Use of Ultrasound for Placement of Peripheral Nerve Block Catheters
R. Scott Lang
Paul E. Bigeleisen
Steven L. Orebaugh
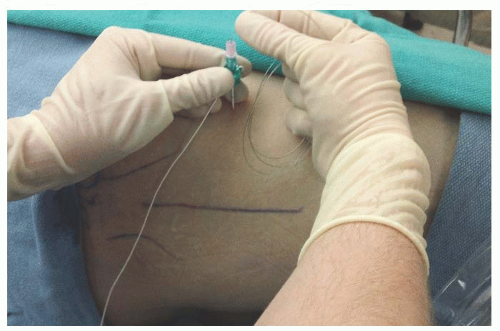
The insertion of catheters percuTaneously to allow the infusion of local anesthetic solutions was initially described by Ansbro in 1946.1 Techniques for placement of catheters have evolved from elicitation of paresthesias, to fascial clicks,2 and subsequently to fluoroscopy,3 nerve stimulator, and ultrasound imaging. The most popular method for inserting catheters is a through-the-needle technique (Fig. 14.1), although catheter-over-the-needle techniques have been reported as well. Placement of a continuous catheter offers some distinct advantages compared to single-injection techniques. In particular, the duration of nerve blockade is a major advantage. Although there are many adjuncts that have been studied to increase the duration of single-injection peripheral nerve blockade, none have been shown to consistently result in analgesia for multiple days to weeks as can catheter techniques.4,5 A catheter can also permit titration of the dose of local anesthetic to increase analgesia or decrease motor blockade to encourage participation in physical therapy. Catheters also provide flexibility in discontinuation and continuation of infusion as dictated by patient care. These benefits have encouraged the use of catheters throughout the body.
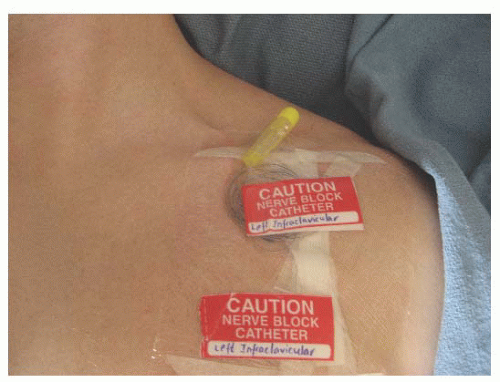
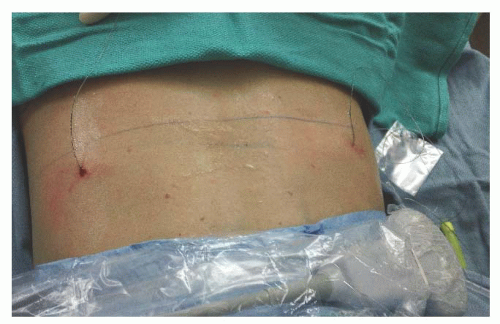
Continuous nerve blockade is used to provide analgesia for surgeries of the upper extremity (Fig. 14.2), thoracic and abdominal areas (Fig. 14.3), and lower extremity (Fig. 14.4). Upper extremity applications include blocks at the interscalene, supraclavicular, cervical paravertebral, suprascapular, infraclavicular, and axillary sites. Thoracic and abdominal catheter techniques include paravertebral, intercostal, epidural, transversus abdominis plane, rectus sheath, and ilioinguinal/iliohypogastric blocks. Finally, catheters for lower extremity surgeries may be inserted at the lumbar plexus, femoral, parasacral, paravertebral, lateral femoral cuTaneous, obturator, fascia iliaca, sciatic, and saphenous regions. The use of ultrasound helps identify the nerves in many of these techniques and allows flexibility in the approach to each. As experience with continuous catheter techniques in a myriad of anatomic regions has accumulated, so has the literature on proper placement, use, and complications.
Peripheral nerve blockade has been associated with neurologic injuries; catheter knotting6, 7and 8; catheter migration and dislodgement; catheter obstruction; fluid leakage; neural irritation9; inflammation; colonization; abscess formation; sepsis; hematoma formation10,11; myotoxocity12; and catheter shearing, breakage, and retention. Inaccurate placement of catheters has also been reported, with catheter tips too far from the nerve, intraneural placement, intravascular insertion, inadvertent intrathecal or epidural penetration, and intrapleural placement. Considering these risks and complications, it is essential to ensure proper placement of the catheter and confirm its position, especially if they are to be used in the ambulatory setting.
 Figure 14.1. A: Image of a multiorifice peripheral nerve catheter through a needle. B: Ultrasound image needle. FA, femoral artery; FN, femoral nerve; LA, local anesthetic; N, needle. |
Benefits of ultrasound
Ultrasound technology has enabled the regional anesthesiologist to place catheters under realtime imaging and to assess position after successful placement (Fig. 14.5). This has become the sTandard of care in many institutions for many peripheral nerve block techniques, especially those areas in close proximity to the neuraxis or blood vessels. Ultrasound guidance and nerve stimulation techniques remain popular techniques to place continuous catheters efficiently and effectively. Although nerve stimulation techniques continue to be utilized, either alone or in conjunction with ultrasound techniques, there are times when nerve stimulation may be undesirable due to discomfort from local muscle contraction. Compared
to nerve stimulation techniques, ultrasound guidance has been shown to improve success rates,13,



to nerve stimulation techniques, ultrasound guidance has been shown to improve success rates,13,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree