CHAPTER 183
Urticaria, Acute
(Hives)
Presentation
The patient is generally very uncomfortable with intense itching. There may be a history of similar episodes and perhaps a known precipitating agent (bee or fire ant sting, food, or drug). More often, the patient will only have a rash. Sometimes this is accompanied by nonpitting edematous swelling of the lips, face, hands, and/or genitalia (angioedema). In the more severe cases, patients may have associated abdominal pain and vomiting (especially if an offending allergen was ingested), wheezing, laryngeal edema, and/or frank cardiovascular collapse (anaphylaxis).
Lesions may occur anywhere on the body. The urticarial rash consists of sharply defined, slightly raised wheals surrounded by erythema and tends to be circular or appear as incomplete rings (Figures 183-1 to 183-3). Each eruption is transient, lasting no more than 8 to 12 hours, but may be replaced by new lesions in different locations. It is not unusual to see these characteristic wheals appear or disappear from areas on the patient’s body, even during a brief encounter. The edematous central area can be pale in comparison with the erythematous surrounding area. These eruptions may occur immediately after exposure to an allergen, or they may be delayed for several days. Allergic reactions to foods or medications are self-limited, typically 1 to 3 days, but will recur with repetitive exposures to cross-reactive substances. Urticaria can sometimes last for 1 to 3 weeks with some drug reactions.

Figure 183-1 Hives. The most characteristic presentation is uniformly red edematous plaques surrounded by a faint white halo. (From Habif T: Clinical dermatology, ed 4. St Louis, 2004, Mosby.)

Figure 183-2 Hives. Urticarial plaques in different stages of formation. (From Habif T: Clinical dermatology, ed 4. St Louis, 2004, Mosby.)
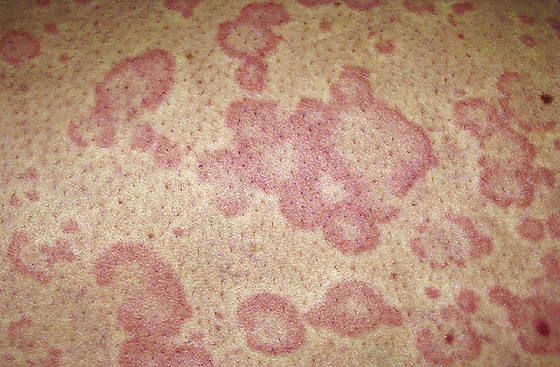
Figure 183-3 Superficial hives vary in color. (From Habif T: Clinical dermatology, ed 4. St Louis, 2004, Mosby.)
Contact urticaria (in which contact of the skin with an allergen, such as latex, causes hives at the site of contact) may be complicated by angioedema and even severe anaphylaxis (see Chapter 160).
What To Do:
 If the respiratory tract is involved, the first priority must be to secure the airway, which occasionally may require intubation. Administer oxygen and establish an intravenous line. For these and other severe systemic reactions, administer intramuscular adrenaline to reduce the edema. A dose of 0.3 to 0.5 mg of epinephrine (0.3-0.5 mL of a 1:1000 dilution) should be given IM every 10 to 15 minutes until symptoms subside, and normal saline should be given intravenously in generous boluses to correct hypotension. Diphenhydramine (Benadryl), 50 mg, should be given IV (or IM if there is no venous access). Solu-Medrol, 40 mg, given intravenously will not provide immediate relief but may reduce the possibility of relapse. Patients with severe angioedema should be admitted for at least 24 hours of observation and further treatment as required. Glucagon may have a role in refractory anaphylaxis when the patient is taking a beta-blocker. The recommended dose is 1 to 5 mg IV over 5 minutes. H2 blockers, such as Pepcid or Zantac may be useful in some patients (responders are unpredictable), and IV epinephrine can be given on very rare (vascular collapse) situations.
If the respiratory tract is involved, the first priority must be to secure the airway, which occasionally may require intubation. Administer oxygen and establish an intravenous line. For these and other severe systemic reactions, administer intramuscular adrenaline to reduce the edema. A dose of 0.3 to 0.5 mg of epinephrine (0.3-0.5 mL of a 1:1000 dilution) should be given IM every 10 to 15 minutes until symptoms subside, and normal saline should be given intravenously in generous boluses to correct hypotension. Diphenhydramine (Benadryl), 50 mg, should be given IV (or IM if there is no venous access). Solu-Medrol, 40 mg, given intravenously will not provide immediate relief but may reduce the possibility of relapse. Patients with severe angioedema should be admitted for at least 24 hours of observation and further treatment as required. Glucagon may have a role in refractory anaphylaxis when the patient is taking a beta-blocker. The recommended dose is 1 to 5 mg IV over 5 minutes. H2 blockers, such as Pepcid or Zantac may be useful in some patients (responders are unpredictable), and IV epinephrine can be given on very rare (vascular collapse) situations.
 In all cases, attempt to elicit a hidden precipitating cause, including stings, drugs, or foods. Obtain the patient’s medical history, focusing on a history of allergy, asthma, or any other preexisting, atopic conditions (i.e., allergic rhinitis and atopic dermatitis). Question patients about their use of all drugs, especially penicillin and sulfa drugs and their derivatives, aspirin (which they may not think of as a drug or which may be hidden in Alka-Seltzer or other over-the-counter [OTC] remedies), oral contraceptives, herbal and vitamin supplements, and foods or drugs containing tartrazine (FD&C yellow dye #5), nitrates, nitrites, sulfites, monosodium glutamate, and aspartame (NutraSweet), among others. Inquire about the foods eaten 6 to 12 hours before developing the rash. Pay particular attention to tree nuts, peanuts, shellfish, eggs, soy, dairy products, and fish, as well as fresh fruits (e.g., kiwi fruit, banana, avocado, strawberries, and tomatoes).
In all cases, attempt to elicit a hidden precipitating cause, including stings, drugs, or foods. Obtain the patient’s medical history, focusing on a history of allergy, asthma, or any other preexisting, atopic conditions (i.e., allergic rhinitis and atopic dermatitis). Question patients about their use of all drugs, especially penicillin and sulfa drugs and their derivatives, aspirin (which they may not think of as a drug or which may be hidden in Alka-Seltzer or other over-the-counter [OTC] remedies), oral contraceptives, herbal and vitamin supplements, and foods or drugs containing tartrazine (FD&C yellow dye #5), nitrates, nitrites, sulfites, monosodium glutamate, and aspartame (NutraSweet), among others. Inquire about the foods eaten 6 to 12 hours before developing the rash. Pay particular attention to tree nuts, peanuts, shellfish, eggs, soy, dairy products, and fish, as well as fresh fruits (e.g., kiwi fruit, banana, avocado, strawberries, and tomatoes).
 If the cause is identified, it should be removed or avoided. In food or drug hypersensitivity, future avoidance is critical.
If the cause is identified, it should be removed or avoided. In food or drug hypersensitivity, future avoidance is critical.
 Perform a general physical examination, with special attention to the skin, to determine the location of lesions and their morphology. Urticaria should present as nontender erythematous cutaneous elevations that blanch with pressure.
Perform a general physical examination, with special attention to the skin, to determine the location of lesions and their morphology. Urticaria should present as nontender erythematous cutaneous elevations that blanch with pressure.
 For immediate relief of severe pruritus, especially if accompanied by systemic symptoms, such as wheezing or hoarseness (although not life threatening as noted previously), give 0.3 mL of epinephrine (1:1000) intramuscularly; this may need to be repeated. If the lesions do not clear with epinephrine, the patient most likely does not have urticaria. Because of the potential for unpleasant side effects, epinephrine use can be omitted for most urticarial reactions that are less intense.
For immediate relief of severe pruritus, especially if accompanied by systemic symptoms, such as wheezing or hoarseness (although not life threatening as noted previously), give 0.3 mL of epinephrine (1:1000) intramuscularly; this may need to be repeated. If the lesions do not clear with epinephrine, the patient most likely does not have urticaria. Because of the potential for unpleasant side effects, epinephrine use can be omitted for most urticarial reactions that are less intense.
 For relief of rash and itching, administer H1 blockers—diphenhydramine (Benadryl), 25 to 50 mg IV, or hydroxyzine (Vistaril, Atarax), 50 mg PO or IM stat—followed by a prescription for 25 to 50 mg PO qid, or cyproheptadine hydrochloride (Periactin), 4 mg tid (all of which can be sedating). Alternatively, give nonsedating cetirizine (Zyrtec), 10 mg qd to bid or fexofenadine (Allegra), 60 to 180 mg qd for the next 48 to 72 hours. Patients might prefer nonsedating antihistamines during the day and sedating antihistamines at night to help with sleep.
For relief of rash and itching, administer H1 blockers—diphenhydramine (Benadryl), 25 to 50 mg IV, or hydroxyzine (Vistaril, Atarax), 50 mg PO or IM stat—followed by a prescription for 25 to 50 mg PO qid, or cyproheptadine hydrochloride (Periactin), 4 mg tid (all of which can be sedating). Alternatively, give nonsedating cetirizine (Zyrtec), 10 mg qd to bid or fexofenadine (Allegra), 60 to 180 mg qd for the next 48 to 72 hours. Patients might prefer nonsedating antihistamines during the day and sedating antihistamines at night to help with sleep.
 Adding H2 blockers to H1 antagonists results in improved clearing of urticaria. Therefore combine one of the antihistamines mentioned with cimetidine (Tagamet), 300 mg IV/IM/PO, ranitidine (Zantac), 50 mg IV or 150 mg PO, or famotidine (Pepcid), 20 mg bid. Follow this with a prescription for cimetidine, 400 mg bid, or ranitidine, 150 mg bid, for the next 48 to 72 hours.
Adding H2 blockers to H1 antagonists results in improved clearing of urticaria. Therefore combine one of the antihistamines mentioned with cimetidine (Tagamet), 300 mg IV/IM/PO, ranitidine (Zantac), 50 mg IV or 150 mg PO, or famotidine (Pepcid), 20 mg bid. Follow this with a prescription for cimetidine, 400 mg bid, or ranitidine, 150 mg bid, for the next 48 to 72 hours.
 To help reduce the likelihood of recurrence, give prednisone, 60 mg PO stat, and prescribe 20 to 50 mg qd for 4 days. When possible, avoid systemic corticosteroids in patients with diabetes, active peptic ulcers, or other steroid risks.
To help reduce the likelihood of recurrence, give prednisone, 60 mg PO stat, and prescribe 20 to 50 mg qd for 4 days. When possible, avoid systemic corticosteroids in patients with diabetes, active peptic ulcers, or other steroid risks.
 In chronic resistant cases, the tricyclic antidepressant doxepin (Sinequan) can be used in doses of 10 to 50 mg qhs. This drug has activity against both H1 and H2 histamine receptors and is 700 times more potent than diphenhydramine. Sedation is common. Leukotriene modifiers, such as montelukast (Singulair), 10 mg qd, and zafirlukast (Accolate), 20 mg bid, in combination with antihistamines may also provide additional benefit in chronic cases.
In chronic resistant cases, the tricyclic antidepressant doxepin (Sinequan) can be used in doses of 10 to 50 mg qhs. This drug has activity against both H1 and H2 histamine receptors and is 700 times more potent than diphenhydramine. Sedation is common. Leukotriene modifiers, such as montelukast (Singulair), 10 mg qd, and zafirlukast (Accolate), 20 mg bid, in combination with antihistamines may also provide additional benefit in chronic cases.
 Inform the patient that the cause of hives cannot be determined in most cases. Let him know that the condition is usually of minor consequence but can at times become chronic and, under unusual circumstances, is associated with other illnesses. Therefore, with recurrent symptoms, the patient should be provided with elective follow-up care, preferably by an allergist.
Inform the patient that the cause of hives cannot be determined in most cases. Let him know that the condition is usually of minor consequence but can at times become chronic and, under unusual circumstances, is associated with other illnesses. Therefore, with recurrent symptoms, the patient should be provided with elective follow-up care, preferably by an allergist.
 Patients with suspected food allergies can be referred to the Food Allergy and Anaphylaxis Network at (800) 929-4040 (www.foodallergy.org).
Patients with suspected food allergies can be referred to the Food Allergy and Anaphylaxis Network at (800) 929-4040 (www.foodallergy.org).
 Patients who experience a more severe reaction should be given a prescription for injectable epinephrine (EpiPen or EpiPen Jr., Ana-Kit), which should be available to them at all times, and they should be advised to wear a MedicAlert bracelet inscribed with this information.
Patients who experience a more severe reaction should be given a prescription for injectable epinephrine (EpiPen or EpiPen Jr., Ana-Kit), which should be available to them at all times, and they should be advised to wear a MedicAlert bracelet inscribed with this information.
 When angioedema of the lips, tongue, pharynx, and larynx is the predominant finding and pruritic urticaria is absent, consider angiotensin-converting enzyme (ACE) inhibitors (e.g., Capoten, Vasotec, Lotensin, Prinivil, Zestril) as the precipitating cause. For a patient who is not taking ACE inhibitors, consider hereditary angioedema (see Chapter 60).
When angioedema of the lips, tongue, pharynx, and larynx is the predominant finding and pruritic urticaria is absent, consider angiotensin-converting enzyme (ACE) inhibitors (e.g., Capoten, Vasotec, Lotensin, Prinivil, Zestril) as the precipitating cause. For a patient who is not taking ACE inhibitors, consider hereditary angioedema (see Chapter 60).
 If the urticarial lesions are tender and accompanied by fever or arthralgias, consider an underlying infection or illness (e.g., collagen vascular disease with vasculitis, viral infections of children and adolescents, anicteric hepatitis, cytomegalovirus, or infectious mononucleosis).
If the urticarial lesions are tender and accompanied by fever or arthralgias, consider an underlying infection or illness (e.g., collagen vascular disease with vasculitis, viral infections of children and adolescents, anicteric hepatitis, cytomegalovirus, or infectious mononucleosis).
What Not To Do:
 Do not perform a comprehensive medical and laboratory investigation in simple straightforward cases of acute urticaria. These studies are expensive and unnecessary. Even with chronic idiopathic urticaria, the evaluation should generally be limited to a complete blood count (CBC), erythrocyte sedimentation rate (ESR), thyroid testing, and liver function tests.
Do not perform a comprehensive medical and laboratory investigation in simple straightforward cases of acute urticaria. These studies are expensive and unnecessary. Even with chronic idiopathic urticaria, the evaluation should generally be limited to a complete blood count (CBC), erythrocyte sedimentation rate (ESR), thyroid testing, and liver function tests.
 Do not let the patient take aspirin or consume excessive alcohol. Some patients experience precipitation or worsening of their symptoms with the use of aspirin, other nonsteroidal anti-inflammatory drugs (NSAIDs), or alcohol. Morphine and codeine as well as certain food additives, such as azo food dyes, tartrazine dye, and benzoates, are often allergens or potentiate allergic reactions and should probably also be avoided.
Do not let the patient take aspirin or consume excessive alcohol. Some patients experience precipitation or worsening of their symptoms with the use of aspirin, other nonsteroidal anti-inflammatory drugs (NSAIDs), or alcohol. Morphine and codeine as well as certain food additives, such as azo food dyes, tartrazine dye, and benzoates, are often allergens or potentiate allergic reactions and should probably also be avoided.
 Do not recommend or prescribe topical steroids, topical antihistamines, or topical anesthetic creams or sprays. They are ineffective and have no role in the management of urticaria.
Do not recommend or prescribe topical steroids, topical antihistamines, or topical anesthetic creams or sprays. They are ineffective and have no role in the management of urticaria.
 Do not overlook the possibility of an urticarial vasculitis when the presenting rash is more painful than itchy and there are systemic symptoms, such as purpura, arthralgias, fever, abdominal pain, and nephritis. Obtain an ESR, consider the diagnosis of systemic lupus erythematosus or Sjögren syndrome, and consult specialists appropriately.
Do not overlook the possibility of an urticarial vasculitis when the presenting rash is more painful than itchy and there are systemic symptoms, such as purpura, arthralgias, fever, abdominal pain, and nephritis. Obtain an ESR, consider the diagnosis of systemic lupus erythematosus or Sjögren syndrome, and consult specialists appropriately.
 Do not restrict the use of iodinated contrast media for patients with a history of seafood allergy. There is no evidence that seafood allergy is a specific contraindication to use of ionic contrast. Most events occur randomly.
Do not restrict the use of iodinated contrast media for patients with a history of seafood allergy. There is no evidence that seafood allergy is a specific contraindication to use of ionic contrast. Most events occur randomly.
Discussion
Urticaria, also referred to as hives or wheals, is a common and distinctive skin reaction pattern that may occur at any age.
Urticaria present for less than 6 weeks is classified as acute, greater than 6 weeks is considered chronic. Simple urticaria affects approximately 20% of the population at some time. Most cases are acute. This local is the result, at least in part, to the release of histamines and other vasoactive peptides from mast cells following an IgE-mediated antigen-antibody reaction. This results in vasodilatation and increased vascular permeability, with the leaking of protein and fluid into extravascular spaces. The heavier concentration of mast cells within the lips, face, and hands explains why these areas are more commonly affected. The edema of urticaria is found in the superficial dermis. The edema in angioedema is found in the deep dermis or subcutaneous/submucosal tissues. Angioedema is more common in children and young adults. Chronic urticaria is more common in middle-aged women. Acute urticaria is often allergic in origin; in the event that a particular cause can be identified, symptoms resolve rapidly after avoidance and do not recur without further exposure. The ideal treatment for allergic urticaria is identification and elimination of its cause. Because the cause is often obscure, however, only symptomatic treatment may be possible. The spontaneous resolution of symptoms obviates the need for an extensive evaluation.
It is well established that food allergies are common causes of acute urticaria. Although virtually any food can act as a food allergen, it is remarkable that most type I (IgE-mediated) food allergies are caused by a rather limited number of food categories. Specifically, milk (dairy), egg, wheat, legumes (including peanut, soybean, and pea), tree nuts, and seafood (fish, crustacean, and mollusk) account for more than 95% of all food allergies. It is also common for acute symptoms to have no obvious cause and spontaneously resolve over the course of a few weeks.
Chronic urticaria and angioedema, on the other hand, usually remain symptomatic for months to years, with periodic remissions and relapses. Although they look like an allergic reaction, they are rarely the result of an allergic process and instead are considered to be caused by an autoimmune or idiopathic mechanism. A significant proportion of chronic urticaria is triggered through particular physical stimuli. Most common among these is dermatographism, in which mast cell degranulation is caused by minor skin trauma (e.g., simple scratching). Cold-induced urticaria is another relatively common form of chronic physical urticaria.
Urticarial vasculitis should be considered if a single urticarial lesion (rather than being short-lived) lasts longer than 24 to 36 hours, if lesions are burning or painful, if they are more common in the lower extremities, or if they leave an area of hemosiderin pigment after they have resolved. Infection, drug sensitivity, serum sickness, chronic hepatitis, and systemic lupus erythematosus may cause urticarial vasculitis. These patients should be referred to a dermatologist for punch biopsy, further evaluation, and management.
The overall incidence of ACE inhibitor–induced angioedema is reported to be approximately 0.1% to 0.2% and is five times more common among black than among white patients. Although angioedema most typically occurs during the first week of therapy, some patients may have taken the ACE inhibitor without any problem for weeks or months before angioedema develops. Because of this, ACE inhibitors are often overlooked as a cause of angioedema, and this may lead to the unfortunate continuation of the edema-producing drug, along with more severe attacks. A clue to the underlying cause is angioedema without urticaria. Because of the risk for relapse and airway compromise and the slow response to standard therapy, some authors recommend that all of these patients should be admitted to a hospital for overnight observation. However, others believe that if patients experience significant improvement and are comfortable after treatment, it is reasonable to consider them for discharge. Symptoms tend to resolve within 24 to 48 hours of cessation of the ACE inhibitor, although the course may be more variable. The use of fresh frozen plasma to replenish ACE stores has been used for the treatment of life-threatening angioedema, especially when it is resistant to other treatments. Also, an airway specialist should be consulted as soon as possible before trouble develops. In general, angiotensin II receptor antagonists are tolerated by patients who have reacted to ACE inhibitors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


