CHAPTER 84
Urinary Retention, Acute
Presentation
The patient, usually male, may complain of increasing dull, low-abdominal discomfort or pain and the urge to urinate, without having been able to urinate for many hours. Urinary hesitancy, sensation of incomplete voiding, an interrupted or decreased urinary stream, and straining to void are other typical symptoms of obstruction. Flank pain may accompany obstruction that leads to hydroureter and hydronephrosis.
Elderly and debilitated patients may be asymptomatic or have vague discomfort with urinary frequency but small volumes, overflow, or stress incontinence.
A firm, distended bladder can be palpated between the symphysis pubis and umbilicus. Rectal examination may reveal an enlarged or tender prostate or suspected tumor, although a prostate that is of normal size and consistency by palpation can still be the cause of urethral obstruction.
What To Do:
 In a male patient, distend the urethra with lidocaine jelly 2% in a catheter-tipped syringe (Uroject, Uro-Jet) and try a 16-, 18-, or 20-Fr Foley catheter. When there is minimal distress, leave the lidocaine jelly in place 15 to 20 minutes to obtain good mucosal anesthesia before inserting the catheter (Figure 84-1).
In a male patient, distend the urethra with lidocaine jelly 2% in a catheter-tipped syringe (Uroject, Uro-Jet) and try a 16-, 18-, or 20-Fr Foley catheter. When there is minimal distress, leave the lidocaine jelly in place 15 to 20 minutes to obtain good mucosal anesthesia before inserting the catheter (Figure 84-1).
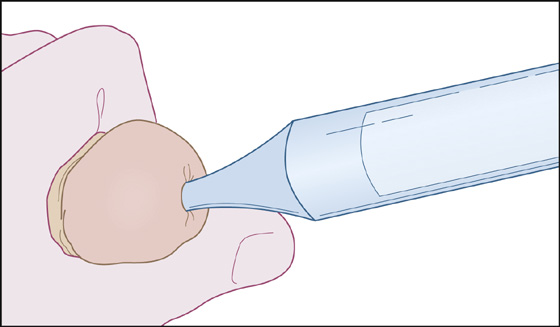
Figure 84-1 Lidocaine jelly administrator.
 When the patient is very uncomfortable, delay only long enough to provide good aseptic technique, pass a Foley catheter into the bladder, and collect the urine in a closed collecting system bag. Reassuring the patient and having him breathe through his mouth may help relax the external sphincter of the bladder and facilitate the passage of the catheter.
When the patient is very uncomfortable, delay only long enough to provide good aseptic technique, pass a Foley catheter into the bladder, and collect the urine in a closed collecting system bag. Reassuring the patient and having him breathe through his mouth may help relax the external sphincter of the bladder and facilitate the passage of the catheter.
 If the problem is negotiating the curve around a large prostate, use a Coudé catheter.
If the problem is negotiating the curve around a large prostate, use a Coudé catheter.
 If the bladder still cannot drain, obtain urologic consultation for instrumentation with stylets, sounds, filiforms, and followers, or consider a percutaneous suprapubic catheterization (but only after it is confirmed that the bladder is distended).
If the bladder still cannot drain, obtain urologic consultation for instrumentation with stylets, sounds, filiforms, and followers, or consider a percutaneous suprapubic catheterization (but only after it is confirmed that the bladder is distended).
 Check renal and urinary function with urinalysis, a urine culture, and serum blood urea nitrogen (BUN) and creatinine determinations.
Check renal and urinary function with urinalysis, a urine culture, and serum blood urea nitrogen (BUN) and creatinine determinations.
 Examine the patient to ascertain the cause of the obstruction. Urinalysis may show hematuria, crystalluria, and/or an elevated pH (>7.5), suggesting the presence of renal calculi. The presence of pyuria, bacteriuria, elevated pH, and/or nitrites suggests infection.
Examine the patient to ascertain the cause of the obstruction. Urinalysis may show hematuria, crystalluria, and/or an elevated pH (>7.5), suggesting the presence of renal calculi. The presence of pyuria, bacteriuria, elevated pH, and/or nitrites suggests infection.
 Ultrasonography is useful in determining whether proximal distention is present in the urinary tract. It can also confirm suspected bladder distention, although this can usually be determined clinically from the physical examination, followed by measurement of the urine flow when a bladder catheter is placed.
Ultrasonography is useful in determining whether proximal distention is present in the urinary tract. It can also confirm suspected bladder distention, although this can usually be determined clinically from the physical examination, followed by measurement of the urine flow when a bladder catheter is placed.
 If there is an infection of the bladder, give antibiotics (see Chapter 85).
If there is an infection of the bladder, give antibiotics (see Chapter 85).
 If the volume drained is modest (0.5 to 1.5 L) and the patient is stable and ambulatory, attach the Foley catheter to a leg bag and discharge the patient for urologic follow-up (and probably catheter removal) the next day.
If the volume drained is modest (0.5 to 1.5 L) and the patient is stable and ambulatory, attach the Foley catheter to a leg bag and discharge the patient for urologic follow-up (and probably catheter removal) the next day.
 If the volume drained is small (100 to 200 mL), remove the catheter and search for alternate causes of the abdominal mass and urinary urgency.
If the volume drained is small (100 to 200 mL), remove the catheter and search for alternate causes of the abdominal mass and urinary urgency.
 When prostatic enlargement (which is a common cause of bladder outlet obstruction in older men) is suspected, alpha-blocker agents may be helpful, especially in those patients who want to be sent home with a trial without an indwelling urinary catheter. Prescribe alfuzosin (Uroxatral), 10 mg qd taken with food; doxazosin (Cardura XL), 4 mg qd at breakfast; or tamsulosin (Flomax), 0.4 mg qd 30 minutes after eating. These drugs can cause symptomatic hypotension, particularly in patients with ventricular hypertrophy. Giving the first dose at bedtime may help avoid syncope.
When prostatic enlargement (which is a common cause of bladder outlet obstruction in older men) is suspected, alpha-blocker agents may be helpful, especially in those patients who want to be sent home with a trial without an indwelling urinary catheter. Prescribe alfuzosin (Uroxatral), 10 mg qd taken with food; doxazosin (Cardura XL), 4 mg qd at breakfast; or tamsulosin (Flomax), 0.4 mg qd 30 minutes after eating. These drugs can cause symptomatic hypotension, particularly in patients with ventricular hypertrophy. Giving the first dose at bedtime may help avoid syncope.
 Warn the patient to return if obstructive symptoms recur, and provide early urologic follow-up, ideally within the next 24 to 48 hours.
Warn the patient to return if obstructive symptoms recur, and provide early urologic follow-up, ideally within the next 24 to 48 hours.
What Not To Do:
 Do not use stylets or sounds unless you have experience instrumenting the urethra; these devices can cause considerable trauma.
Do not use stylets or sounds unless you have experience instrumenting the urethra; these devices can cause considerable trauma.
 Do not remove the catheter right away if the bladder was significantly distended. Bladder tone will take several hours to return, and the bladder may become distended again.
Do not remove the catheter right away if the bladder was significantly distended. Bladder tone will take several hours to return, and the bladder may become distended again.
 Do not clamp the catheter to slow decompression of the bladder, even if the volume drained is more than 2 L.
Do not clamp the catheter to slow decompression of the bladder, even if the volume drained is more than 2 L.
 Do not use bethanechol (Urecholine) unless it is clear that there is no obstruction, inadequate (parasympathetic) bladder tone is the only cause of the distention, and there is no possibility of gastrointestinal disease.
Do not use bethanechol (Urecholine) unless it is clear that there is no obstruction, inadequate (parasympathetic) bladder tone is the only cause of the distention, and there is no possibility of gastrointestinal disease.
 Do not perform an intravenous pyelogram in patients with compromised renal function. This can cause further renal compromise because of nephrotoxicity.
Do not perform an intravenous pyelogram in patients with compromised renal function. This can cause further renal compromise because of nephrotoxicity.
 Do not routinely prescribe prophylactic antibiotics. They lower the incidence of bacteriuria at the expense of selecting out more virulent organisms. Unless the patient is at high risk for the complications of catheter-associated bacteriuria (i.e., renal transplant and granulopenic patients), antibiotic prophylaxis for short-term catheterization is not warranted. A small percentage of low-risk patients with bacteriuria will progress to symptomatic urinary tract infection. However, most will clear spontaneously.
Do not routinely prescribe prophylactic antibiotics. They lower the incidence of bacteriuria at the expense of selecting out more virulent organisms. Unless the patient is at high risk for the complications of catheter-associated bacteriuria (i.e., renal transplant and granulopenic patients), antibiotic prophylaxis for short-term catheterization is not warranted. A small percentage of low-risk patients with bacteriuria will progress to symptomatic urinary tract infection. However, most will clear spontaneously.
Discussion
Urinary retention is characterized by a urine residual greater than 200 mL after attempted voiding.
Urinary retention may be caused by stones lodged in the urethra or urethral strictures (often from gonorrhea); foreign bodies, including blocked urinary catheters; prostatitis, prostatic carcinoma, or benign prostatic hypertrophy; blood clot, following urologic procedures; and tumor in the bladder.
Any drug with anticholinergic effects or α-adrenergic effects, such as antihistamines, ephedrine sulfate, and phenylpropanolamine, can precipitate urinary retention. Morphine and other narcotics inhibit the voiding reflex and increase the muscle tone of the external sphincter, both of which can contribute to urinary retention. Other drugs that can cause urinary retention are tricyclic antidepressants, detrusor relaxants (e.g., oxybutynin [Ditropan]), and calcium channel blockers.
Neurologic causes include cord lesions, diabetic neuropathy, Parkinson disease, stroke, malignancy that compresses the spinal cord, and multiple sclerosis. Patients with genital herpes or herpes zoster may develop urinary retention from nerve involvement.
Urinary retention has also been reported following vigorous anal intercourse. In addition, anything that causes compression from outside the urinary tract can cause obstruction. Abdominal aneurysms, tumors (primary or metastatic, benign or malignant), pregnancy, ovarian abscess, intra-abdominal abscess (e.g., ruptured appendiceal abscess), and large fecal impactions are some examples of extrinsic lesions that can cause obstruction. The urethral catheterization outlined is the appropriate initial treatment for all these conditions.
Sometimes hematuria develops midway through bladder decompression, probably representing loss of tamponade of vessels that were injured as the bladder distended. This should be watched until the bleeding stops (usually spontaneously) to be sure that there is no great blood loss, no other urologic disease responsible, and no clot obstruction.
Postobstructive diuresis is common, possibly because of increased synthesis of renal prostaglandins. In severe cases, this can lead to electrolyte imbalances and even dehydration. In these severe cases, fluid and electrolyte replacement may be indicated but should be undertaken carefully, because inappropriate replacement can prolong the diuresis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


