Ultrasound-Guided Lumbar Facet Medial Branch Block and Intra-articular Facet Joint Injection
Kacey A. Montgomery
Michael Gofeld
 Background and indications: Zygapophyseal joint (facet joint) syndrome is a common cause of axial low back pain among patients that present to chronic outpatient pain clinics. Patients may complain of back pain, buttock pain, or pain referred to the posterior thigh or inguinal area. Lumbar spondylosis or facet joint osteoarthritis-mediated pain is transmitted via lumbar medial branch nerves. These nerves can be blocked for diagnostic purposes and eventually ablated if indicated and confirmed as the source of pain. Alternatively, for therapeutic purposes, intra-articular facet joint steroid injections can be performed.
Background and indications: Zygapophyseal joint (facet joint) syndrome is a common cause of axial low back pain among patients that present to chronic outpatient pain clinics. Patients may complain of back pain, buttock pain, or pain referred to the posterior thigh or inguinal area. Lumbar spondylosis or facet joint osteoarthritis-mediated pain is transmitted via lumbar medial branch nerves. These nerves can be blocked for diagnostic purposes and eventually ablated if indicated and confirmed as the source of pain. Alternatively, for therapeutic purposes, intra-articular facet joint steroid injections can be performed. Anatomy: Each vertebra is connected to the vertebra above and below by facet joints posteriorly and intervertebral discs anteriorly. The facet joint is formed by the inferior articular process (IAP) from the vertebra above and the superior articular process (SAP) from the vertebra below and can accumulate a volume of approximately 1 to 1.5 mL. The superior facet surface has a concave shape that articulates with the convex surface of the inferior facet (Fig. 54.1A to C). These articulations allow flexion but limit rotation. A segmental nerve root exits the corresponding neural foramen and divides into the ventral and dorsal rami. The dorsal ramus has the medial, intermediate, and lateral branches. The facet joint is innervated by the medial branch at that corresponding level and the level above that must be anesthetized in order to block pain generated by a single facet joint. If the pathology exists at a single lumbar level, the median branch at that level as well as at the level above it must be blocked to provide pain relief because of the dual innervation of the joint.
Anatomy: Each vertebra is connected to the vertebra above and below by facet joints posteriorly and intervertebral discs anteriorly. The facet joint is formed by the inferior articular process (IAP) from the vertebra above and the superior articular process (SAP) from the vertebra below and can accumulate a volume of approximately 1 to 1.5 mL. The superior facet surface has a concave shape that articulates with the convex surface of the inferior facet (Fig. 54.1A to C). These articulations allow flexion but limit rotation. A segmental nerve root exits the corresponding neural foramen and divides into the ventral and dorsal rami. The dorsal ramus has the medial, intermediate, and lateral branches. The facet joint is innervated by the medial branch at that corresponding level and the level above that must be anesthetized in order to block pain generated by a single facet joint. If the pathology exists at a single lumbar level, the median branch at that level as well as at the level above it must be blocked to provide pain relief because of the dual innervation of the joint.The location of the medial branch nerve is uniformly located at the base of the SAP between the neural foramen and the mammillo-accessory ligament. After innervating the multifidus muscle, the medial branch gives off the superior and inferior articular branches to the corresponding facet joint above and below (see Fig. 54.1A, B). The L5 medial branches have a variable course. Thus, the L5 dorsal ramus is targeted at the junction of S1 SAP and the sacral ala (see Fig. 54.1C).
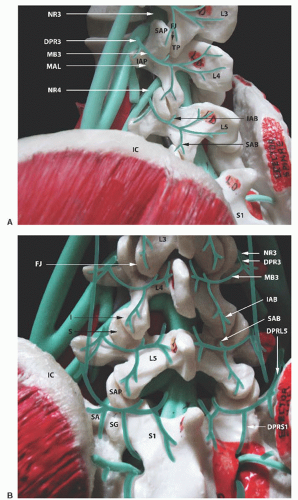 Figure 54.1. A: Lateral view of the spine. DPR3, dorsal primary ramus of nerve root 3; FJ, facet joint; IAB, inferior articular branch; IAP, inferior articular process; IC, iliac crest; MAL, mamillo-accessory ligament; MB3, medial branch from nerve root 3; NR3, nerve root 3; NR4, nerve root 4; SAB, superior articular branch; SAP, superior articular process; TP, transverse process. B: Anatomy of the L5 dorsal ramus. DPR3, dorsal primary ramus of nerve root 3; DPRL5, dorsal primary ramus of L5; DPRS1, dorsal primary ramus of S1; FJ, facet joint; I, inferior articular process; IAB, inferior articular branch; IC, iliac crest; MB3, medial branch from nerve root 3; NR3, nerve root 3; S, sacrum; SA, sacrum ala; SAB
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|








