Links: Criteria | Types of Ventilators | Ventilatory Modes | Non-invasive Ventilation | Initial Settings | Monitoring, Pearls & Suctioning | Respiratory Physiology | Complications of Ventilators | Other Ventilator Considerations | Trouble Shooting | Weaning | Sedation | Prolonged Mechanical Ventilation / Dependence | Intubation | Extubation | Tracheostomy | Non-Invasive | BIPAP | Paralyzing (NM Block) | Ventilator Pneumonia | Tracheostomy | See ARDS | Sepsis |
Routine ordering of a daily CXR for mechanically ventilated pt’s does not seem to improve outcomes compared with a more restrictive approach to chest radiography (Chest 2003;123:1607-14) as there was no differences between groups in mortality rates or in average duration of mechanical ventilation, ICU stay, or total hospital stay. The analysis was based on data for 20,241 pt’s who received mechanical ventilation in 37 hospitals in 2002–2003 found that higher ICU volume was significantly associated with lower ICU and hospital mortality rates (NEJM 2006;355:41-50)…..adjusted ICU mortality (for a pt at average predicted risk for ICU death) was 21.2% in hospitals with 87 to 150 mechanically ventilated pt’s annually Vs 14.5% in hospitals with 401 to 617 mechanically ventilated pt’s annually.
Cell Phones: But modern equipment has shields to protect it from electromagnetic interference and the ban on cell phones has been lifted in some hospitals…even in intensive care units (Prescriber’s Letter 2010;26(4):260402)….Feel comfortable using standard household electronics 6 feet away from sensitive equipment. To be extra safe, switch off cell phones and laptops when closer than 6 feet to critical care equipment. Keep in mind that cell phones might be banned for other reasons, such as protecting patient privacy or reducing disruptions. It becam clear in 2003 that the electromagnetic energy emitted by cell phones may be strong enough to interfere with mechanical ventilators in the ICU, even to the point where a ventilator may shut down, also can cause false alarms and unintentional cycling of ventilators.
• Cellular telephones can interfere with medical equipment, but also reveals that recent technological advances have changed the electromagnetic interference (EMI) landscape for the better (Mayo Clin Proc 2005;80:1286-1290)….the incidence of “clinically important” interferences was 1.2%.
• A study involving 300 tests with 192 medical devices concluded that cell phones produced no noticeable interference or interaction with the medical devices (Mayo Clin Proc 2007;82:282-85) (used two different cellular carriers and 2 Blackberry devices).
• Cell phones with Internet capability (General Packet Radio Service = GPRS) and other bells and whistles can cause life-threatening electrical interference if they’re used too close to medical devices (Critical Care 2007;11: doi:10.1186/cc6115)(shut down ventilators or restated them at different rates, they also shut down syringe pumps without an acoustic alarm or with an incorrect alarm and a cell phone signal led to incorrect inhibition in a test of external pacemakers).
Criteria Parameters:
RR >35/min.
PaCO2 >50mmHg & pH < 7.30.
VC < 10-15 ml/kg.
VD/VT = dead space/ tidal volume >0.60.
FEV1 <10 ml/kg.
Resting Minute Ventilation >20 or <3 L/min.
Max Insp Press < -20 cm H2O.
A-a gradient >450 mmHg.
PaO2 with O2 supplement <55-60 mm Hg.
Other Indications: To improve pulmonary gas exchange in resp. failure of pulmonary or extrapulmonary (chest bellow, central resp. drive) etiology, to incr PAO2 and decr PaCO2. To relieve respiratory distress, decr O2 cost of breathing. To reverse respiratory muscle fatigue. To alter pressure-volume relationships, prevent and reverse atelectasis, improve lung compliance. Reduced CNS resp. drive (intoxication, brainstem CVA). To treat incr ICP by hyperventilating to reduce cerebral blood flow.
Prophylactic –> sepsis, shock, upper GI bleed with aspiration risk (varices), obtundation with loss of protective airway reflexes.
Tips: Always consider individual pt’s characteristics, e.g. PCO2 of 55 in a young asthmatic indicates impending resp. failure, whereas in an elderly COPD’er it may be their baseline. Consider alternative methods of non-invasive ventilation with BiPAP.
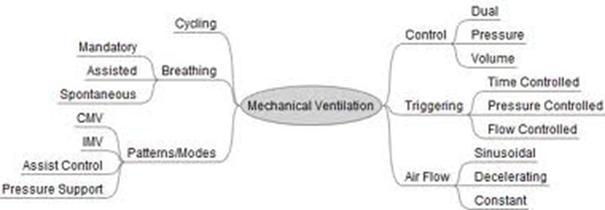
Types of ventilators: Link: Vent Modes |
Ventilation can be delivered to the lung by two methods.
Negative Pressure Ventilator: Non-invasive negative pressure ventilation (NINPV). A negative pressure is applied externally around the thorax (cuirass ventilators). The iron lung used during polio epidemic in 1950’s.
Positive Pressure Ventilator: Raise airway pressure to create inspiratory flow that inflates the lungs, used with cuffed ET tubes. A positive pressure is applied to the lungs via the trachea. This is the method used in theatre and these devices are driven by one of three methods: gas, electricity, or a separate supply of compressed air or oxygen.
There are five types of ventilators:
• Mechanical thumbs: used with T-piece circuits.
• Minute volume dividers.
 • Bag squeezers: widely used with circle systems where a pneumatic bellows device operates intermittently.
• Bag squeezers: widely used with circle systems where a pneumatic bellows device operates intermittently.
• Intermittent flow generators: have a control mechanism that interrupts intermittently a flow of gas from a high pressure source (for example, a cylinder). These can be made compact and are used for ventilation during transportation.
• High frequency ventilators: deliver very small tidal volumes at very high rates to maintain normal gas exchange.
Divided into 4 Categories:
1. Time Cycle –> Timed delivery of gas flow. TV = Flow rate X insp time. Delivers a relatively constant TV to allow for precise control and variability in waveform of delivered gas.
2. Volume-cycled –> most common, reliably delivers set volume of gas at a pre-set flow regardless of pressure. TV (tidal volume) is constant despite fluctuations in respiratory mechanics. TV will not vary with changes in pressure (compliance), unless pressure limit is reached.
3. Pressure-cycled –> Triggered by pt’s inspiratory effort to deliver air at until a preset airway pressure is reached. Inspiration stops when preset pressure reached. TV = Flow rate X Time until pressure reached. Will have variable volume if circuit pressure varies (compliance).
4. High Frequency Ventilators: jet ventilation, oscillation, percussive ventilation. Have low mean airway pressure, but volume increases. Used for closed head injuries, large pulmonary air leaks/ flail chest and refractory respiratory failure.









