KEY POINTS
Suspected upper airway obstruction (UAO) constitutes a medical emergency. The immediate bedside consultation of a clinician experienced in the management of this condition is indicated.
The initial evaluation of UAO is focused on determining the severity and suspected site of the obstruction. Arterial desaturation is a late manifestation; better indicators of severity include stridor, poor air movement, accessory muscle use, abnormal mentation or agitation, tachycardia, hypertension, and pulsus paradoxus.
Infections represent important causes of oropharyngeal and hypopharyngeal UAO and include Ludwig angina, peritonsillar abscess, and infections of the retropharyngeal and lateral pharyngeal spaces. Otolaryngology consultation is indicated. Depending on the initial site of infection, spread to other critical sites (eg, the mediastinum) may occur.
While intubation is not always required in adults with epiglottitis, management in an ICU is mandatory, and intubation equipment and a tracheostomy tray should be at the bedside.
Bacterial infections of the larynx are life-threatening. Causative organisms include Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, and Corynebacterium diphtheriae.
Laryngospasm and laryngeal edema are important causes of postextubation stridor. Prophylactic corticosteroids may be effective at preventing this phenomenon in high-risk patients. A reasonable approach is to administer methylprednisolone 20 mg IV q4h beginning 12 to 24 hours prior to planned extubation and continued until the tube is removed. Patients with postextubation stridor from laryngeal edema may be treated with a short (eg, 24 hours) course of corticosteroids.
Long-term intubation may result in a variety of problems related to the upper airway, including endotracheal tube obstruction from secretions, vocal cord injury, subglottic stenosis, and tracheal stenosis.
Risk factors for foreign body aspiration in adults include diminished level of consciousness; impaired swallowing mechanism or diminished upper airway sensation as a result of neuromuscular disorder, prior cerebrovascular accident, or advanced age; and inability to chew food properly because of poor dentition.
All suspected traumatic laryngeal injuries should be evaluated promptly to reduce the immediate risk of UAO, as well as to prevent long-term sequelae such as subglottic stenosis.
Early laryngoscopic examination of the upper airway is crucial in the evaluation of burn patients with suspected inhalation injury. The risk of UAO increases throughout the first 24 hours.
Functional upper airway obstruction may occur in patients who exhibit abnormal glottic closure during inspiration and/or expiration. There is a high risk of coincident asthma, complicating the evaluation of such patients.
Angioedema may result from allergy, hereditary or acquired disorders of the complement cascade, direct release of histamine from mast cells from nonallergic mechanisms (eg, opiates), and from angiotensin-converting enzyme inhibitors.
Angioedema from angiotensin-converting enzyme inhibitors may occur at any time during the course of therapy.
Helium-oxygen mixtures reduce the density-dependent pressure required to drive airflow across obstructing upper airway lesions, and may stabilize patients with UAO pending definitive therapy.
Prompt evaluation and management of suspected UAO may prevent subsequent complications including cardiac arrest, anoxic brain injury, and negative pressure pulmonary edema.
There are few medical conditions that are as rapidly and predictably lethal as the loss of upper airway patency. Because of the relative infrequency with which upper airway obstruction (UAO) is encountered by most physicians, opportunities to acquire significant clinical experience are limited. This, combined with the frequently subtle presentation of upper airway obstruction and the clinician’s inability to visualize the upper airway in its entire extent through routine physical examination, may hamper diagnosis of this condition until a crisis results. This chapter describes an approach to diagnosing and treating UAO as it presents in adults. While certain infections of the head, neck, and upper respiratory tract are considered here as they relate to UAO, the specific approach to their management is considered in greater detail in Chap. 73. A high index of suspicion for UAO, combined with early consultation of anesthesia and otolaryngology services, is critical to the successful management of this condition.
ANATOMY OF THE UPPER AIRWAY
The upper airway comprises air-conducting passages that begin at the mouth or nose and end at the mainstem carina.1,2 The thoracic inlet divides the upper airway into the intrathoracic and extrathoracic airways. The extrathoracic airways are further divided into the nasopharynx, oropharynx, hypopharynx, larynx, and extrathoracic trachea. Air inspired through the nose passes through the nasal cavities and enters the nasopharynx after exiting the nose by way of the posterior nares. Airflow proceeds inferiorly through the nasopharynx, passes posterior to the soft palate, and enters the oropharynx. Closure of the soft palate allows inspiration of air through the mouth. Air passes inferiorly through the oropharynx to the hypopharynx, which begins just superior to the hyoid bone, and passes the epiglottis, thereby entering the larynx.
