is unusual for a patient to remain persistently ventilator dependent solely because of a lack of breathing effort, multiple interacting factors can suppress the output of the ventilatory drive center. As a rule, old and debilitated patients are the most susceptible to drive suppression. Sedatives and neurologic impairment generally receive adequate clinical attention. However, other important causes of drive suppression may be potentially reversible. For example, chronic loading of ventilation (as during a severe bout of asthma) can condition the ventilatory center to tolerate hypercapnea. Metabolic alkalosis, hypothyroidism, and sleep deprivation are commonly overlooked causes of impaired ventilatory drive. Because the output of the ventilatory center tends to parallel metabolic rate and caloric intake, nutritional status is important. Starvation impairs hypoxic and, to a lesser extent, hypercapnic sensitivity. Interestingly, drive is restored rapidly within a few days of reinitiating adequate feeding. The drive to breathe is generally higher, and the breathing pattern is different in the waking state. Minute ventilation occasionally falls markedly during sleep or sedation and accelerates impressively with the return to alertness. (A florid example of this pattern is often provided by the recovering drug overdose victim.) The administration of pharmacologic drive stimulants such as doxapram or progesterone has been advocated when depressed drive impedes weaning. These drugs, however, are seldom helpful or used.
Muscular Performance
Strength
Carbon dioxide retention is uncommon if the patient can generate more than 25% of the predicted maximum inspiratory pressure against an occluded airway. The strength of the respiratory muscles is determined by muscle bulk, the intrinsic properties and loading conditions of the contractile fibers, and the chemical environment in which the muscle contracts. Poor nutrition causes muscle wasting and thereby limits maximal respiratory pressures. As overall body weight diminishes, the mass and strength of the diaphragm decrease proportionately. Paralysis that is sustained for more than 24 to 48 h can initiate the process of diaphragm atrophy. Glucocorticoids accelerate the rate of protein catabolism. Optimal concentrations of calcium, magnesium, potassium, phosphate, hydrogen ion, chloride, and carbon dioxide are each important in maximizing muscle performance. Hypoxemia tends to impair endurance more than muscle strength.
Certain commonly used drugs—particularly aminoglycosides and antiarrhythmics (e.g., calcium channel blockers) contribute to weakness in the setting of myasthenia gravis or other underlying neuromuscular impairment (see Chapter 17). Conversely, aminophylline and β-sympathomimetic drugs may modestly improve contractility and endurance. Intriguing experimental data suggest that the resting potential of the skeletal muscle membrane may remain abnormal for days after sepsis control and perhaps after the crisis period of other critical illnesses as well. Moreover, a “critical illness neuropathy” may help explain the prolonged and impressive muscle weakness observed in many of these patients after the acute phase has passed. The extended suppression of neuromuscular excitation by paralytic agents may result in very profound weakness for lengthy periods after they are discontinued, especially when corticosteroids have been used concomitantly as in status asthmaticus (see Chapter 17).
Contractile Fiber Properties
The contractile force developed by a stimulated muscle fiber relates directly to its resting length at the onset of contraction and inversely to its speed of contraction. Force output is, therefore, compromised when a patient inhales rapidly from high lung volume, as so often occurs in breathless, hyperinflated patients with chronic obstructive pulmonary disease (COPD) or asthma (see Chapter 25).
Endurance
Endurance, the ability of a muscle to sustain effort, is determined by the balance between the supply and demand of muscular energy. Hypoxemia, anemia, and ischemia are especially important to correct, because working muscles require an adequate flow of well-oxygenated blood for optimal performance. Although the respiratory muscles normally can access a large recruitable reserve, even this luxuriant supply may be insufficient under conditions of high stress and a failing cardiac pump. Studies of patients with acute ventilatory failure indicate that spontaneous breathing routinely consumes approximately 25% of the oxygen used by the entire body and even more during flagrant respiratory distress. (The normal percentage of respiratory oxygen consumption at rest is 1% to 2%.)
Over the years, many attempts have been made to gauge endurance by comparing spontaneous breathing cycles with maximal voluntary efforts. For example, the ability to voluntarily double [V with dot above]E or tidal volume has been considered a positive predictive
sign. Unfortunately, such voluntary indices require patient cooperation. However, the respiratory pattern gives important clues to ventilatory compensation. The respiratory frequency is the most sensitive but least specific indicator of developing problems. Early in the course of respiratory muscle fatigue, respiratory frequency increases. At the threshold of total exhaustion, frequency may diminish—a harbinger of approaching apnea. The breathing pattern shows variation of tidal volume and I:E ratio when the patient who receives modest support has ample respiratory reserve. In responding to an increased ventilatory workload (e.g., increasing exercise), a well-compensated subject will regularize the breathing pattern and increase both frequency and tidal volume together. Although tidal volume may reach a plateau value while frequency is still rising, tidal volume does not fall during compensated exercise and the ratio of frequency to tidal volume rarely exceeds 50 breaths/min/L, even during vigorous exertion. It has been suggested that a ratio of frequency to tidal volume that exceeds approximately 100 breaths/min/L indicates an unsustainable workload, as the patient fails to generate sufficient pressure to achieve a tidal volume appropriate to the minute ventilation required. The result is inefficient gas exchange and, ultimately, failure to wean from ventilatory support. (There are many exceptions, however, as most patients with restrictive disease naturally start from a higher resting baseline.)
sign. Unfortunately, such voluntary indices require patient cooperation. However, the respiratory pattern gives important clues to ventilatory compensation. The respiratory frequency is the most sensitive but least specific indicator of developing problems. Early in the course of respiratory muscle fatigue, respiratory frequency increases. At the threshold of total exhaustion, frequency may diminish—a harbinger of approaching apnea. The breathing pattern shows variation of tidal volume and I:E ratio when the patient who receives modest support has ample respiratory reserve. In responding to an increased ventilatory workload (e.g., increasing exercise), a well-compensated subject will regularize the breathing pattern and increase both frequency and tidal volume together. Although tidal volume may reach a plateau value while frequency is still rising, tidal volume does not fall during compensated exercise and the ratio of frequency to tidal volume rarely exceeds 50 breaths/min/L, even during vigorous exertion. It has been suggested that a ratio of frequency to tidal volume that exceeds approximately 100 breaths/min/L indicates an unsustainable workload, as the patient fails to generate sufficient pressure to achieve a tidal volume appropriate to the minute ventilation required. The result is inefficient gas exchange and, ultimately, failure to wean from ventilatory support. (There are many exceptions, however, as most patients with restrictive disease naturally start from a higher resting baseline.)
Other components of the respiratory pattern, although harder to quantify, provide equally valuable diagnostic clues. At moderate levels of exertion, pressure in the abdomen rises as the diaphragm contracts, displacing the abdominal contents downward and outward; expiration, which occurs passively at low levels of exertion, often becomes active. Vigorous activity recruits the thoracic musculature, elongating the chest and expanding the rib cage. If diaphragmatic contraction is not proportionately forceful, the abdomen retracts paradoxically during inspiration. When observed in the supine position, this phenomenon, known as paradoxical abdominal motion, indicates a high level of exertion relative to the capability of the diaphragm. Paradoxical abdominal motion may be observed routinely in well-compensated patients with severe airflow obstruction. Some clinicians view the development of this finding as an indicator of established muscle fatigue, but more likely, it should be interpreted as a sign of high workload that may or may not be tolerable. Much less commonly, the ribcage and abdomen alternate primary responsibility for driving inspiration, a pattern known as respiratory alternans. Overt respiratory alternans is much less commonly observed than paradoxical abdominal motion and, when present, often has a neuropathologic origin.
Importance of Muscle Rest
To reverse fatigue, the most effective intervention is to rest the muscles. Total rest is not required but a substantial fraction of the imposed workload must be relieved. Assisted mechanical ventilation, optimally adjusted to meet patient demands, usually allows the patient to rest sufficiently. As a rule, the support level can be assumed adequate if the alert patient is made comfortable. How long a skeletal muscle must be rested before it fully recovers from fatigue is not known with certainty. However, physiologic evidence of subnormal performance can be detected in the laboratory setting for at least 12 to 24 h after brief exposure to a fatiguing load. Therefore, a rest period of at least 12 to 24 h seems appropriate after an episode of acute decompensation. Because recovery may be prolonged, labored breathing risks fatigue and must be avoided.
PREDICTING INDEPENDENCE FROM VENTILATORY SUPPORT
Many predictive indices based on ventilatory performance have been suggested to accurately forecast the outcome of the weaning trial (Table 10-3). However, if the patient is ventilator dependent for reasons unrelated to muscle strength (e.g., hypoxemia, cardiac ischemia, or psychological factors), such indices are of questionable value. Their predictive performance is equally limited after a long period of ventilatory support and for certain patients with permanent neuromuscular deficits. Even when impaired ventilatory power and endurance are responsible, no single index has been universally successful, perhaps because multiple factors cause the patient to remain ventilator dependent. Widely used panels of indicators tests are: [V with dot above]E, muscle strength, muscle reserve, and respiratory mechanics. Patients who are successfully weaned from mechanical support generally have a [V with dot above]E lower than 10 L/min, a maximally negative inspiratory pressure exceeding -20 cm H2O, a vital capacity (VC) more than twofold of the spontaneous tidal volume, and an ability to double the baseline [V with dot above]E on command. In practice, the problem with using such a panel of criteria is twofold: only selected components can be measured in uncooperative patients, and there is uncertainty
when only one or two indices lie within the acceptable range. Thus, although these time-honored criteria are reliably predictive when all are satisfied or violated, they are of questionable assistance in difficult cases. While favorable weaning parameters may support a decision to undertake a weaning attempt, poor parameters should not preclude a carefully observed trial of spontaneous breathing or an attempt to wean if clinical judgment otherwise suggests a favorable outcome (Table 10-4).
when only one or two indices lie within the acceptable range. Thus, although these time-honored criteria are reliably predictive when all are satisfied or violated, they are of questionable assistance in difficult cases. While favorable weaning parameters may support a decision to undertake a weaning attempt, poor parameters should not preclude a carefully observed trial of spontaneous breathing or an attempt to wean if clinical judgment otherwise suggests a favorable outcome (Table 10-4).
TABLE 10-3 PREDICTORS OF WEANABILITYa
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|