4 Upper Extremities ! +++ R2–3 times a week, up to 12 weeks PhysApps, FMA, ThE, Acu, Chiro, ESWL ! +++ R 2 times a week, up to 4 weeks PhysApps, FMA, Acu ! +++ R 2 times a week, up to 12 weeks Chiro, PhysApps, FMA, ThE, Orthotech, ESWL !++ R 2 times a week, up to 4 weeks FMA, PhysApps, Acu, Med !++ R2–3 times a week, up to 4 weeks PhysApps, TENS, ThE, MET
 Complex Pain
Complex Pain
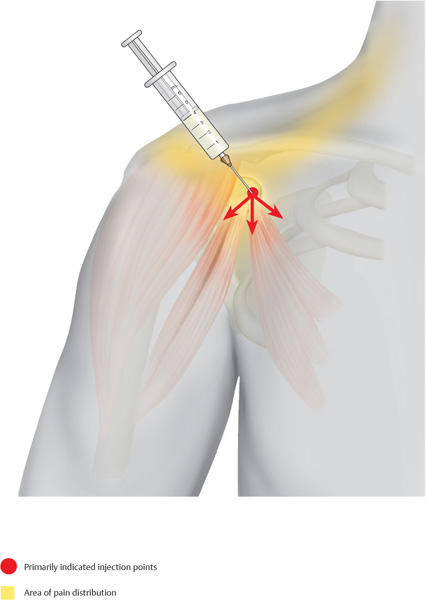
Anterior Shoulder and Subacromial Pain
Indications
 Shoulder–arm pain
Shoulder–arm pain
 Humeroscapular periarthritis
Humeroscapular periarthritis
 Degenerative changes in the rotator cuff
Degenerative changes in the rotator cuff
 Omarthrosis
Omarthrosis
 Musculotendinous overload
Musculotendinous overload
 Frozen shoulder
Frozen shoulder
 Referred pain symptoms arising from cardiac disorders
Referred pain symptoms arising from cardiac disorders
Material
 Local anesthetic: 5–7mL
Local anesthetic: 5–7mL
 Needle: 0.6 × 60 mm
Needle: 0.6 × 60 mm
Technique
 The acromioclavicular joint is located through palpation while the arm is placed in slight internal rotation. From there, the insertion site is barely 1.5 cm inferolaterally. The tip of the needle points transversely from anterolateral in the posteromedial direction. The needle is advanced 2.5–3 cm until bone contact is made. The local anesthetic is administered successively while the needle is being retracted.
The acromioclavicular joint is located through palpation while the arm is placed in slight internal rotation. From there, the insertion site is barely 1.5 cm inferolaterally. The tip of the needle points transversely from anterolateral in the posteromedial direction. The needle is advanced 2.5–3 cm until bone contact is made. The local anesthetic is administered successively while the needle is being retracted.
 Now, 3–4 cm medially at the same level, the usually painful coracoid process is located. The needle is advanced until bone contact is made. Then, the needle is slightly retracted and advanced again inferiorly for 1 cm. Following aspiration, the local anesthetic is injected.
Now, 3–4 cm medially at the same level, the usually painful coracoid process is located. The needle is advanced until bone contact is made. Then, the needle is slightly retracted and advanced again inferiorly for 1 cm. Following aspiration, the local anesthetic is injected.
 The injection slightly inferolateral to the acromioclavicular joint completes the therapeutic triangle. The needle first makes bone contact, is slightly retracted, and 0.5 mL of a local anesthetic is injected.
The injection slightly inferolateral to the acromioclavicular joint completes the therapeutic triangle. The needle first makes bone contact, is slightly retracted, and 0.5 mL of a local anesthetic is injected.
 Additionally, the insertion of the ligament at the superior edge of the coracoid process can be flooded with the injectable. If pain radiates into the upper arm, the deltoid insertion should receive an injection of a local anesthetic as well. On the anterolateral aspect of the upper arm, the deltoid attachment is located in a slight depression. From a mediolateral direction, the needle is advanced until bone contact is made and the injectable is administered in a fan-shaped pattern around the muscle attachment at the deltoid tuberosity of the humerus.
Additionally, the insertion of the ligament at the superior edge of the coracoid process can be flooded with the injectable. If pain radiates into the upper arm, the deltoid insertion should receive an injection of a local anesthetic as well. On the anterolateral aspect of the upper arm, the deltoid attachment is located in a slight depression. From a mediolateral direction, the needle is advanced until bone contact is made and the injectable is administered in a fan-shaped pattern around the muscle attachment at the deltoid tuberosity of the humerus.
Risks
 Injury to the cephalic vein. Aspiration!
Injury to the cephalic vein. Aspiration!
 Unintentional conduction anesthesia of the radial nerve with temporary wrist drop. In the case of galvanic, flashlike sensations during insertion, the needle must be placed more precisely.
Unintentional conduction anesthesia of the radial nerve with temporary wrist drop. In the case of galvanic, flashlike sensations during insertion, the needle must be placed more precisely.
 The patient must be informed about the temporary characteristics of anesthesia if numbness or paresthesia is noticed immediately after the injection. Until the regular sensation in the hand is restored, patients should refrain from driving a vehicle.
The patient must be informed about the temporary characteristics of anesthesia if numbness or paresthesia is noticed immediately after the injection. Until the regular sensation in the hand is restored, patients should refrain from driving a vehicle.
Concomitant Therapies
 In the case of predominantly inflammatory changes, local cryotherapy is indicated.
In the case of predominantly inflammatory changes, local cryotherapy is indicated.
 Transverse friction massage at the muscle–tendon junction
Transverse friction massage at the muscle–tendon junction
 Temporary abducted positioning of the arm
Temporary abducted positioning of the arm
 Phonophoresis
Phonophoresis
 Stabilization of the shoulder girdle by building up muscle through physical therapy
Stabilization of the shoulder girdle by building up muscle through physical therapy
 Acupuncture, including needling of the periost
Acupuncture, including needling of the periost
 In the case of frozen shoulder, intra-articular saline injection to rupture the capsule, involving manual mobilization and co-treatment of the irritated suprascapular nerve
In the case of frozen shoulder, intra-articular saline injection to rupture the capsule, involving manual mobilization and co-treatment of the irritated suprascapular nerve
 In the case of segmental cervical spine dysfunctions, complementing chiropractic treatments
In the case of segmental cervical spine dysfunctions, complementing chiropractic treatments
 In the case of calcified humeroscapular peri-arthritis, extracorporeal shockwave lithotripsy
In the case of calcified humeroscapular peri-arthritis, extracorporeal shockwave lithotripsy
Pain in the Area of the Coracoid Process
Indications
 Insertion tendinosis of the pectoralis minor and the coracobrachialis
Insertion tendinosis of the pectoralis minor and the coracobrachialis
 Projected pain symptoms to the left of the stomach and the heart
Projected pain symptoms to the left of the stomach and the heart
 Right-sided reflex zones of the ascending colon and the liver area
Right-sided reflex zones of the ascending colon and the liver area
Differential Diagnoses
 Affections of the acromioclavicular joint in terms of arthrosis and blockages
Affections of the acromioclavicular joint in terms of arthrosis and blockages
 Inflammatory changes of the subacromial bursa
Inflammatory changes of the subacromial bursa
 Scalene compartment syndrome
Scalene compartment syndrome
Material
 Local anesthetic: 3 mL
Local anesthetic: 3 mL
 Needle: 0.6 × 30 mm
Needle: 0.6 × 30 mm
Technique
 A rough, pressure-sensitive protuberance is located approximately 1–2 cm below the lateral third of the clavicle. This is the fascia-covered coracoid process. The needle is inserted 2–3cm at the inferior edge of the palpable protuberance.
A rough, pressure-sensitive protuberance is located approximately 1–2 cm below the lateral third of the clavicle. This is the fascia-covered coracoid process. The needle is inserted 2–3cm at the inferior edge of the palpable protuberance.
 The needle is inserted vertically and the injectable is administered in a fan-shaped pattern. It is important to also inject the local anesthetic into the periost of the coracoid process, because the origin site of the short head of the biceps brachii can cause periosteal irritation.
The needle is inserted vertically and the injectable is administered in a fan-shaped pattern. It is important to also inject the local anesthetic into the periost of the coracoid process, because the origin site of the short head of the biceps brachii can cause periosteal irritation.
Risks
 The cephalic vein can be injured if the needle is inserted too far medially.
The cephalic vein can be injured if the needle is inserted too far medially.
 Aspiration prior to injection can avoid the risk of injecting the local anesthetic into the parallel-running deltoid artery.
Aspiration prior to injection can avoid the risk of injecting the local anesthetic into the parallel-running deltoid artery.
Concomitant Therapies
 Treatment with ultrasound in the area of tendon insertions, as well as transverse friction massage
Treatment with ultrasound in the area of tendon insertions, as well as transverse friction massage
 Iontophoresis
Iontophoresis
 Acupuncture (LI-15, LU-2, SP-9)
Acupuncture (LI-15, LU-2, SP-9)
Lateral Epicondylitis (Tennis Elbow)
Indications
 Lateral epicondylitis
Lateral epicondylitis
 Disorders of the radioulnar joint
Disorders of the radioulnar joint
 Irritation of the anular ligament of the radius
Irritation of the anular ligament of the radius
 Myogelosis and insertion tendinosis of the anconeus
Myogelosis and insertion tendinosis of the anconeus
Differential Diagnoses
 Shoulder–arm pain due to cervical spine disorders of the C 4 segment
Shoulder–arm pain due to cervical spine disorders of the C 4 segment
 Nerve compartment syndrome (supinator syndrome)
Nerve compartment syndrome (supinator syndrome)
 Herniated disk in the C 4/C 5 segment
Herniated disk in the C 4/C 5 segment
 Free joint bodies
Free joint bodies
 Osteonecrosis (Hegemann disease, Iselin disease)
Osteonecrosis (Hegemann disease, Iselin disease)
 Osteochondritis dissecans of the humeral condyle
Osteochondritis dissecans of the humeral condyle
Material
 Local anesthetic: 2 mL
Local anesthetic: 2 mL
 Needle: 0.4 × 20 mm
Needle: 0.4 × 20 mm
Technique
 The easily palpable bony protuberance of the condyle of humerus is located. It is generally very pain sensitive.
The easily palpable bony protuberance of the condyle of humerus is located. It is generally very pain sensitive.
 Approximately 2 cm distally, the needle is inserted from posterior in the direction of the elbow crease. With use of a fan-shaped pattern, the muscular attachment site is completely flooded with the injectable, particularly the parts close to the bone.
Approximately 2 cm distally, the needle is inserted from posterior in the direction of the elbow crease. With use of a fan-shaped pattern, the muscular attachment site is completely flooded with the injectable, particularly the parts close to the bone.
Risks
 If the needle is placed imprecisely and advanced excessively, the radial nerve may be anesthetized. Temporary numbness will result in the area supplied by this nerve, especially on the radial and posterior aspect. Temporary partial paralysis may occur as well.
If the needle is placed imprecisely and advanced excessively, the radial nerve may be anesthetized. Temporary numbness will result in the area supplied by this nerve, especially on the radial and posterior aspect. Temporary partial paralysis may occur as well.
 If the periost is penetrated and injection takes place in this area, an extremely painful local anesthetic deposit will result between the bone and the periost, which may intensify the initial pain.
If the periost is penetrated and injection takes place in this area, an extremely painful local anesthetic deposit will result between the bone and the periost, which may intensify the initial pain.
Concomitant Therapies
 Functional disorders of the cervical spine segment C 4/C 5 should bilaterally be ruled out. Beyond that, sensorimotor dysfunctions do not occur. Especially if fingers become numb at night, an affection of the median nerve must be considered.
Functional disorders of the cervical spine segment C 4/C 5 should bilaterally be ruled out. Beyond that, sensorimotor dysfunctions do not occur. Especially if fingers become numb at night, an affection of the median nerve must be considered.
 In the case of limited mobility and movement disorders in the radioulnar joint, the joint should be treated with manual therapy. If characteristic symptoms of periosteal irritation are present, the patient should apply local cryotherapy, for example, massaging the area with ice cubes. In addition, ultrasound and transverse friction according to Cyriax are recommended.
In the case of limited mobility and movement disorders in the radioulnar joint, the joint should be treated with manual therapy. If characteristic symptoms of periosteal irritation are present, the patient should apply local cryotherapy, for example, massaging the area with ice cubes. In addition, ultrasound and transverse friction according to Cyriax are recommended.
 Overload relating to work or athletic activities responds well to stretching techniques and additional subcircular taping or supportive bandaging. It is important to gather relevant information about work and athletic activities in the case history. Extracorporeal shockwave treatment is recommended in chronically recurrent cases.
Overload relating to work or athletic activities responds well to stretching techniques and additional subcircular taping or supportive bandaging. It is important to gather relevant information about work and athletic activities in the case history. Extracorporeal shockwave treatment is recommended in chronically recurrent cases.
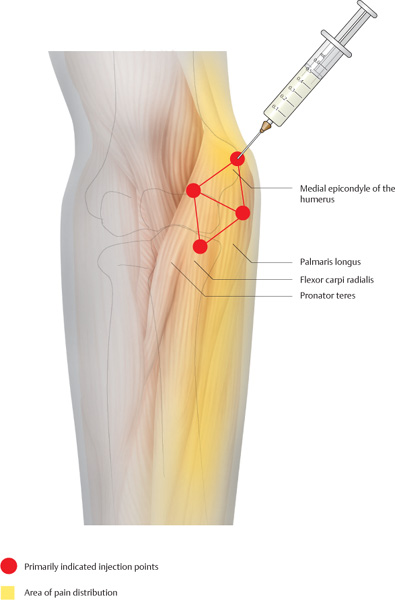
Medial Epicondylitis (Golfer’s Elbow)
Indications
 Medial epicondylitis
Medial epicondylitis
 Pronator teres syndrome
Pronator teres syndrome
 Arthrosis of the elbow joint
Arthrosis of the elbow joint
 Periostosis with affection of the ulnar collateral ligament
Periostosis with affection of the ulnar collateral ligament
Differential Diagnoses
 Radicular symptoms of the inferior cervical spine C 7/C 8
Radicular symptoms of the inferior cervical spine C 7/C 8
 Cubital tunnel syndrome
Cubital tunnel syndrome
 Free joint bodies
Free joint bodies
Material
 Local anesthetic: 2 mL
Local anesthetic: 2 mL
 Needle: 0.4 × 20 mm
Needle: 0.4 × 20 mm
Technique
 The “two-wall technique” produces the best results. The first injection site is located directly above the most protruding point of the ulnahumeral epicondyle. The needle is advanced up to the periost, retracted 1 mm, and 0.5 mL of a local anesthetic is injected.
The “two-wall technique” produces the best results. The first injection site is located directly above the most protruding point of the ulnahumeral epicondyle. The needle is advanced up to the periost, retracted 1 mm, and 0.5 mL of a local anesthetic is injected.
 The other points are arranged in the shape of an isosceles triangle, 2 cm distal, deviating slightly in the medial and posterior direction. The fourth point completes an isosceles trapezium and is located a further 2 cm distally on a straight line that comes from the first point and divides the distance between the second and third points in half. The points are located above the pronator teres, flexor carpi radialis, and palmaris longus. The needle is inserted vertically and advanced 1 cm. Each site receives 0.5 mL of a local anesthetic.
The other points are arranged in the shape of an isosceles triangle, 2 cm distal, deviating slightly in the medial and posterior direction. The fourth point completes an isosceles trapezium and is located a further 2 cm distally on a straight line that comes from the first point and divides the distance between the second and third points in half. The points are located above the pronator teres, flexor carpi radialis, and palmaris longus. The needle is inserted vertically and advanced 1 cm. Each site receives 0.5 mL of a local anesthetic.
Risks
 If the injection takes place posterior to the ulnar epicondyle, the ulnar nerve is anesthetized.
If the injection takes place posterior to the ulnar epicondyle, the ulnar nerve is anesthetized.
 If the needle is inserted too far proximally at the medial injection site, the injectable may be administered into the ulnar artery.
If the needle is inserted too far proximally at the medial injection site, the injectable may be administered into the ulnar artery.
 At the distal injection sites, unintentional injections into the basilic vein may occur; therefore, aspiration prior to injection is required.
At the distal injection sites, unintentional injections into the basilic vein may occur; therefore, aspiration prior to injection is required.
Concomitant Therapies
 Transverse friction massage according to Cyriax, local cryotherapy, and transcutaneous application of anti-inflammatories
Transverse friction massage according to Cyriax, local cryotherapy, and transcutaneous application of anti-inflammatories
 Changes in workload and athletic activities, if applicable
Changes in workload and athletic activities, if applicable
 Phonophoresis
Phonophoresis
 Acupuncture along the heart and large intestine channels (HT-3, LI-11)
Acupuncture along the heart and large intestine channels (HT-3, LI-11)
 Therapy through Muscles, Tendons, and Ligaments
Therapy through Muscles, Tendons, and Ligaments
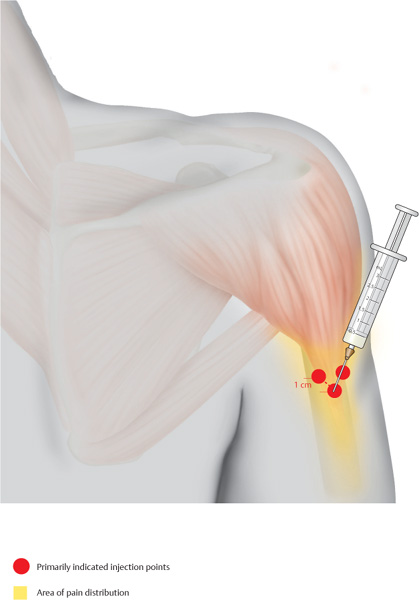
Deltoid
Indications
 Characteristic pain projected in the attachment area of the deltoid, which is located at the deltoid tuberosity on the lateral aspect of the upper arm
Characteristic pain projected in the attachment area of the deltoid, which is located at the deltoid tuberosity on the lateral aspect of the upper arm
 Adjuvant treatment for rotator cuff injuries
Adjuvant treatment for rotator cuff injuries
Differential Diagnoses
 Affections of the teres minor
Affections of the teres minor
 Pain projections in the case of pulmonary affections
Pain projections in the case of pulmonary affections
 Vascular compartment syndromes, especially scalenus compartment syndromes
Vascular compartment syndromes, especially scalenus compartment syndromes
Material
 Local anesthetic: 3–5mL
Local anesthetic: 3–5mL
 Needle: 0.6 × 60 mm
Needle: 0.6 × 60 mm
Technique
 The main infiltration sites are located in the area of the deltoid insertion at the lateral aspect of the upper arm. The distinct sensitivity to pressure can be found in this tapering muscle part. The needle is inserted vertically until bone contact is made. The injection includes the periost. The second insertion takes place 1 cm superomedially to the first site. The needle is advanced again until bone contact is made. The third insertion takes place in the same manner, 1.5 cm posterosuperiorly. Each site receives 0.5–1mL of a local anesthetic.
The main infiltration sites are located in the area of the deltoid insertion at the lateral aspect of the upper arm. The distinct sensitivity to pressure can be found in this tapering muscle part. The needle is inserted vertically until bone contact is made. The injection includes the periost. The second insertion takes place 1 cm superomedially to the first site. The needle is advanced again until bone contact is made. The third insertion takes place in the same manner, 1.5 cm posterosuperiorly. Each site receives 0.5–1mL of a local anesthetic.
 Additional injection sites include painful points along the entire deltoid. They can usually be identified as indurated areas within the muscle. With use of the two-finger technique, the distinct pain area receives 0.5 mL of a local anesthetic, 1.5–2 cm deep.
Additional injection sites include painful points along the entire deltoid. They can usually be identified as indurated areas within the muscle. With use of the two-finger technique, the distinct pain area receives 0.5 mL of a local anesthetic, 1.5–2 cm deep.
Risks
 Along the anterior border of the deltoid, one may unintentionally inject the local anesthetic into the cephalic vein; therefore, aspiration is necessary prior to injection.
Along the anterior border of the deltoid, one may unintentionally inject the local anesthetic into the cephalic vein; therefore, aspiration is necessary prior to injection.
 On the posterior border of the muscle, the local anesthetic may be unintentionally injected into the superior lateral brachial cutaneous nerve of the axillary nerve, which causes temporary numbness in the posterior and lateral aspect of the deltoid. The patient must therefore be informed about possible changes in sensitivity.
On the posterior border of the muscle, the local anesthetic may be unintentionally injected into the superior lateral brachial cutaneous nerve of the axillary nerve, which causes temporary numbness in the posterior and lateral aspect of the deltoid. The patient must therefore be informed about possible changes in sensitivity.
Concomitant Therapies
 Local cryotherapy at the deltoid attachment
Local cryotherapy at the deltoid attachment
 Ultrasound in the form of phonophoresis
Ultrasound in the form of phonophoresis
 Transcutaneous electrical nerve stimulation above the painful areas
Transcutaneous electrical nerve stimulation above the painful areas
 Depending on the stage, physical therapy in the case of rotator cuff injuries
Depending on the stage, physical therapy in the case of rotator cuff injuries
 Medical exercise therapy
Medical exercise therapy
Rhomboid
Indications
 Pain along the superior thoracic spine
Pain along the superior thoracic spine
 Pain along the medial edge of the shoulder blade
Pain along the medial edge of the shoulder blade
Differential Diagnoses
 Left-sided affections of the posterior myocardial wall
Left-sided affections of the posterior myocardial wall
 Affections of the kidneys and the superior urinary tract
Affections of the kidneys and the superior urinary tract
 Costovertebral joint dysfunctions
Costovertebral joint dysfunctions
Material
 Local anesthetic: 0.5 mL
Local anesthetic: 0.5 mL
 Needle: 0.6 × 30 mm
Needle: 0.6 × 30 mm
Technique
 The major and minor rhomboids originate between the first and fifth thoracic vertebra and travel in a transverse-lateral direction to the medial edge of the scapula. The most effective insertion sites are located approximately 2 finger widths medial to the palpable bony edge of the scapula. This is where a distinct, painfully indurated area of the muscle group can be found.
The major and minor rhomboids originate between the first and fifth thoracic vertebra and travel in a transverse-lateral direction to the medial edge of the scapula. The most effective insertion sites are located approximately 2 finger widths medial to the palpable bony edge of the scapula. This is where a distinct, painfully indurated area of the muscle group can be found.
 Beginning at the level of the superior tip of the scapula, needle insertions take place vertically every 3 cm, the needle is advanced 1 cm, and 0.5–1 mL of a local anesthetic is injected.
Beginning at the level of the superior tip of the scapula, needle insertions take place vertically every 3 cm, the needle is advanced 1 cm, and 0.5–1 mL of a local anesthetic is injected.
Risks
 If the needle is advanced excessively, pleura and lungs may be injured; therefore, observe the insertion depth.
If the needle is advanced excessively, pleura and lungs may be injured; therefore, observe the insertion depth.
Concomitant Therapies
 Local, moist heat application
Local, moist heat application
 Mobilization of the scapula and the scapulothoracic gliding plane using manual therapy
Mobilization of the scapula and the scapulothoracic gliding plane using manual therapy
 Patients learn to massage the area themselves, for example, using a tennis ball or a porcupine massage ball.
Patients learn to massage the area themselves, for example, using a tennis ball or a porcupine massage ball.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree