KEY POINTS
Heart failure in patients with chronic valvular heart disease is usually precipitated by concurrent illness, progressive deterioration of cardiac function, or worsening valvular disease.
Acute onset of severe valvular regurgitation is uncommon. Clinical and echocardiographic diagnosis is challenging.
Acute severe aortic and mitral regurgitation (flail segments secondary to trauma, aortic dissection, ruptured papillary muscle) are surgical emergencies. Acute severe tricuspid regurgitation is usually better tolerated, but on occasion can lead to cardiogenic shock.
Severe symptomatic aortic stenosis is a surgical disease. Medical treatment is temporizing or palliative.
Transcatheter aortic valve replacement (TAVR) or aortic balloon valvuloplasty should be considered in patients with severe AS and decompensated heart failure.
Hemodynamically significant mitral stenosis should be treated by mechanical intervention on the valve (percutaneous mitral balloon valvuloplasty or surgery). Medical treatment is temporizing or palliative.
Valvular regurgitation, perivalvular extension of infection, and systemic embolization are important complications of infective endocarditis and should be actively sought on clinical examination, ECG, and echocardiography.
Prosthetic valve thrombosis presents with thromboembolic events or heart failure due to valve obstruction. Diagnosis is made by echocardiography or fluoroscopy. Treatment depends on location (left- vs right-sided valves) and thrombus burden.
Structural failure of a mechanical prosthesis is rare and requires urgent reoperation. Failure of a bioprosthesis is frequent and progressive due to degeneration. Reoperation after stabilization is recommended.
INTRODUCTION
Valvular heart disease is one of the most common causes of heart failure. The etiology varies, with degenerative valvular disease being predominant in the Western world and rheumatic disease in developing countries. Patients with critical illness and valvular disease can be separated in two broad categories: (a) patients in whom acute medical illness precipitates heart failure on a background of compensated valvular heart disease and (b) acute valvular lesions causing acute de novo cardiac decompensation. These entities are quite different in presentation, diagnosis, and management. Indeed, decompensated heart failure in the first category is a result of increased demand and/or tachycardia (arrhythmias, pain, anemia, hypotension, hypoxemia, fever) on a background of reduced cardiac reserve due to valvular disease; prompt treatment of the primary cause together with appropriate cardiac and vascular support is the cornerstone of management. In the second category, it is the acute valvular disease itself causing cardiovascular compromise. Medical management is usually only temporizing; many of these patients represent true surgical emergencies.
Physical examination is the first step in the diagnosis of any cardiac disease. This remains true in patients with acute illnesses and coexisting significant valvular disease. Indeed, all patients with critical illness should have a detailed examination of the cardiovascular system to ascertain the presence of valvular lesions. Presence of murmurs, gallops, and/or signs of vascular congestion are important clues to concurrent valvular conditions. It is important to remember that patients with acute severe valvular disease rarely have significant cardiac findings, with substantial discrepancy between quasi-silent cardiac examination and symptoms of extreme dyspnea (reflecting acute pulmonary edema), profound hypotension (cardiogenic shock), and angina (coronary hypoperfusion).
The key diagnostic modality in patients with critical illness and valvular disease is echocardiography. The unique advantages of this imaging modality (available at bedside, immediate interpretation, comprehensive assessment of valvular lesions, and ventricular function) render echocardiography irreplaceable in modern ICU care. Due to its versatility and diagnostic ability, it has largely replaced catheterization as a diagnostic modality in valvular disease; the latter is usually indicated only when discrepancies between echocardiographic and clinical findings are noted. Other routine evaluations (electrocardiography, chest x-ray) are of obvious utility in critically ill patients. In complex situations, cardiac CT and MRI can further complete the diagnosis, but require transportation of the critically ill patient to the specific areas, which is cumbersome.
In this chapter, we will further review the etiology, pathophysiology, clinical presentation, diagnostic evaluation, and management of critical illness in the context of major valvular disease. Acute prosthetic valvular disease and infective endocarditis will be presented at the end of the chapter.
AORTIC STENOSIS
The prevalence of significant aortic valvular heart disease (moderate severity or worse) increases with age, occurring in only 0.7% of those age 18 to 44 years but in 13.3% of adults 75 years and older.1 Native aortic valve stenosis is the most common valvular lesion in clinical practice, followed by mitral regurgitation (25%), and multivalve disease (20%).2 According to location, aortic stenosis (AS) can be classified as subvalvular, valvular, or supravalvular (Fig. 41-1). Subvalvular and supravalvular stenoses result from focal (isolated membrane) or extended (tubular) stenotic lesions. Regardless of lesion type, they lead to impaired flow in the left ventricular outflow tract or aortic root, and are indistinguishable from valvular AS from a hemodynamic perspective. Therefore, their management in critically ill patients is similar to valvular AS.
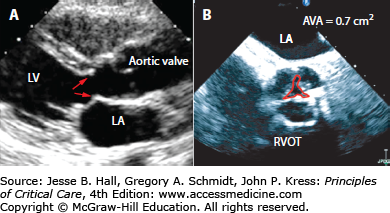
FIGURE 41-1
A. Subaortic membrane demonstrated on transthoracic echocardiography. Note presence of a ridge (red arrows) approximately 1 cm below the aortic valve. Blood flow accelerates at this level, and the high velocity jet can damage the native aortic valve. B. Systolic frame obtained by transesophageal echocardiography in a patient with severe calcific aortic valve stenosis. The maximal aortic valve area (AVA) is 0.7 cm2 by planimetry (red tracing). LA, left atrium; LV, left ventricle; RVOT, right ventricular outflow tract.
The most common cause of valvular AS is degenerative disease of a tricuspid aortic valve. This is very common after the age of 70, leading to significant morbidity and mortality. Surgical series have reported the incidence of degenerative AS as high as 10% to 30%3 but the true prevalence is likely underestimated considering that many patients are not referred for surgical correction. Degeneration of a congenitally malformed aortic valve (bicuspid or unicuspid aortic valves) occurs earlier in life, and patients present with significant valvular disease in the middle or late adult life. It is estimated that 1% to 2% of aortic valves are bicuspid, making this one of the most common congenital heart malformations.4 In both tricuspid and congenitally malformed valves, degeneration of the valve progresses from the base of the cusps to the leaflets, eventually causing a reduction in leaflet motion and effective valve area; commissural fusion is a late phenomenon. Calcific AS is an active disease process characterized by lipid accumulation, inflammation, and calcification, with many similarities to atherosclerosis. In rheumatic AS, stenosis is caused by fusion of the commissures with scarring and eventual calcification. It is less commonly seen in the Western world and is invariably accompanied by various degrees of mitral valve disease.
Classically, AS begins with a prolonged asymptomatic period, in which morbidity and mortality are very low. However, once even moderate disease is present, AS is a relentlessly progressive disease. The average rate of progression is an increase in mean pressure gradient of 7 mm Hg per year, and a decrease in valve area of 0.1 cm2 per year,5 but there is marked individual variability. Regular clinical follow-up is mandatory in all patients with asymptomatic mild to moderate AS.
The key hemodynamic change in AS is a progressively increasing resistance to blood flow. In the Gorlin equation,6 the cardiac output is directly proportional to the square root of the pressure gradient. Therefore, small changes in both cardiac output and valve area may have significant effects on the pressure gradient. Such large variations may lead to confusion in classification of disease severity, as currently used criteria to define severe AS are not necessarily simultaneously present in all patients. Intuitively, aortic valve area should be the best estimate of AS severity as it represents the anatomical obstacle to left ventricular outflow, and is less prone to variations under hemodynamic conditions. Indeed, a valve area of less than 1.0 cm2 was associated with unfavorable outcome regardless of gradient or symptoms.7
Stroke volume and cardiac output are initially maintained by hypertrophy of the left ventricle. The increased wall thickness leads to maintaining wall stress within normal limits, and explains why cardiac output, ejection fraction, and left ventricular cavity dimensions are maintained for a long period. Once compensatory mechanisms are overwhelmed by progressive stenosis, the cardiac output declines, and the left ventricle eventually enlarges. Note that transvalvular gradient actually declines in these late stages, leading to the “low cardiac output, low gradient” type AS.8 Classically, only patients with low EF were included in this category. More recently, emphasis has been placed on patients with pseudonormal left ventricular function. These are individuals in whom a low transvalvular gradient is present despite preserved EF; the low cardiac output in this situation is explained by a combination of low stroke volume and increased valvuloarterial impedance.9 In the absence of surgical intervention the outcome of patients with low cardiac output and severe AS is poor, regardless of type (low EF or normal EF).
Left ventricular hypertrophy maintains contractile function, but will ultimately lead to relaxation abnormalities (diastolic dysfunction), resulting in elevated left atrial pressure and secondary pulmonary hypertension. Ischemia may develop due to both concomitant coronary artery disease (present in ∼50% of patients with severe AS) and endocardial ischemia due to increased wall thickness and coronary hypoperfusion. A particularly dangerous situation is created by any sudden reduction in blood pressure or systemic vascular resistance (such as that seen in sepsis or with the use of vasodilating drugs). This decreases coronary perfusion pressure, with global ischemia, precipitous further fall in cardiac output and ultimately cardiac arrest. Therefore, use of vasodilators and diuretics needs to be cautious in patients with severe AS.
AS remains essentially a surgical disease, with correction of stenosis bringing about significant improvement in cardiac function. This leads to further decrease in right heart pressures and left ventricular filling pressures. Left ventricular hypertrophy regresses early, sometimes eventually to a normal mass. While uniform improved outcomes are seen after surgical correction, the magnitude of benefit is largely dictated by the disease severity. Indeed, patients with low cardiac output, dilated ventricles, and low ejection fraction have the worst response, especially if no contractile reserve is present.
In the critically ill patient, presentation with severe AS is a reflection of acute decompensation, often due to a concurrent condition because AS severity progresses otherwise slowly. Acute decompensated heart failure in patients with severe AS is characterized by presence of dyspnea, less so by angina or syncope. Some patients complain of nonspecific symptoms such as fatigue, dizziness, or palpitations. A particular presentation is that of decompensated heart failure in patients with severe AS undergoing noncardiac surgery. In this situation, large volume shifts and vasodilation associated with surgical procedure and anesthesia may lead to acute decompensation. Indeed, among valvular diseases AS is associated with the highest risk of perioperative complications, up to 10% mortality in some series.10
Physical examination can suggest presence of AS. The apical impulse is usually sustained, and is not significantly displaced unless the ventricle has dilated. The hallmark auscultatory findings are presence of the AS systolic murmur and the absence of the aortic component of the second heart sound. The murmur is crescendo-decrescendo and is usually heard throughout the precordium. With severe AS, the peak is late in systole, and the murmur radiates to the carotid and subclavian arteries. As the blood fluid column in the LVOT ensures good transmission of sound waves to the apex, the AS murmur may be sometimes louder at the apex, thereby mimicking mitral regurgitation; the latter is holosystolic, and usually radiates to the axilla. The carotid impulse is generally diminished in volume and has a delayed, slow-rising peak; this finding may be absent in the elderly, where increased aortic stiffness preserves the pulse strength. Note that auscultatory findings may be trivial or even absent in patients with severe AS and low ejection fraction, and in those with severe COPD.
The electrocardiogram is nonspecific, and does not help in assessment of AS severity. Left ventricular hypertrophy with secondary repolarization abnormalities (strain pattern) as well as ischemic changes can be seen. The chest x-ray can show valvular calcifications. Nonspecific findings of decompensated heart failure (pulmonary venous congestion or frank pulmonary edema, pleural effusions, cardiomegaly) need to be actively sought.
Echocardiography remains the cornerstone of diagnosis in all valvular diseases, both in chronic and acute decompensated states. It provides an anatomical diagnosis (degenerative vs rheumatic vs supra/subvalvular AS) as well as comprehensive hemodynamic assessment. Transvalvular gradients correlate well with those measured directly in the catheterization laboratory; calculated valve areas by continuity equation (echo) or Gorlin formula (cath lab) are similarly close. It is important to remember that high-quality, comprehensive evaluation is a prerequisite for accurate measurement of the aortic valve. Indeed, aortic valve area calculation by echocardiography includes squaring of the LVOT diameter; small errors in this measurement can lead to significant over- (more common) or underestimation (less common) of disease severity. In addition, comprehensive interrogation of the aortic valve gradient from multiple windows must be performed to ensure capturing the highest gradient.
In the current ACC/AHA Valvular Heart Disease Guidelines,5 AS is classified into mild, moderate, and severe according to echocardiographic findings. A velocity >4 m/s, gradient >40 mm Hg, and valve area <1.0 cm2 are consistent with severe disease. These criteria have been criticized as being intrinsically discordant,11 as up to 30% of patients with calculated valve area of less than 1 cm2 will not have velocities and gradients in the severe range. Some of these patients have low gradients due to low cardiac output and true AS, while others may have low calculated valve areas in the context of a nonvalvular myopathic process rendering the left ventricle unable to generate enough pressure for full valve opening (pseudosevere AS). Low-dose dobutamine echocardiography is helpful in diagnosis.12 Indeed, when cardiac output increases on the background of true severe AS, this will result in a corresponding increase in transvalvular gradients, and the calculated valve area remains in the severe range (Fig. 41-2). On the contrary, in patients with pseudosevere AS, an increase in contractile function leads to improved opening of the aortic valve, and the increase in cardiac output results in an increased valve area. Dobutamine stress echocardiography has also prognostic value for the outcome of surgery. Indeed, patients demonstrating presence of contractile reserve (at least 20% increase in stroke volume and cardiac output) have a low operative risk and a good long-term prognosis, whereas operative mortality is high in the absence of contractile reserve.8 However, patients with severe low-gradient AS may benefit from surgery even in the absence of contractile reserve, and need careful assessment.
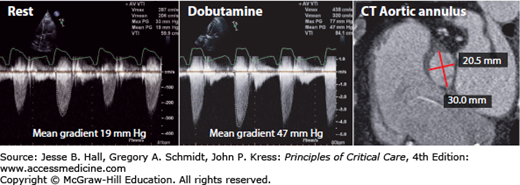
FIGURE 41-2
Low-dose dobutamine-stress echocardiogram in a patient with low-flow, low-gradient aortic stenosis. Note very low gradient at rest (19 mm Hg) that increases sharply to 47 mm Hg with dobutamine. Valve area was calculated 0.8 cm2. In this patient, chest CT was performed for assessing feasibility of transcatheter aortic valve replacement (TAVR) and demonstrated marked oval shape of the aortic annulus, with a long diameter of 30 mm and short diameter of 20.5 mm (red lines). This information is used for selection of appropriate prosthesis size.
Cardiac CT has been increasingly used in assessment of AS. Presence of heavily calcified valve is associated with rapid progression of the disease, and correlates with aortic valve area.13 With the advent of transcatheter aortic valve replacement (TAVR), CT has been also used for determining the shape and size of the aortic annulus. Indeed, the annulus is often oval shaped, with a major and minor diameter. Determining the size of aortic prosthesis solely on long-axis echo images may lead to undersizing and significant periprosthetic regurgitation after TAVR.14
Whenever discrepancies exist between clinical and echocardiographic findings, cardiac catheterization can be performed for assessment of severity of AS. While early stages of AS have normal cardiac output, normal right heart and pulmonary capillary wedge pressures, and a normal ejection fraction, patients with decompensated heart failure will obviously have elevated filling pressures, with high left ventricular end-diastolic pressure and wedge pressure. In advanced states, the cardiac output and ejection fraction will be depressed. Coronary angiography is usually performed in a single study, as many patients with severe AS require surgical intervention.
Regardless of etiology, AS is a mechanical problem and the only effective long-term treatment is a mechanical intervention to relieve the obstruction to outflow. For stable patients, onset of symptoms, evidence of left ventricular dysfunction (EF <50%), and need for bypass or thoracic aortic surgery are the class I indications for aortic valve replacement.
Patients with critical noncardiac disease and severe AS pose a significant challenge in management. Due to fixed obstruction, the increased cardiac output required for tissue perfusion in sepsis or profound anemia may not be adequate. The need for urgent noncardiac surgery in patients with severe AS puts a patient at a very high risk for cardiac complications, including myocardial infarction, congestive heart failure, and death.15
Treatment of critically ill patients with decompensated severe AS is complex, and consists of stabilizing measures (typically undertaken in the intensive care settings) followed when possible by mechanical interventions on the stenotic valve. Medical measures aim at maintaining cardiac output and coronary perfusion pressure. All medications have the potential for acute decompensation, and close monitoring is required. Diuretics are frequently used, but dosing should be cautious. We favor an initial small intravenous bolus followed by continuous furosemide infusion, as it allows rapid achievement of a steady state, and leads to less hemodynamic instability caused by the vasodilating effect of intermittent dosing. The intensity of diuretic regimen can be further titrated to the desired effect. As diuretics decrease preload, excessive dosing can rapidly impair cardiac output in AS patients who are very preload dependent. Blood pressure needs to be carefully monitored, and episodes of hypotension must be promptly treated, usually by administering a peripheral vasoconstricting agent such as phenylephrine. Indeed, any significant decrease in systemic blood pressure results in a decrease in coronary perfusion pressure, and leads to a rapidly spiraling cardiac decompensation. Positive inotropic agents such as dobutamine can also be used, but care should be taken to avoid tachycardia as it reduces cardiac output and may lead to ischemia due to increased oxygen consumption. Other medications commonly used in heart failure, such as ACE inhibitors or angiotensin receptor blockers are rarely considered, as the relief of obstruction is the established approach to be considered. Digitalis can be used in patients with depressed ejection fraction or atrial fibrillation. In patients with acute pulmonary edema due to AS, nitroprusside infusion may be used under the guidance of invasive hemodynamic monitoring.16 This should be done cautiously, and used only as a temporizing measure until a mechanical intervention on the AS can be performed. Preexisting β-blockers used for angina/heart failure must be decreased or suspended during acute decompensation, then cautiously reintroduced in a stepwise fashion.
Coronary perfusion and cardiac output can be further augmented by mechanical assist devices, most commonly intra-aortic balloon pump (IABP). Positioning can be guided by either fluoroscopy or TEE, with the tip of balloon a few centimeters below the subclavian artery takeoff. This should not delay the urgent relief of AS by surgical (aortic valve replacement) or percutaneous approach (TAVR or aortic balloon valvuloplasty). Atrial fibrillation must be aggressively controlled, and restoration of sinus rhythm should be considered whenever reasonable; if cardioversion is unsuccessful, pharmacological control of the ventricular rate is essential. Therefore, the acute medical management of severe AS with congestive heart failure consists of the careful use of diuretics, with either positive inotropes (dobutamine) and/or afterload reduction (nitroprusside), being careful not to cause hypotension.
Mechanical intervention to remove the obstruction is the only treatment associated with long-term success. Until recently, the only option was surgical replacement of the aortic valve. Regardless of the approach (percutaneous vs standard sternotomy), it is preferable to stabilize the patient, as emergent surgery carries substantial risks. We found the Society of Thoracic Surgeons (STS) risk score useful in estimating the risk for aortic valve replacement, even if observed morbidity and mortality at our institution are significantly lower than predicted values. The surgical concept that “it is never too late to operate on aortic stenosis” must be judged in a heart team approach, carefully understanding the associated risks.
Development of TAVR technology has provided a much needed alternative in patients with advanced AS and high risk for surgery17 (Fig. 41-3). The Edwards SAPIEN valve has been approved for transfemoral implantation and another device (CoreValve) is under clinical investigation in the United States. Both devices have been approved in numerous other countries. TAVR is superior to medical management in inoperable patients, reducing mortality in half.17 In high-risk but operable patients, outcomes of TAVR and standard surgery are similar, albeit at a higher risk of stroke.
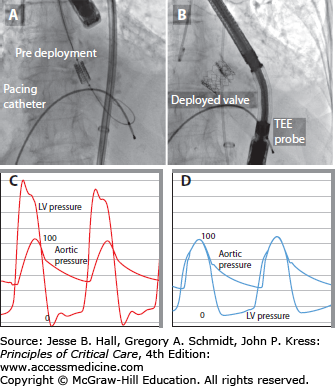
FIGURE 41-3
Transcatheter aortic valve replacement (TAVR). A. Predeployment, the Edwards-Sapien valve is crimped on a delivery balloon and advanced into position under fluoroscopic guidance. A temporary right ventricular pacing catheter allows pacing at rates ∼180 bpm at the time of delivery, ensuring minimal stroke volumes, and thereby minimizing the risk of the valve being pushed out of ideal position at the time of balloon inflation. B. Postdeployment the valve stent is visible in aortic position. The function is immediately evaluated by TEE. Note dramatic change in transvalvular gradients from baseline (C) to postdeployment (D).
The recently developed TAVR has also led to resurgence in the use of aortic balloon valvuloplasty, as a temporizing measure.18 The procedure consists of mechanical stretching with a balloon positioned across the stenotic valve, and is associated with an immediate improvement in transvalvular gradients and cardiac output, despite usually small changes in calculated valve area (rarely exceeding 1 cm2). Complications are significant, with stroke, myocardial infarction, acute aortic regurgitation, and death occurring in as many as 10% of the patients. Restenosis invariably occurs within 6 months. The procedure has been used in patients with cardiogenic shock,19 patients requiring major noncardiac surgery,20 and as bridge to delivery in symptomatic pregnant women. After recovery, definitive aortic valve replacement by surgery or TAVR can be performed at a later date.
KEY POINTS—AORTIC STENOSIS
Severe AS is a surgical disease.
AS occurs mostly due to degeneration of tricuspid or bicuspid valves. Rheumatic AS is uncommon.
Increased afterload leads to hypertrophy and ultimately failure. Relief of the mechanical obstacle often reverses ventricular dysfunction.
Acute presentation is usually with dyspnea, less common with syncope or angina.
Harsh, loud, midsystolic murmur and decreased S2 are typical of severe AS. This may be reduced or absent in patients with reduced ejection fraction.
Echocardiography is the cornerstone of diagnosis. Valve area <1.0 cm2 and gradient ≥40 mm Hg are diagnostic of severe AS.
Low output/low gradient AS can be diagnosed with low-dose dobutamine stress. Presence of contractile reserve predicts good outcome.
Cardiac catheterization verifies severity of AS in difficult cases and provides preoperative coronary angiography.
Medical management is only temporizing.
Temporizing aortic balloon valvuloplasty may be used.
Surgical or transcatheter aortic valve replacement are the only treatments with long-term success. Decision should be made by the heart team (surgeon and cardiologist).
AORTIC REGURGITATION
The presentation and management of patients with severe aortic regurgitation (AR) depends on the nature of underlying disease. Acute severe AR is rare, but is a true medical and surgical emergency. It can be the result of endocarditis (leaflet or annular destruction), aortic dissection (compromised leaflet coaptation), or traumatic (leaflet or annular tear/rupture from blunt chest trauma or aortic balloon valvuloplasty; the aortic valve is the most commonly involved valve in blunt chest trauma) (Fig. 41-4). Chronic AR may be secondary to diseases of the valve leaflets (calcific degeneration, rheumatic, myxomatous) or to abnormalities of the aortic root (Marfan and Ehlers-Danlos syndromes; aortitis in ankylosing spondylitis, syphilis, rheumatoid arthritis, giant cell aortitis, Reiter syndrome).5 It is a disease that progresses slowly, and does not require treatment unless symptomatic or when left ventricular dysfunction becomes evident. However, acute cardiac decompensation on a background of severe AR may also represent a medical emergency.
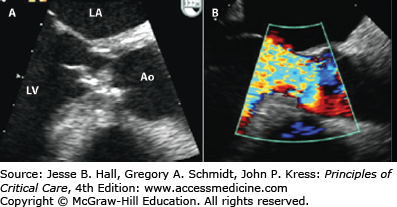
FIGURE 41-4
This case illustrates the dramatic differences in echocardiographic appearance of acute aortic regurgitation (resulting from a flail anterior leaflet as a complication of aortic balloon valvuloplasty; top row) versus chronic aortic regurgitation (destroyed anterior leaflet by endocarditis in a patient with long-standing aortic regurgitation and bicuspid aortic valve; bottom row). A. The anterior leaflet of the aortic valve was confirmed to be flail at TEE, and prolapses into the left ventricular outflow tract (arrow). B. The Color Doppler obtained few minutes earlier by transthoracic echocardiography is unimpressive, with a brief flash of color at the aortic valve plane. Ao, ascending aorta; LA, left atrium; LV, left ventricle.
Presence of chronic AR leads to both volume overload (the left ventricle has to accommodate the regurgitant volume) and pressure overload (increased afterload due to increased wall stress and systolic pressure). The left ventricle dilates progressively, with both eccentric and concentric hypertrophy. The increased diastolic volume allows for augmentation of stroke volume (Frank-Starling mechanism), and maintains cardiac output in the normal range for many years despite presence of severe AR. Once compensatory mechanisms are overwhelmed, the disease tends to progress rapidly. Left ventricular volumes (left ventricular end-systolic diameter >50 mm, left ventricular end-diastolic diameter >70 mm) can be used to predict which patients are more likely to have progressive disease and the development of left ventricular failure. Indexed left ventricular dimensions are better predictors in patients of small body size and in women.21
In acute onset AR, the left ventricle has to accommodate suddenly a large regurgitant volume. Left ventricular dilation is limited by the compliance of the ventricle and by the constraining pericardium. As such, small increase in regurgitant volume may lead to a dramatic increase in left ventricular diastolic pressure. This leads to an increase in left atrial pressure, causing pulmonary congestion/edema. The combination of decreased aortic diastolic pressure and increased left ventricular diastolic pressure leads to a dramatic decrease in coronary perfusion pressure. Acute AR is especially difficult to tolerate by patients with a very stiff left ventricle due to preexisting concentric hypertrophy; this entity is now more commonly present with a resurgence of aortic balloon valvuloplasty (postdilatation AR) and increasing use of TAVR (periprosthetic AR).
Patients with decompensation of chronic long-standing AR have the classical features of AR in addition to the signs and symptoms of the acute decompensated state. The heart is enlarged, with displaced apical impulse. The heart sounds are usually normal (unless pulmonary hypertension is present). There is a soft diastolic decrescendo murmur best heard over the aortic area, radiating along the parasternal border. A diastolic rumble (Austin-Flint) can sometimes be heard at the apex. The peripheral pulse has a rapid upstroke, and pulse pressure is wide; classic peripheral signs of AR are less common.
Patients with acute severe AR are critically ill, with a discrepancy between the symptom severity (intense dyspnea due to acute pulmonary edema) and paucity of clinical findings. Signs of pulmonary edema and cardiogenic shock are present (tachycardia, hypotension, diaphoresis, and peripheral vasoconstriction), but cardiac examination is underwhelming. As the aortic and left ventricular pressure rapidly equalize, the murmur of acute AR is subdued and early diastolic, if present at all. The heart is not enlarged. The first heart sound may be soft, owing to premature closure of the mitral valve caused by the aortic regurgitant jet. The P2 component of the second heart sound may be loud, reflecting pulmonary hypertension. A gallop rhythm is usually present. Arterial hyperpulsatility and large blood pressure differential coexistent with congestive heart failure are clues to diagnosis of severe AR.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree