Figure 3.1 Solar energy used to charge and power medical equipment in the remote environment. (a) Photovoltaic panels are used to charge a battery. (b) The charged battery is then used to power various equipment, including a portable ultrasound machine and netbook computer. Image courtesy of N. Stuart Harris, MD.
Finally, in developing ultrasound programs in resource-poor regions, it is important to consider the maintenance and sustainability of a program. Machine and transducer maintenance, contact gel, and cleansing solution do add a small but continued financial commitment to ultrasound use. Likely of greatest concern and need in the developing world is the adequate training of providers in the use and interpretation of sonography. Any sustainable program requires a continued experienced presence in the field to maintain the use and quality assurance of clinical ultrasound; this is often the greatest challenge as well-trained personnel are few and far between. Ultrasound training should include the long-term planning of projects with a concern for sustainability. Ideally these programs should involve trainees becoming trainers themselves, and creating a self-maintained ultrasound program.
Applications in the developing world
The various uses of ultrasound add to its utility in a setting where X-ray availability may be limited or non-existent and more advanced imaging may require transfer to far-off tertiary care centers. With a variety of transducers, one portable ultrasound machine may be used for multiple common indications such as echocardiography, obstetrics, and trauma. Other diagnostic abilities include long-bone fracture detection, pulmonary sonography, musculoskeletal, and soft tissue imaging. Sonography is also commonly used for procedural guidance. These applications include venous access, lumbar puncture, thoracentesis, paracentesis, pericardiocentesis, arthrocentesis, and nerve blocks for painful procedures. This “multi-use” phenomenon makes portable ultrasound particularly well adapted for the austere setting. While most of these studies can be performed with a single curvilinear transducer, optimal performance and diagnostics would be accomplished with a variety of transducers, including linear, phased-array, and endocavitary probes, which unfortunately add to the cost of a machine.
Despite having so many potential applications, there has been little focused, long-term research looking at the clinical

Figure 3.2 Training courses abroad should be tailored to the needs of the local clinicians. A point person should be identified, and continuing education and oversight should be established. This course was performed in Roatan, Honduras. Dr. Suzanne Hiramatsu instructs local physician Dra. Cibeles Mejia in the evaluation of the E-FAST examination, aorta, gallbladder, and pregnancy.
and cost outcomes when adding diagnostic ultrasound to various practice settings in the developing world. Obstetric ultrasound has received particular attention, since it has the potential to improve maternal and fetal outcomes in the developing world. In contrast to childbearing in industrialized nations, pregnancy and childbirth remain perilous in the developing world. Almost all maternal deaths in a 2005 estimate by the WHO occurred in the developing world. Maternal mortality is the leading cause of death for women of childbearing age, and accounts for more than 15% of deaths in this age group. Estimating the lifetime risk of maternal death highlights the disparity between developed and underdeveloped nations: 1 out of 7 women in some parts of Sub-Saharan Africa who become pregnant will eventually die of a maternal-related cause; in most of Europe, this rate is about 1 per 48,000. The risk to the fetus is even more pronounced and equally disproportionate. Current estimates of annual perinatal deaths stand at approximately six million, with the developing world accounting for about 98% of this number. With minimal training, point-of-care sonography can prevent potential obstetric emergencies in resource-restricted settings. Although there is a lack of large studies that indicate a change in mortality as a result of obstetric ultrasound use, there is evidence that indicates a significant change in patient management as a result of point-of-care obstetric sonography performed by health providers (physicians and midwives). Common findings with ultrasound in rural and remote settings include non-vertex lie of the fetus, multiple gestation, lack of fetal heart rate, and abnormal placenta positioning. Additionally, ultrasound can be used to assess for intrauterine fetal demise, ectopic pregnancy, and gross fetal anomalies. Although many developing countries have restrictive abortion laws, therapeutic abortion for major fetal malformation is permitted in many places. Routine ultrasound can therefore influence perinatal and infant mortality, through the early discovery and abortion of fetuses with major malformations. For less severe fetal abnormalities, the early diagnosis and awareness can help formulate a clear management plan, which may include the place of delivery (e.g. at a tertiary hospital with adequate neonatal care facilities), mode of delivery (e.g. planned cesarean section), and, sometimes, timing of delivery (Figure 3.3).
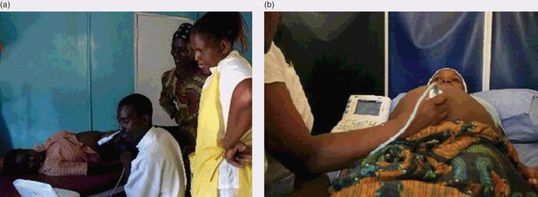
Figure 3.3 Prenatal sonography taught to midwives in rural care centers in Zambia. (a) A portable machine is used to estimate gestational age. (b) Ultrasound plays a vital role in prenatal care in the developed world. In resource-limited settings, the availability of an ultrasound machine and skilled operator aid in the detection of high-risk pregnancies and the decision to refer high-risk patients for further care.
Trauma is one of the leading causes of death and disability worldwide. A lack of trained specialists in trauma and resuscitation is coupled with the lack of availability of advanced diagnostic imaging, limiting trauma care in developing countries. In addition, equipment shortage, facility disrepair, and improper maintenance of resources compound existing challenges. The FAST examination is frequently used to assess the presence of intraperitoneal or pericardial bleeding in trauma. It has been introduced to developing nations and is identified by the WHO as desirable in their Guidelines for Essential Trauma Care. While CT scanning remains the gold standard in terms of radiologic assessment in trauma, it has been proposed that FAST may be an acceptable alternative in resource-poor facilities where CT scans are unavailable. The early ultrasound detection of free fluid in the trauma patient could be used as an indication to expedite transfer to a center that has advanced imaging capabilities, thereby reducing overall morbidity and mortality. Additionally, at the peripheral hospitals with no CT scanning and limited radiology, the results of the FAST could be communicated to the surgeon or specialist at the referral hospital, providing useful information to surgeons in referral centers (Figure 3.4).

Figure 3.4 Ultrasound in locations where advanced imaging is unavailable. This trauma surgeon, Dr. Indira Sanchez in Roatan, Honduras, uses point-of-care ultrasound to determine whether this patient needs to be operated on. She is the only surgeon on the entire island with a population of 70,000+ and no CT scanner.
Another useful application of handheld ultrasound in the developing world is point-of-care echocardiography for the detection of structural cardiac anomalies. In particular, rheumatic heart disease (RHD) is estimated to affect 15.6–19.6 million people worldwide and causes 233,000–492,000 deaths each year, 95% of which occur in developing countries. While Africa has about 10% of the world’s population, as many as half of the 2.4 million children affected by RHD globally live on the continent. Rheumatic heart disease accounts for a major proportion of all cardiovascular disease in children and young adults throughout Africa, Asia, and South America. While acute rheumatic fever is on the decline in the developing world, there are still a large number of chronic rheumatic heart disease cases, often detected as an incidental finding on clinical examination or undetected until the disease is complicated by chronic congestive heart failure and recurrent thromboembolic phenomena. Echocardiography is a highly accurate method for diagnosing and characterizing valvular lesions. With appropriate training, care providers in remote settings have been able to detect valvular lesions not heard on clinical examination. In fact, the use of portable ultrasound machines has resulted in the detection of more RHD in developing nations over the last few years; over 80% of lesions noted on point-of-care ultrasound were inaudible to experienced auscultators. In addition to being a tool to diagnose cardiac lesions, ultrasound may be also used in the management of heart disease. Combining echocardiography and pulmonary ultrasound to detect pulmonary edema can be used to target optimal diuresis and fluid management in patients with heart failure and valvular insufficiency. In places where central venous pressure monitoring and chest X-ray are unavailable, sonographic assessment may be critical in patient management (Figure 3.5).
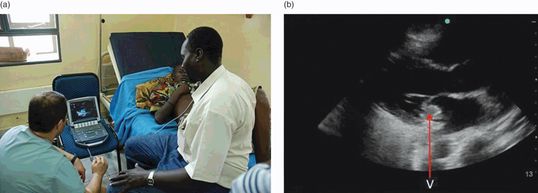
Figure 3.5 Ultrasound for the detection of rheumatic heart disease. (a) A young adult male receives an echocardiogram after presenting with fever and hemiparesis in Juba, South Sudan. (b) The patient was found to have a large vegetation (V) with regurgitant flow across his mitral valve, consistent with the diagnosis of endocarditis and rheumatic heart disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