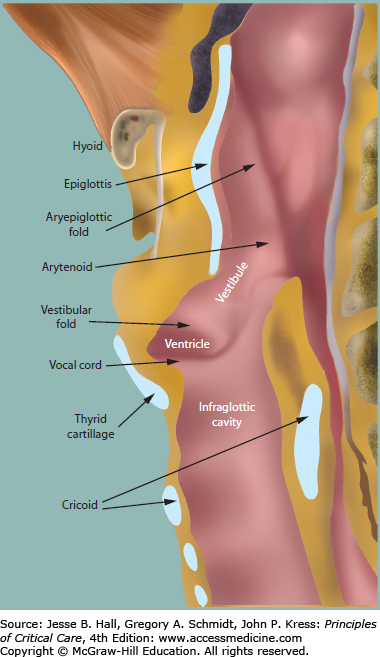
The larynx is constructed of a cartilaginous skeleton consisting of the thyroid, cricoid, and arytenoid cartilages (Fig. 47-1). This skeleton surrounds the vocal cords, the movements of which are controlled by the intrinsic muscles of the larynx, with their innervation arising from the left and right branches of the recurrent laryngeal nerve. An exception to this rule is the innervation of the cricothyroid muscle, which arises from the superior laryngeal nerve. This nerve also supplies sensation to the epiglottis and vestibular folds (false cords), which lie superior to the true vocal cords. The larynx is divided into the supraglottic portion, the glottis, and the subglottic portion. The glottis contains the structures within the plane of the true vocal cords and is located at the midpoint of the thyroid cartilage. The supraglottic region extends from the epiglottis to just above the true vocal cords, while the subglottic region lies between the vocal cords and the lower border of the cricoid cartilage.
The trachea lies between the inferior border of the cricoid cartilage and the main carina, and is 10 to 13 cm in length in adults. The extrathoracic trachea is typically 2 to 4 cm long, and comprises the segment that lies between the cricoid cartilage and the thoracic inlet. The normal trachea has roughly the same coronal as sagittal diameter. Normal coronal tracheal diameter is 13 to 25 mm in men and 10 to 21 mm in women.
This chapter focuses on disorders of the extrathoracic upper airway because of this region’s greater importance to the topic of UAO.
PATHOPHYSIOLOGY OF UPPER AIRWAY OBSTRUCTION
While obstruction may occur at any point in the upper airway, laryngeal obstruction is most problematic because the airway is narrowest at this point. The glottis is the narrowest region in adults, while the subglottic region is the narrowest in infants. The basis for which seemingly minor reductions in the cross-sectional area of the upper airway have important effects on airflow is presented below.
Alveolar ventilation is accomplished through the bulk flow of fresh gas down to the terminal bronchioles, at which point the cross-sectional area of the airways becomes so large that the forward velocity of gas molecules becomes negligible, and diffusive flow occurs.3 Prior to this point airflow may be laminar, transitional, or turbulent. Laminar flow consists of orderly streams of gas arranged in lines parallel to the airway. At higher flow rates and at branch points flow may become transitional, with gas eddies that break away from the parallel streams. Turbulent flow is the most disorganized pattern, and occurs at high flow rates. The Reynolds number (Re) is a dimensionless number that derives from the ratio of inertial to viscous forces and allows prediction of whether flow will be laminar or not:
where r is the radius of the tube, v is the average gas velocity, d is the gas density, and μ is the gas viscosity. Values less than 2000 predict laminar flow, values between 2000 and 4000 predict transitional flow, and values greater than 4000 predict turbulent flow. The driving pressure for laminar flow is proportional to the flow rate and inversely related to the fourth power of the radius, among other factors. Thus a relatively minor decrease in the radius of a tube like the upper airway causes a large increase in the driving pressure necessary to achieve the same flow rate. Turbulent flow as occurs in a rough tube like the larynx and trachea requires greater driving pressure than laminar flow, being proportional to the density of the gas and the square of the flow rate. Inhalation of a low-density gas such as helium therefore decreases the driving pressure required for airflow through two mechanisms: reducing the Reynolds number, thereby increasing the proportion of flow that is laminar; and decreasing the density-dependent driving pressure where turbulent flow exists.4
The clinical implications of these principles are as follows: (1) Upper airway obstructing lesions, once symptomatic, can progress rapidly to a crisis, with relatively small increases in size leading to proportionately greater increases in the work of breathing; (2) the inhalation of a low-density gas mixture such as helium-oxygen decreases the driving pressure required for a given airflow. Helium-oxygen mixtures therefore may act to stabilize the airway in marginally compensated patients, bridging the patient toward definitive treatment of the upper airway obstruction.
Upper airway obstructing lesions may limit inspiratory flow, expiratory flow, or both, depending on the site and nature of the lesion. Flow-volume loops obtained by spirometry are useful for understanding the physiology of different sites of upper airway obstruction.5
During normal inspiration the intrathoracic airways dilate, while the extrathoracic airways tend to collapse as the increase in gas velocity causes a fall in intraluminal pressure (Bernoulli effect). As gas velocity increases past an obstructing lesion, this effect is increased, causing dynamic collapse of the nonrigid airway and flow limitation, with a reduction in peak inspiratory flow and a flattening of the inspiratory limb of the flow volume loop. In contrast, during forced expiration the intraluminal pressure is positive relative to the atmosphere, preserving expiratory flow. These lesions occur above the thoracic inlet and include bilateral vocal cord paralysis, paradoxical movement of the vocal cords, and tracheomalacia of the extrathoracic airway.
During forced expiration the intrathoracic airways have a tendency to narrow as a result of airway compression and the Bernoulli effect. This leads to a reduction in peak expiratory flow and a flattening of the expiratory limb of the flow volume loop. Inspiratory flow, in contrast, is preserved as lung expansion increases the radius of the airway at the site of the obstructing lesion. Common causes of variable intrathoracic obstruction include low tracheal tumors and tracheomalacia of the intrathoracic airway.6
Fixed upper airway obstruction occurs when airflow at the site of obstruction is insensitive to the effects of the respiratory cycle because the lesion imparts rigidity to the walls of the affected area. Affected patients have reductions in peak inspiratory and expiratory flow, while the flow volume loop depicts flattening of the inspiratory and expiratory limbs. Examples of this disorder include subglottic stenosis and some tumors.
CLINICAL PRESENTATION AND INITIAL EVALUATION
Patients presenting with upper airway obstruction may complain of a variety of symptoms including hoarseness, stridor, hemoptysis, dysphagia, odynophagia, drooling, and swelling of the neck or face. Dyspnea is typically exacerbated by exercise, and in the case of certain diseases—for example, anterior mediastinal tumors—by the supine position. In many cases prior evaluations have yielded a diagnosis of asthma or chronic obstructive pulmonary disease. While certain disorders such as epiglottitis have very acute presentations, at times symptoms have developed so insidiously that the patient has habituated to the condition, and has few or no complaints.
If time permits, initial evaluation should include a history of the present illness, focusing on the duration of symptoms and any associated oropharyngeal, gastrointestinal, or constitutional symptoms, along with a history of prior upper aerodigestive tract disorders, recent dental problems or procedures, and smoking. Physical examination is directed toward localizing the site of the lesion. Inspiratory stridor generally indicates a lesion at or above the level of the glottis, while biphasic stridor (stridor present during both inspiration and expiration), which is usually higher in pitch, suggests a lesion at the subglottic or tracheal level. The presence of stridor indicates a severe degree of narrowing, typically to ≤6 mm. Supraglottic lesions may cause a muffling of the voice, while oral abscesses may cause a “hot potato voice” (ie, the speech of someone who has a hot potato in his mouth). Hoarseness accompanies unilateral vocal cord paralysis. An oral examination should be performed, unless epiglottitis is suspected and skilled airway personnel are not present. The submental and submandibular regions should be palpated, along with the neck and cervical and supraclavicular lymph nodes.
The first priority in encountering a patient with suspected UAO is to determine the severity of obstruction. When the obstruction is severe and loss of the airway is feared, the airway should be secured by an experienced operator. Arterial desaturation is an extremely late sign of UAO in the patient with normal lungs, and often heralds a catastrophe. This is illustrated by the difficulty normal, untrained individuals have in achieving arterial desaturation during breath holding. Similarly, arterial blood gases provide little information beyond that obtained through the bedside assessment of an experienced clinician. Better indicators of severe airway obstruction include stridor, poor air movement, accessory muscle use, abnormal mentation or agitation, tachycardia, hypertension, and pulsus paradoxus. All patients with newly diagnosed UAO of more than trivial severity should be monitored in an ICU until treatment can be initiated or clinical stability can be determined.
If UAO is suspected but there is no immediate risk of losing the airway, further evaluation may employ a range of techniques, depending on the suspected diagnosis. Spirometry is useful in the elective evaluation of subacute to chronic UAO; however, because the airway must be narrowed to ≤8 mm in order to affect the flow volume loop, spirometry is relatively insensitive. Inspection of the flow volume loop for flattening of the inspiratory or expiratory limb is the most reliable spirometric indication of UAO, particularly when done by an experienced reader. Poor effort may mimic UAO but is suggested by poor reproducibility of the loops and by the technician’s subjective assessment of inadequate patient effort. In such cases it is necessary to either repeat the tests or consider an alternative diagnostic approach if the patient appears unable to provide high quality loops. Spirometry may fail to detect even significant degrees of UAO in patients with severe chronic obstructive pulmonary disease.
Plain chest radiographs may demonstrate tracheal deviation from masses arising in the mediastinum or neck. Lateral neck films may suggest the diagnosis of croup or epiglottitis. Computed tomography (CT) is extremely useful in evaluating suspected tumors of the upper airway, and in characterizing the extent of upper airway soft tissue infections. Three-dimensional reconstruction is useful in identifying fixed anatomic abnormalities of the upper airway, such as tracheal stenosis, and in following the response to therapy.7 However, dynamically determined disorders such as tracheomalacia generally require direct visualization.
Endoscopic evaluation may be flexible or rigid. Rigid endoscopy is useful in the management of suspected foreign body aspiration. Flexible endoscopy may be performed via the oropharyngeal or nasopharyngeal route.
CAUSES OF UPPER AIRWAY OBSTRUCTION
Benign and malignant masses of the nose and nasopharynx constitute important sources of morbidity, and occasionally, mortality. However, because ventilation can usually be maintained via the oropharyngeal route in these cases, they will not be discussed here.
Infectious Causes: Infectious etiologies represent relatively common causes of upper airway obstructing lesions. Ludwig angina is a deep neck infection of the submandibular space of frequently odontogenic origin that commonly begins as a cellulitis but may progress to a fasciitis and subsequently to a true abscess.8 The source of infection is usually a second or third mandibular molar tooth, with causative organisms representing typical oral flora: viridans group streptococci, staphylococci, and anaerobes. Mixed aerobic and anaerobic infections are typical, mandating broad spectrum coverage. Methicillin-resistant Staphylococcus auerus (MRSA) infection should be considered as a potential pathogen in communities with a high prevalence of MRSA colonization, or when the patient is immunocompromised or has other risk factors for this infection. Gram-negative and multi-drug resistant organisms including Pseudomonas aeruginosa and the extended-spectrum β-lactamase-producing Enterobacteriaceae should be considered as potential etiologies in patients with risk factors for altered oral flora: neutropenia, diabetes mellitus, or other immunocompromised state, recent antibiotic use or hospitalization, residence in a nursing home or chronic care facility, or postoperative infection. Airway obstruction may result from elevation and posterior displacement of the tongue and supraglottic edema. The infection may extend to the lateral and retropharyngeal spaces, and subsequently along the carotid sheath and to the mediastinum.
Affected patients present with dysphagia, neck swelling (“bull neck”) and stiffness, trismus, drooling, and brawny induration of the floor of the mouth. Occasionally, crepitus of the submandibular area is present. Tooth pain or a history of recent tooth extraction is usual, but not invariable. While not all patients with Ludwig angina need to undergo endotracheal intubation or tracheostomy, the decision to observe the airway rather than secure it should not be made lightly, and should be made after consultation with an otolaryngologist. If intubation is deemed necessary, placement via a flexible fiberoptic approach may be useful in decreasing the risk of laryngospasm during the procedure. Treatment consists of antibiotic therapy, and in some patients, surgical decompression and drainage. Obviously, any infected teeth should be extracted. The mainstays of management of Ludwig angina—airway protection, broad-spectrum antibiotic use, and surgical decompression—have reduced the mortality from this disease to below 10%.
Lymphatic drainage from the oropharynx, teeth, maxillary sinuses, and ears passes through the retropharyngeal space, predisposing it to infections from the ear, nose, and throat.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree