Ultrasound-Guided Transversus Abdominis Plane Block and Quadratus Lumborum Block
Part 1: Transversus Abdominis Plane Block
Kim Russon
Rafael Blanco
 Background and indications: The transversus abdominis plane block, more commonly referred to as the TAP block, places local anesthetic in the lateral abdominal wall in a plane between the internal oblique and the transversus abdominis muscles. Here, the local anesthetic block can block many of the abdominal nerves as they pass to the abdominal structures. The TAP block was first described by O’Donnell et al.1 in 2006. Their original technique was a blind technique using a blunt regional anesthesia needle and relied on feeling a double pop as the needle passed through the layers in an area known as the triangle of Petit. Since then, the technique has been modified to utilize ultrasound to confirm placement of the local anesthetic. Studies (although numbers remain small) have shown bilateral TAP blocks to provide effective postoperative analgesia after prostatectomy,1 large and small bowel resection,2 and cesarean section3 compared to morphine. Intuition suggests that if the nerves to the abdominal wall and peritoneum can be numbed with this block, then it is likely to be useful in providing pain relief following many other abdominal surgical, gynecological, and urological procedures.
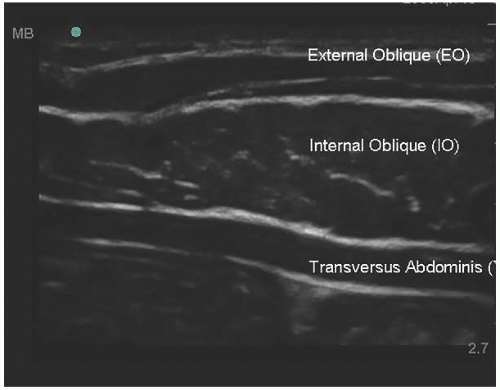
Background and indications: The transversus abdominis plane block, more commonly referred to as the TAP block, places local anesthetic in the lateral abdominal wall in a plane between the internal oblique and the transversus abdominis muscles. Here, the local anesthetic block can block many of the abdominal nerves as they pass to the abdominal structures. The TAP block was first described by O’Donnell et al.1 in 2006. Their original technique was a blind technique using a blunt regional anesthesia needle and relied on feeling a double pop as the needle passed through the layers in an area known as the triangle of Petit. Since then, the technique has been modified to utilize ultrasound to confirm placement of the local anesthetic. Studies (although numbers remain small) have shown bilateral TAP blocks to provide effective postoperative analgesia after prostatectomy,1 large and small bowel resection,2 and cesarean section3 compared to morphine. Intuition suggests that if the nerves to the abdominal wall and peritoneum can be numbed with this block, then it is likely to be useful in providing pain relief following many other abdominal surgical, gynecological, and urological procedures. Anatomy: The abdominal wall between the iliac crest and the subcostal margin consists of three layers of muscle (external oblique, internal oblique, transversus abdominis) covered by connective tissue and skin (Fig. 35.1). The transversus abdominis is the deepest layer, and below it is the peritoneum. The skin, muscles, and peritoneum of the anterior abdominal wall are innervated by the lower six thoracic nerves and the first intercostal nerve. At the costal margin, thoracic nerves 7 to 11 leave their intercostal spaces and enter the neurovascular plane of the abdominal wall between transversus abdominis and internal oblique (Fig. 35.1). Running across the surface of the transversus abdominis muscle and aponeurosis are the lower intercostal, subcostal and iliohypogastric nerves.
Anatomy: The abdominal wall between the iliac crest and the subcostal margin consists of three layers of muscle (external oblique, internal oblique, transversus abdominis) covered by connective tissue and skin (Fig. 35.1). The transversus abdominis is the deepest layer, and below it is the peritoneum. The skin, muscles, and peritoneum of the anterior abdominal wall are innervated by the lower six thoracic nerves and the first intercostal nerve. At the costal margin, thoracic nerves 7 to 11 leave their intercostal spaces and enter the neurovascular plane of the abdominal wall between transversus abdominis and internal oblique (Fig. 35.1). Running across the surface of the transversus abdominis muscle and aponeurosis are the lower intercostal, subcostal and iliohypogastric nerves. Probe position: Transverse or transverse oblique between the margin of the 12th rib and superior iliac spine.
Probe position: Transverse or transverse oblique between the margin of the 12th rib and superior iliac spine. Needle: 22G blunt needle (5 to 10 cm) for single injection; 18G Tuohy needle (5 to 10 cm) for continuous infusions.
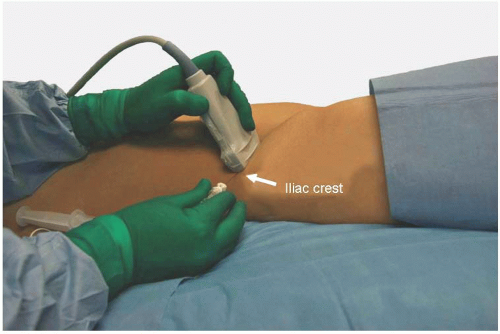
Needle: 22G blunt needle (5 to 10 cm) for single injection; 18G Tuohy needle (5 to 10 cm) for continuous infusions. Technique: This block may be performed before or following induction of general or spinal anesthesia. The patient needs to be lying supine. An aseptic technique is advocated using a no-touch technique, an appropriate cleaning solution, and a sterile cover for the ultrasound probe. The ultrasound probe is positioned horizontally on the skin just above the iliac crest in the midaxillary line (Fig. 35.2). The muscle layers are identified (Fig. 35.3). The authors prefer to use a peripheral nerve block needle because it allows “disTant” injection
Technique: This block may be performed before or following induction of general or spinal anesthesia. The patient needs to be lying supine. An aseptic technique is advocated using a no-touch technique, an appropriate cleaning solution, and a sterile cover for the ultrasound probe. The ultrasound probe is positioned horizontally on the skin just above the iliac crest in the midaxillary line (Fig. 35.2). The muscle layers are identified (Fig. 35.3). The authors prefer to use a peripheral nerve block needle because it allows “disTant” injection by your assisTant while you remain in control of the ultrasound probe and needle. A 50-mm needle is usually sufficient. The authors use an in-plane approach, inserting the needle posteriorly and directing anteriorly. The needle is followed under direct vision as it passes through the muscle layers until the tip lies between the internal oblique and transversus abdominis muscles (Fig. 35.4).
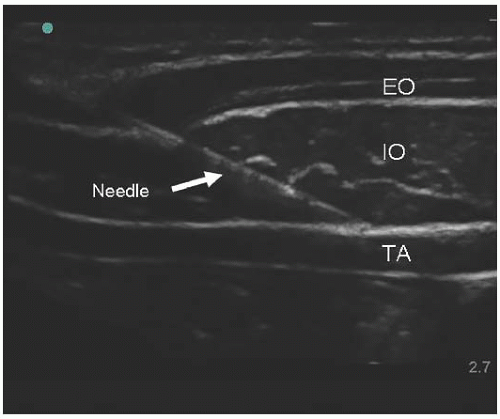 Figure 35.4. Ultrasound scan with needle. EO, external oblique; IO, internal oblique; TA, transversus abdominis. |
Injection of the local anesthetic must be seen to ensure correct placement. It is very cHaracteristic to see the layer expanding in an ellipsoid way (Fig. 35.5). The authors use 20 mL of 0.375% levobupivacaine in each side, as do McDonnell et al.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree