Ultrasound-Guided Interscalene Block
Steven L. Orebaugh
Ryan Guffey
Nizar Moayeri
Paul E. Bigeleisen
 Background and indications: Winnie1 first described the interscalene block in 1970. This block is ideal for surgery of the shoulder, distal clavicle, or proximal humerus. It provides anesthesia to the superior elements of the brachial plexus, including the suprascapular nerve and the supraclavicular nerve (C4). It frequently spares the ulnar nerve completely and preserves some motor and sensory function of the radial and median nerves of the forearm and hand. The interscalene block may not cover the superficial cervical plexus completely. This can be supplemented as necessary for surgery involving the lower neck. If surgery includes the anteroinferior or posteroinferior surface of the upper arm, a separate block of the intercostal brachial and medial cuTaneous nerves (T1-T2) may be required. Surgery involving the elbow may be accomplished with the interscalene nerve block as described in the following text with the addition of a second injection of local anesthetic to the inferior trunk of the brachial plexus.
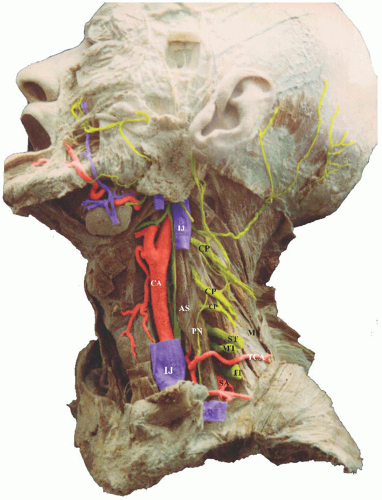
Background and indications: Winnie1 first described the interscalene block in 1970. This block is ideal for surgery of the shoulder, distal clavicle, or proximal humerus. It provides anesthesia to the superior elements of the brachial plexus, including the suprascapular nerve and the supraclavicular nerve (C4). It frequently spares the ulnar nerve completely and preserves some motor and sensory function of the radial and median nerves of the forearm and hand. The interscalene block may not cover the superficial cervical plexus completely. This can be supplemented as necessary for surgery involving the lower neck. If surgery includes the anteroinferior or posteroinferior surface of the upper arm, a separate block of the intercostal brachial and medial cuTaneous nerves (T1-T2) may be required. Surgery involving the elbow may be accomplished with the interscalene nerve block as described in the following text with the addition of a second injection of local anesthetic to the inferior trunk of the brachial plexus. Anatomy: Block of the brachial plexus at this level requires placement of local anesthetic in the interscalene groove, a potential space between the anterior and middle scalene muscles, which is occupied by the nerve elements of the plexus, as well as the subclavian artery. This space typically lies just posterior to the lateralmost extent of the sternocleidomastoid muscle and is exposed when the patient turns the head to the contralateral side (Fig. 16.1). The groove between the anterior and middle scalene muscles can be palpated in most thin patients. It may be difficult to palpate in obese patients and in those patients with limited neck mobility.
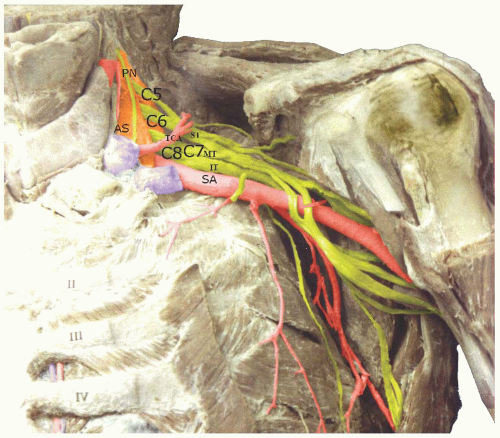
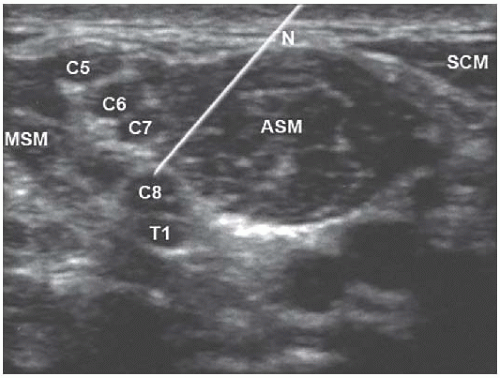
Anatomy: Block of the brachial plexus at this level requires placement of local anesthetic in the interscalene groove, a potential space between the anterior and middle scalene muscles, which is occupied by the nerve elements of the plexus, as well as the subclavian artery. This space typically lies just posterior to the lateralmost extent of the sternocleidomastoid muscle and is exposed when the patient turns the head to the contralateral side (Fig. 16.1). The groove between the anterior and middle scalene muscles can be palpated in most thin patients. It may be difficult to palpate in obese patients and in those patients with limited neck mobility.In the interscalene space, the roots of C5-T1 coalesce to form the superior (C5-C6), middle (C7), and inferior (C8-T1) trunks, which proceed laterally and inferiorly toward the space between the clavicle and first rib and then into the axilla (Fig. 16.2). Several imporTant branches are released from the brachial plexus at this level, including the suprascapular nerve, the dorsal scapular nerve, and the long thoracic nerve.
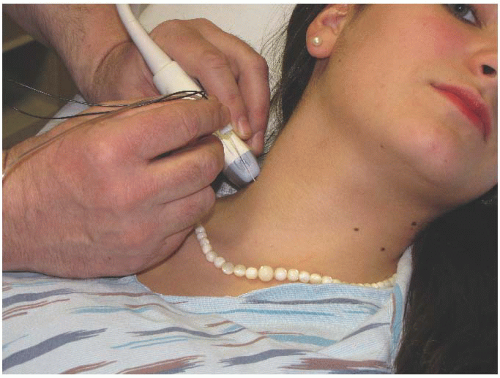
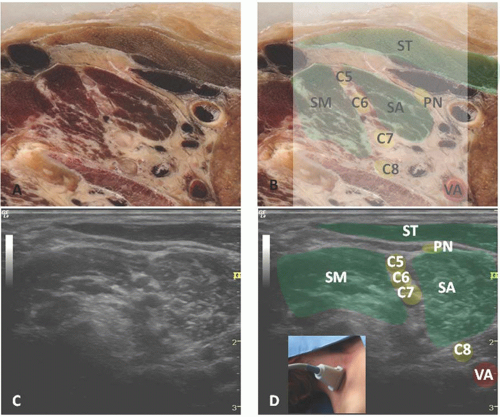
On ultrasound, an appreciation of the anatomy at the level of the roots begins with imaging of a reliable landmark at the base of the neck—that is, the subclavian artery and the brachial plexus, which lies dorsolateral to the artery and superior to the rib (Fig. 16.3). This requires placement of the transducer first in the supraclavicular fossa, in a sagittal oblique orientation (Fig. 16.3). At this level, the nerves appear as a cluster of grapes dorsal and lateral (posterior) to the artery. Upon establishing these landmarks, the transducer should be moved slowly cephalad, tilting the probe more horizontally and following the nerve plexus proximally. This position will reveal the nerve elements (roots) aligning vertically between the scalene muscles (Figs. 16.4 through 16.6). The sternocleidomastoid muscle at this position is usually very attenuated and is visible as a triangular slip of muscle lying superficial to the plexus and
scalene muscles. At this level, the practitioner may be imaging trunks (Fig. 16.4) or roots (Figs. 16.5 and 16.6). In a few patients, the C5 nerve root may pass anterior to or directly through the anterior scalene muscle (Fig. 16.7).
scalene muscles. At this level, the practitioner may be imaging trunks (Fig. 16.4) or roots (Figs. 16.5 and 16.6). In a few patients, the C5 nerve root may pass anterior to or directly through the anterior scalene muscle (Fig. 16.7).
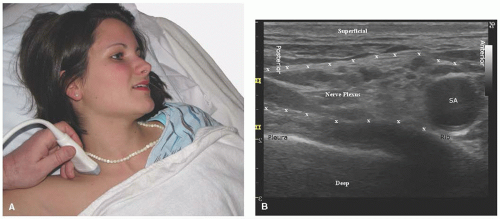 Figure 16.3. A: Probe position in the supraclavicular fossa. B: Ultrasound scan of supraclavicular brachial plexus. SA, subclavian artery. |
The interscalene space is lined by evaginated prevertebral fascia, which proceeds distally with the plexus as a discontinuous sheath (Fig. 16.1).1,4 This fascia is not typically evident on ultrasound imaging; rather, the nerve roots and trunks are sandwiched between the scalene muscles and appear as hypoechoic nodules (Fig. 16.6).2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree