Ultrasound-Guided Lower Extremity Blockade in Children
Ralph Beltran
Joseph D. Tobias
Stephen Lucas
Paul E. Bigeleisen
Depending on the site of surgery or injury and the nerves that need to be anesthetized, there are several regional anesthesia techniques of the lower extremity that may be applicable to the pediatric population. These techniques may be used for procedures of the foot and ankle (such as club foot repair or tendon lengthening of the lower extremity) or for major operations of the femur and hip (including the treatment of traumatic femoral fractures or open reduction and internal fixation of the hip due to traumatic or congenital conditions). In addition to their use for postoperative analgesia, isolated blocks of the lower extremity may be used instead of anesthesia in patients with comorbid diseases, which may increase the risk of general anesthesia, such as in patients with undiagnosed myopathy. In these patients, muscle biopsy can generally be accomplished with femoral nerve block or a fascia iliaca block. Alternatively, there are also isolated case reports of the use of regional anesthesia to induce sympathectomy in the lower extremity for treatment of vascular compromise of various etiologies. In the past, analgesia following lower extremity procedures was most commonly accomplished with the use of a caudal approach; however, given data demonstrating the efficacy and lower risk of adverse events with peripheral nerve blockade versus caudal epidural block, it is likely that there will be increasing use of peripheral nerve block of the lower extremity.
Lumbar plexus block
 Background and Indications: The most proximal approach to the lumbar plexus is direct block at the lumbar plexus. The technique provides anesthesia of the three nerves of the lumbar plexus (femoral, lateral femoral cuTaneous, and obturator) with a single injection. This approach is also commonly referred to as the psoas compartment block. The authors advocate a slightly more medial approach (Fig. 41.3) to needle insertion than that described in the adult population. As with the techniques of Winnie et al. and Chayen et al., a line is drawn through the posterior superior iliac spine (PSIS) parallel to the spine. A second line is drawn connecting the two iliac crests (the intercristal line). The point of intersection of these two lines is identified and the needle is moved slightly (1 to 2 cm) medially along the intercristal line. The needle is inserted at a 90-degree angle to the skin and advanced using a nerve stimulator. In addition, ultrasound guidance can be used with the needle in plane with the transducer held in the transfer or longitudinal plane. As the psoas compartment is entered, a loss of resisTance is felt and a muscle response in the quadriceps muscle will be obtained. During needle insertion, if the transverse process is contacted, the needle is walked off the transverse process in either a caudad or cephalad direction. The lumbar and sacral plexuses lie in the same anatomic planes in the paravertebral space along the vertebral column, consequently variable analgesia of the sacral plexus occurs. The potential to achieve anesthesia of both the lumbar and sacral plexus makes this approach suitable for femoral osteotomies as well as surgical procedures of the hip. Although there are limited data in the pediatric population, lumbar plexus analgesia can be used to provide analgesia following major orthopedic surgical procedures of the hip, such as triple osteotomy of the pelvis, or femur surgery, such as femoral osteotomy.
Background and Indications: The most proximal approach to the lumbar plexus is direct block at the lumbar plexus. The technique provides anesthesia of the three nerves of the lumbar plexus (femoral, lateral femoral cuTaneous, and obturator) with a single injection. This approach is also commonly referred to as the psoas compartment block. The authors advocate a slightly more medial approach (Fig. 41.3) to needle insertion than that described in the adult population. As with the techniques of Winnie et al. and Chayen et al., a line is drawn through the posterior superior iliac spine (PSIS) parallel to the spine. A second line is drawn connecting the two iliac crests (the intercristal line). The point of intersection of these two lines is identified and the needle is moved slightly (1 to 2 cm) medially along the intercristal line. The needle is inserted at a 90-degree angle to the skin and advanced using a nerve stimulator. In addition, ultrasound guidance can be used with the needle in plane with the transducer held in the transfer or longitudinal plane. As the psoas compartment is entered, a loss of resisTance is felt and a muscle response in the quadriceps muscle will be obtained. During needle insertion, if the transverse process is contacted, the needle is walked off the transverse process in either a caudad or cephalad direction. The lumbar and sacral plexuses lie in the same anatomic planes in the paravertebral space along the vertebral column, consequently variable analgesia of the sacral plexus occurs. The potential to achieve anesthesia of both the lumbar and sacral plexus makes this approach suitable for femoral osteotomies as well as surgical procedures of the hip. Although there are limited data in the pediatric population, lumbar plexus analgesia can be used to provide analgesia following major orthopedic surgical procedures of the hip, such as triple osteotomy of the pelvis, or femur surgery, such as femoral osteotomy.Other investigators have provided recent additional insight into the use of the lumbar plexus block in the pediatric population. Using ultrasound guidance, Kirchmair1 demonstrated that weight rather than age provided the best measure for estimating the depth of the lumbar plexus in a cohort of 32 children. The patients were stratified into three age groups (3 to 5 years, 5 to 8 years, and more than 8 years). The lumbar plexus could be delineated in 19 of 20 cases in group 1, 17 of 20 cases in group 2, 22 of 24 cases at either L3-L4 or L4-L5. In all patients, the lumbar plexus was situated within the posterior part of the psoas major muscle. The strongest positive correlation existed between skin-to-plexus disTances and the children’s weight. Although there was a significant increase in the skin-to-plexus disTance in the three groups, no difference was noted in the skin-to-plexus disTance at L3-L4 versus L4-L5. The disTance from the skin to the anterior border of the lumbar plexus at L3-L4 was 2.5 ± 0.4, 2.7 ± 0.5, and 3.2 ± 0.3 cm in the three groups, respectively. The authors concluded that ultrasound guidance enabled safe und successful posterior approaches to the lumbar plexus, thus resulting in effective anesthesia and analgesia of the inguinal region. Although this study demonstrated that the lumbar plexus was within the body of the psoas major muscle in all cases, subsequent work from the same group has demonstrated that the lumbar plexus occasionally is located posterior to the psoas major muscle. In a prospective randomized comparison of continuous epidural versus lumbar plexus block following surgical procedures of the hip and femur in a cohort of 40 children, lumbar plexus block provided equivalent analgesia with a superior adverse effect profile. The cohort for the study included 40 children. After the induction of general induction, 0.5 mL/kg of 0.375% ropivacaine was injected via the epidural or lumbar plexus catheter. This was followed postoperatively by an infusion of 0.2% ropivacaine at 0.1 mL/kg/hr for the lumbar plexus catheter or 0.2 mL/kg/hr for the epidural. Postoperative analgesia was excellent for both continuous block techniques with comparable pain scores and need for supplemental analgesia. The number of children who had at least one adverse effect, plasma ropivacaine levels, and the need to stop the local anesthetic infusion prematurely was significantly higher in epidural group. These data and other investigators have demonstrated the efficacy of lumbar plexus blockade in providing analgesia following hip and femur surgery in the pediatric population. Although rare, reported complications for lumbar plexus blockade have included cardiac arrest during intravascular injection, muscular and renal hematoma, epidural anesthesia, spinal blockade, and retroperitoneal injection.
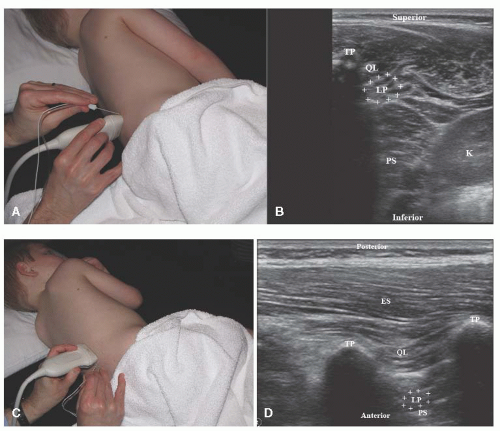
 Anatomy: The sensory and motor innervation of the lower extremity is derived from the lumbar and sacral plexuses. The lumbar plexus is formed by the union of the anterior rami of the first four lumbar nerves (L1-L4) with variable input from the 12th thoracic nerve (T12) and L5. The lumbar plexus lies in the “psoas compartment” in the paravertebral space. The anterior border of the compartment is formed by the psoas major, and the posterior border is formed by the quadratus lumborum/erector spinae muscles (Fig. 41.1 A to D). In many cases, the lumbar plexus lies within the psoas muscle. As the lumbar plexus emerges from the psoas compartment, it divides into the three nerves that innervate the anterior portion of the proximal aspect of the lower extremity: the femoral nerve, the lateral femoral cuTaneous nerve, and the obturator nerve. The femoral nerve provides sensory innervation to the anterior and medial aspects of the thigh and motor innervation to the quadriceps muscles (Fig. 41.2 A,B). The lateral femoral cuTaneous nerve is purely sensory, providing sensory innervation to the lateral aspect of the thigh. It branches from the lumbar plexus and enters the thigh deep to the inguinal ligament, medial to the anterior superior iliac spine. The obturator nerve provides motor innervation to the adductors of the leg as well as sensory innervation to part of the medial aspect of the lower portion of the thigh. The obturator nerve also innervates the knee joint, making it necessary to anesthetize to achieve analgesia following procedures involving the knee.
Anatomy: The sensory and motor innervation of the lower extremity is derived from the lumbar and sacral plexuses. The lumbar plexus is formed by the union of the anterior rami of the first four lumbar nerves (L1-L4) with variable input from the 12th thoracic nerve (T12) and L5. The lumbar plexus lies in the “psoas compartment” in the paravertebral space. The anterior border of the compartment is formed by the psoas major, and the posterior border is formed by the quadratus lumborum/erector spinae muscles (Fig. 41.1 A to D). In many cases, the lumbar plexus lies within the psoas muscle. As the lumbar plexus emerges from the psoas compartment, it divides into the three nerves that innervate the anterior portion of the proximal aspect of the lower extremity: the femoral nerve, the lateral femoral cuTaneous nerve, and the obturator nerve. The femoral nerve provides sensory innervation to the anterior and medial aspects of the thigh and motor innervation to the quadriceps muscles (Fig. 41.2 A,B). The lateral femoral cuTaneous nerve is purely sensory, providing sensory innervation to the lateral aspect of the thigh. It branches from the lumbar plexus and enters the thigh deep to the inguinal ligament, medial to the anterior superior iliac spine. The obturator nerve provides motor innervation to the adductors of the leg as well as sensory innervation to part of the medial aspect of the lower portion of the thigh. The obturator nerve also innervates the knee joint, making it necessary to anesthetize to achieve analgesia following procedures involving the knee. Patient position: Lateral decubitus with knees and hips flexed as feasible or Sims position, with side to be blocked upright.
Patient position: Lateral decubitus with knees and hips flexed as feasible or Sims position, with side to be blocked upright. Transducer: Depending on the size of the patient, either the 35-mm linear array oscillating at 13 MHz or the curved 11-mm intermediate frequency probe oscillating at 5 to 10 MHz will allow visualization of bony structures, psoas major muscle, and in most cases the lumbar plexus. The lower frequency probe is used for larger patients given its increased depth of penetration.
Transducer: Depending on the size of the patient, either the 35-mm linear array oscillating at 13 MHz or the curved 11-mm intermediate frequency probe oscillating at 5 to 10 MHz will allow visualization of bony structures, psoas major muscle, and in most cases the lumbar plexus. The lower frequency probe is used for larger patients given its increased depth of penetration. Transducer orientation: Transverse, just below the site of needle insertion, using an in-plane technique. Alternatively, the transducer can be placed in the longitudinal plane with the needle inserted caudad (distal) to the transducer (in plane).
Transducer orientation: Transverse, just below the site of needle insertion, using an in-plane technique. Alternatively, the transducer can be placed in the longitudinal plane with the needle inserted caudad (distal) to the transducer (in plane). Needle: Depending on the size of the patient and the depth of the lumbar plexus, either a 20G, 6-inch or 21G, 4-inch needle is used. Alternatively, an 18G insulated Tuohy needle of variable length can be used if a catheter is going to be placed for a continuous infusion.
Needle: Depending on the size of the patient and the depth of the lumbar plexus, either a 20G, 6-inch or 21G, 4-inch needle is used. Alternatively, an 18G insulated Tuohy needle of variable length can be used if a catheter is going to be placed for a continuous infusion. Local anesthetic agent: The volume is dependent on the size of the patient, and the concentration is dependent on the degree of motor blockade that is desired. For postoperative analgesia, 0.25% bupivacaine or 0.2% ropivacaine are effective, whereas 0.5% concentrations are used to provide surgical anesthesia and profound motor blockade. In most patients, a volume of 0.2 to 0.4 mL/kg is sufficient. In all cases, the total dose of bupivacaine or ropivacaine should not exceed 3 mg/kg. Epinephrine in a concentration of 1:200,000 is added to the solution. For continuous infusions, 0.2% ropivacaine is infused at 0.1 mL/kg/hr.
Local anesthetic agent: The volume is dependent on the size of the patient, and the concentration is dependent on the degree of motor blockade that is desired. For postoperative analgesia, 0.25% bupivacaine or 0.2% ropivacaine are effective, whereas 0.5% concentrations are used to provide surgical anesthesia and profound motor blockade. In most patients, a volume of 0.2 to 0.4 mL/kg is sufficient. In all cases, the total dose of bupivacaine or ropivacaine should not exceed 3 mg/kg. Epinephrine in a concentration of 1:200,000 is added to the solution. For continuous infusions, 0.2% ropivacaine is infused at 0.1 mL/kg/hr. Technique: For use of ultrasound to guide the lumbar plexus block, sterile preparation of the skin is performed and sterile ultrasound gel is placed over the skin of the lumbar area at the anticipated needle insertion point. The ultrasound probe is placed in a transverse position to identify the bony elements of the vertebral body and the muscles that border the psoas compartment (the quadratus lumborum/erector spinae and the psoas major muscles) (Fig. 41.1A,B). The needle is inserted above (superior) to the probe. The kidney can usually be identified superior (cephalad) to the psoas muscle. In many cases, the lumbar plexus can be visualized within the psoas major muscle. The needle is advanced between two of the transverse processes of the lumbar vertebrae and can be viewed as it pierces the quadratus lumborum/erector spinae muscles and enters the psoas compartment. Once the psoas compartment is entered, the ultrasound transducer can be turned into a longitudinal plane to verify the location of the tip of the needle at the lumbar plexus. Electrostimulation may also be used to confirm needle placement. Once the correct placement of the needle is confirmed, the local anesthetic solution is injected until the plexus is surrounded.
Technique: For use of ultrasound to guide the lumbar plexus block, sterile preparation of the skin is performed and sterile ultrasound gel is placed over the skin of the lumbar area at the anticipated needle insertion point. The ultrasound probe is placed in a transverse position to identify the bony elements of the vertebral body and the muscles that border the psoas compartment (the quadratus lumborum/erector spinae and the psoas major muscles) (Fig. 41.1A,B). The needle is inserted above (superior) to the probe. The kidney can usually be identified superior (cephalad) to the psoas muscle. In many cases, the lumbar plexus can be visualized within the psoas major muscle. The needle is advanced between two of the transverse processes of the lumbar vertebrae and can be viewed as it pierces the quadratus lumborum/erector spinae muscles and enters the psoas compartment. Once the psoas compartment is entered, the ultrasound transducer can be turned into a longitudinal plane to verify the location of the tip of the needle at the lumbar plexus. Electrostimulation may also be used to confirm needle placement. Once the correct placement of the needle is confirmed, the local anesthetic solution is injected until the plexus is surrounded.Some practitioners prefer a longitudinal approach (Fig. 41.1C,D). In this case, a parasagittal scan is obtained that identifies the transverse processes and quadratus lumborum and psoas muscles. In slim patients, the nerve plexus may also be identified. The needle is inserted in line with the probe until the lumbar plexus compartment is entered. Needle position may be confirmed with electrostimulation. Once proper needle placement is confirmed, local anesthetic is injected until the nerve plexus is surrounded.
Femoral nerve block
 Background and Indications: Block of the femoral nerve can be used to provide analgesia following surgical procedures on the anterior or lateral aspect of the thigh, knee arthroscopy, anterior cruciate ligament reconstruction, patellar ligament realignment, and traumatic femur fracture or following femoral osteotomies.
Background and Indications: Block of the femoral nerve can be used to provide analgesia following surgical procedures on the anterior or lateral aspect of the thigh, knee arthroscopy, anterior cruciate ligament reconstruction, patellar ligament realignment, and traumatic femur fracture or following femoral osteotomies.There are two basic approaches described for femoral nerve block. The first involves direct block of the nerve just below the inguinal crease and lateral to the femoral artery.
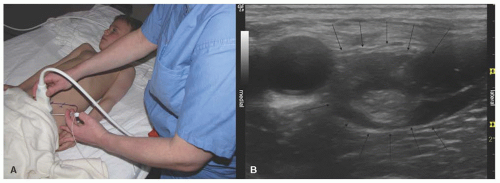
This technique can also be modified to provide what has been termed a 3-in-1 block, or the inguinal perivascular approach, whereby block of the femoral, lateral femoral cuTaneous, and obturator nerve may be feasible (Fig. 41.2A,B). As originally described, the theory behind the block is that a fascial sheath that surrounds the femoral nerve can be used as a conduit to carry local anesthetic centrally to the lumbar plexus. This is accomplished by the use of larger volume of local anesthetic than is used for isolated femoral nerve block and holding pressure distal to the site of injection. Our own cadaver studies suggest that Winnie’s 3-in-1 block was actually an intraneural block wherein the local anesthetic traveled proximally to the origin of the lumbar plexus within the epineurium. Another possibility, shown by our cadaver studies, is that the local anesthetic originally travels proximally about 10 cm within the epineurium and then ruptures into the space containing the three nerves between the psoas and iliacus muscles.
The second approach to the femoral nerve is the fascia iliaca block. With this technique, a large volume of local anesthetic solution is injected more laterally with medial spread to the femoral nerve, superiorly to the obturator and lateral femoral cuTaneous nerves. The point of needle entry is at the junction of the outer and middle third of the line connecting the symphysis pubis and the anterior superior iliac crest (Fig. 41.3). When compared to nerve stimulation, ultrasound guidance in the performance of femoral nerve block in the pediatric population has been shown to result in a longer duration of analgesia and a decrease in the volume of local anesthetic that is required.
 Anatomy: The femoral nerve is the largest branch of the lumbar plexus. It arises from the dorsal division of the anterior rami of L2-L4 and descends into the pelvis lateral to the psoas major muscle, where it passes deep to the inguinal ligament. In the anterior compartment of the thigh, the femoral nerve divides into multiple branches supplying the muscle, joints, and skin of the anterior thigh. The inguinal crease is generally several centimeters caudad to the inguinal ligament. Below the inguinal crease is the level at which the block is performed. At this level, the nerve lies deep to the fascia lata and the fascia iliaca and is separated from the femoral artery and vein by the iliopectineal ligament (Cooper ligament). The anterior branch of the femoral nerve innervates the pectineus muscle and is responsible for thigh adduction on stimulation. The posterior branch innervates the quadriceps femoris muscles and provides leg extension and patellar elevation on stimulation. The superficial branch lies deep to the fascia lata and superior to the fascia iliaca. It stimulates contraction of the sartorius muscle. Because this branch lies above the fascia iliaca, it is not a suitable stimulation end point for femoral nerve block. The saphenous nerve is a cuTaneous branch of the femoral nerve, which supplies innervation to the skin over the medial aspect of the leg and foot.
Anatomy: The femoral nerve is the largest branch of the lumbar plexus. It arises from the dorsal division of the anterior rami of L2-L4 and descends into the pelvis lateral to the psoas major muscle, where it passes deep to the inguinal ligament. In the anterior compartment of the thigh, the femoral nerve divides into multiple branches supplying the muscle, joints, and skin of the anterior thigh. The inguinal crease is generally several centimeters caudad to the inguinal ligament. Below the inguinal crease is the level at which the block is performed. At this level, the nerve lies deep to the fascia lata and the fascia iliaca and is separated from the femoral artery and vein by the iliopectineal ligament (Cooper ligament). The anterior branch of the femoral nerve innervates the pectineus muscle and is responsible for thigh adduction on stimulation. The posterior branch innervates the quadriceps femoris muscles and provides leg extension and patellar elevation on stimulation. The superficial branch lies deep to the fascia lata and superior to the fascia iliaca. It stimulates contraction of the sartorius muscle. Because this branch lies above the fascia iliaca, it is not a suitable stimulation end point for femoral nerve block. The saphenous nerve is a cuTaneous branch of the femoral nerve, which supplies innervation to the skin over the medial aspect of the leg and foot.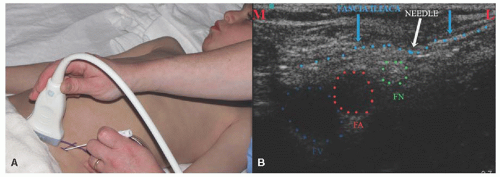 Figure 41.3. A: Needle and probe position for fascia iliaca block. B: Ultrasound scan for fascia iliaca block. FA, femoral artery; FN, femoral nerve; FV, femoral vein; L, lateral; M, medial. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree