Ultrasound-Guided Blocks at the Elbow and Forearm
Steven L. Orebaugh
Shruthima Thangada
Paul E. Bigeleisen
 Background and indications: Proximal upper extremity blocks on occasion fail to provide anesthesia in all of the nerve territories required for surgery on the forearm or hand. When this occurs, anesthesiologists may choose to provide a more distal block to supplement the brachial plexus block, selectively placing local anesthetic around the nerve that was not adequately anesthetized. Infrequently, respiratory compromise from a pneumothorax or phrenic nerve block may be a complication of supraclavicular or infraclavicular block. This complication can manifest several hours after the procedure is performed. In selected outpatient surgeries, one may consider a distal elbow block in patients susceptible to respiratory complications. Selective block of more distal nerves under ultrasound guidance may also be useful for limited surgical procedures of the forearm or hand, such as open reduction and fixation of a finger, carpal tunnel release, tendon repair, or ganglion cyst removal.1 Although distal extremity blocks are an option in these cases, a recent study demonstrated no significant difference in patient satisfaction when comparing distal extremity to proximal brachial plexus blocks where motor block above the elbow was present.2
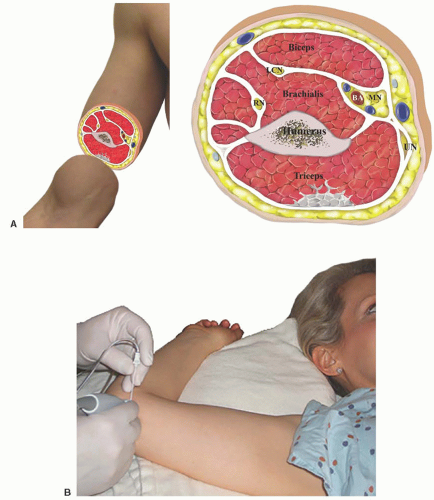
Background and indications: Proximal upper extremity blocks on occasion fail to provide anesthesia in all of the nerve territories required for surgery on the forearm or hand. When this occurs, anesthesiologists may choose to provide a more distal block to supplement the brachial plexus block, selectively placing local anesthetic around the nerve that was not adequately anesthetized. Infrequently, respiratory compromise from a pneumothorax or phrenic nerve block may be a complication of supraclavicular or infraclavicular block. This complication can manifest several hours after the procedure is performed. In selected outpatient surgeries, one may consider a distal elbow block in patients susceptible to respiratory complications. Selective block of more distal nerves under ultrasound guidance may also be useful for limited surgical procedures of the forearm or hand, such as open reduction and fixation of a finger, carpal tunnel release, tendon repair, or ganglion cyst removal.1 Although distal extremity blocks are an option in these cases, a recent study demonstrated no significant difference in patient satisfaction when comparing distal extremity to proximal brachial plexus blocks where motor block above the elbow was present.2 Anatomy: With the aid of ultrasound, the ulnar nerve may be followed from the axilla to the sulcus ulnaris—the bony canal—where it travels through the ulnar groove between the medial epicondyle of the radius and the olecranon process of the ulna. Most authors recommend providing the block 5 cm proximal to the sulcus ulnaris (Fig. 21.1). Here, the nerve is subcuTaneous and amenable to block. Nearer to the elbow, the nerve lies within the sulcus ulnaris (Fig. 21.2). Performing the block within the sulcus ulnaris may lead to high pressures deep to the retinaculum, which confines the nerve to the bony canal in most patients. Injection at the level of the sulcus ulnaris may also lead to a higher probability of intraneural injections, seeing as the nerve is less mobile.3 Immediately below the elbow and lying between the flexor digitorum superficialis and the flexor carpi ulnaris, the nerve is also superficial and easily blocked (Fig. 21.3). More distally, in the forearm, the ulnar nerve courses between the flexor tendon layers. Nearby lie the ulnar artery and median nerve.4,5 At the level of the wrist, the artery and nerve can be seen passing distally into the hand, medial to the carpal tunnel (Fig. 21.4).
Anatomy: With the aid of ultrasound, the ulnar nerve may be followed from the axilla to the sulcus ulnaris—the bony canal—where it travels through the ulnar groove between the medial epicondyle of the radius and the olecranon process of the ulna. Most authors recommend providing the block 5 cm proximal to the sulcus ulnaris (Fig. 21.1). Here, the nerve is subcuTaneous and amenable to block. Nearer to the elbow, the nerve lies within the sulcus ulnaris (Fig. 21.2). Performing the block within the sulcus ulnaris may lead to high pressures deep to the retinaculum, which confines the nerve to the bony canal in most patients. Injection at the level of the sulcus ulnaris may also lead to a higher probability of intraneural injections, seeing as the nerve is less mobile.3 Immediately below the elbow and lying between the flexor digitorum superficialis and the flexor carpi ulnaris, the nerve is also superficial and easily blocked (Fig. 21.3). More distally, in the forearm, the ulnar nerve courses between the flexor tendon layers. Nearby lie the ulnar artery and median nerve.4,5 At the level of the wrist, the artery and nerve can be seen passing distally into the hand, medial to the carpal tunnel (Fig. 21.4).The median nerve remains with the brachial artery in its course through the medial aspect of the arm to the elbow. At the elbow, it can be located quite readily with ultrasonography and found to be medial to the brachial artery (Fig. 21.5). As the median nerve travels distally into the forearm, it initially remains close to the ulnar artery. In the forearm, the median nerve is located between the flexor digitorum superficialis and flexor digitorum profundus. It can be followed with ultrasound scanning into the wrist, where it is seen in the carpal tunnel among the flexor tendons (Fig. 21.6). Voluntary motion by the patient of his or her fingers causes the tendons to “dance,” moving about quite actively while the nerve is less mobile. This may help distinguish these structures from one another.
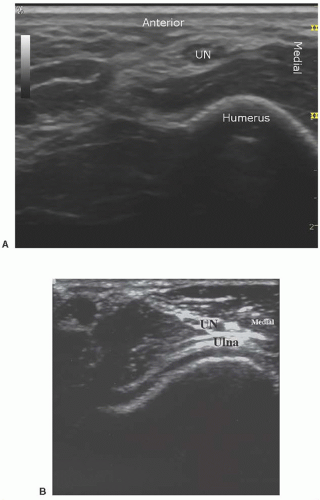 Figure 21.2. A: Ultrasound scan of ulnar nerve above the elbow. UN, ulnar nerve. B: Ultrasound scan of ulnar nerve below the elbow. UN, ulnar nerve. |
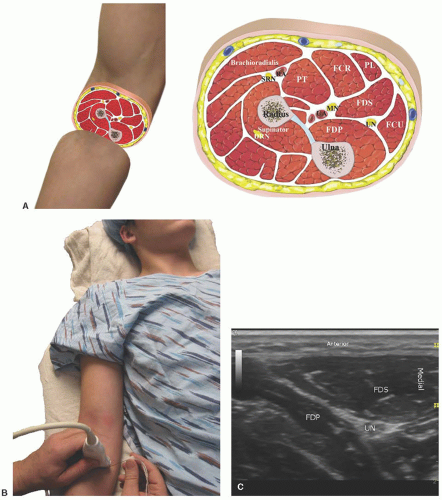 Figure 21.3. A: Gross anatomy below the elbow. DRN, deep radial nerve; FCR, flexor carpi radialis muscle; FCU, flexor carpi ulnaris muscle; FDP,
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|