Ventricular Tachycardia
Bruce A. Koplan
William G. Stevenson
I. GENERAL PRINCIPLES
A. Definitions.
1. Ventricular tachycardia (VT).
a. ≥3 beats at a rate ≥100 bpm.
b. QRS width ≥0.12 seconds.
c. Originates from the ventricle.
2. Nonsustained ventricular tachycardia (NSVT).
a. Terminates spontaneously within 30 seconds without causing severe symptoms.
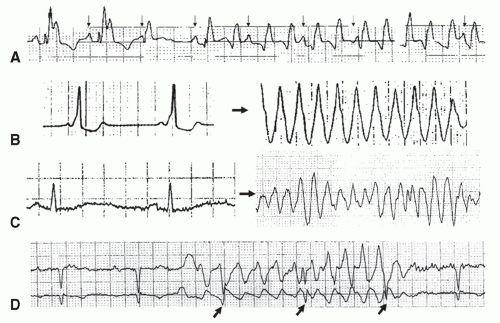
B. Classification (Fig. 35-1).
1. Monomorphic VT. Same configuration from beat to beat.
a. Usually due to a circuit through a region of old myocardial infarction (MI) scar.
b. Idiopathic VT (less common): VT in the absence of an identifiable cause (e.g., structural heart disease/prior MI).
i. Right ventricular outflow tract (RVOT) tachycardia: most common idiopathic VT. Left bundle branch block morphology with inferior axis.
2. Polymorphic VT. Continually changing QRS morphology.
a. Etiologies.
i. Active cardiac ischemia (most common).
ii. Electrolyte disturbance.
iii. Drug toxicity.
iv. Familial.
b. Torsade de pointes.
i. Unique form of polymorphic VT.
ii. Waxing and waning QRS amplitude during tachycardia associated with prolonged QT interval.
iii. Secondary to QT-prolonging drugs, electrolyte abnormalities, or familial ion channel disorders (long QT syndrome).
3. Sinusoidal VT. Sinusoidal appearance often associated with severe electrolyte disturbance (e.g., hyperkalemia).
4. Accelerated idioventricular rhythm (AIVR).
a. Wide complex, ventricular rhythm at 40 to 100 beats/min.
b. Usually hemodynamically stable.
c. Can occur in the first 12 hours after reperfusion of an acute MI or during periods of elevated sympathetic tone.
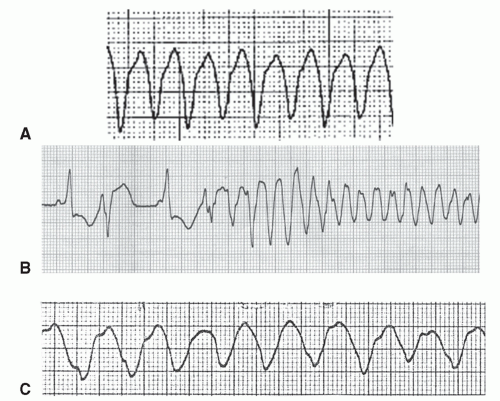 Figure 35-1. Three different wide QRS tachycardias are shown: monomorphic VT in (A); polymorphic VT in (B); and sinusoidal VT due to hyperkalemia in (C). |
d. Onset typically preceded by sinus slowing.
e. Usually resolves without specific therapy.
f. Antiarrhythmic drug (AAD) treatment rarely necessary.
II. DIAGNOSIS
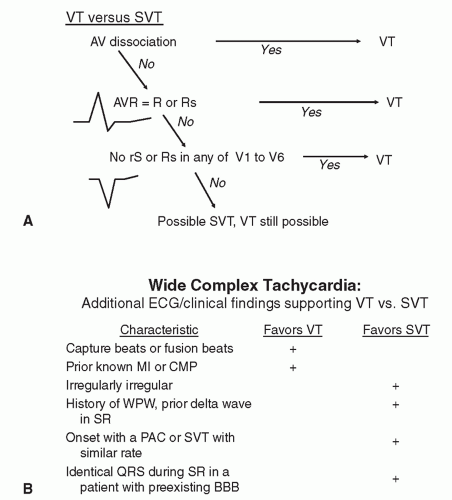
A. Differentiating VT from supraventricular tachycardia (SVT) in a patient with a wide complex tachycardia (WCT).
1. Differential diagnosis of WCT.
a. VT.
b. SVT with aberrancy (bundle branch block).
c. SVT conducting down an accessory pathway (Fig. 35-2B).
2. Assume VT until proven otherwise.
3. WCT with a history of MI should be assumed to be VT unless proven otherwise.
4. If the patient is hemodynamically stable, obtain a 12-lead electrocardiogram (ECG).
5. ECG criteria that favor VT over SVT (Fig. 35-3A and B).
b. Initial R in avR.
c. QRS concordance. Absence of an rS or Rs complex in any precordial lead (V1-V6).
d. Capture beats/fusion beats during tachycardia (Fig. 35-4).
i. Occur when a supraventricular conducts to the ventricles, depolarizing the ventricle (completely—capture beat or partially—fusion beat) in advance of the next tachycardia beat.
ii. Morphologically identical (capture beat) or similar (fusion beat) to the QRS complex seen in sinus rhythm but occur in the midst of a wide QRS complex tachycardia.
iii. Capture beats during WCT are pathognomonic for VT.
6. Additional principles.
a. Hemodynamic instability is dependent on the rate and underlying ventricular function and does not differentiate VT from SVT.
b. Electrocardiographic artifacts can mimic VT/ventricular fibrillation (VF) (Fig. 35-2D).
III. TREATMENT. First priority—Determine whether the patient is hemodynamically stable.
A. Management of hemodynamically unstable VT/VF (see Algorithm, Fig. 35-5).
1. CPR and rapid defibrillation are the most important measures to improve survival.