and Sarah B. Murthi1
(1)
Trauma and Critical Care, R Adams Cowley Shock Trauma Center, Baltimore, MD, USA
Keywords
Point-of-care ultrasoundDopplerM-mode2DB-modePhysics of ultrasoundIntroduction
Ultrasound has uses in heavily resourced as well as remote, underdeveloped regions. It is being studied everywhere, even on the international space station [1]. A good working knowledge of ultrasound is essential when caring for trauma.
Focused assessment with sonography for trauma (FAST) is an important innovation in ultrasound, not because it is a technological advancement, but because it redefines who can use ultrasound and when [2, 3]. The FAST establishes the safety and feasibility of using US to diagnose and manage trauma in real time, thus creating the concept of point-of-care (POC) ultrasound. Currently POC ultrasound includes both diagnostic imaging, like the FAST, and ultrasound for procedural guidance, including central lines and percutaneous drains. More advanced Doppler capabilities make US useful as physiologic measurement tool as well. A variety of cardiac exams can be used to guide complex resuscitation from the trauma bay to the ICU [4–7]. Taken together, the US is a portable stethoscope, CT scanner, and pulmonary artery catheter in one.
History
Ultrasound has been used in medicine since the 1940s, but the technology was understood long before. In the 1700s an Italian physicist, Lazzaro Spallanzani, first recognized that bats used echolocation. With the improved understanding of ultrasound physics, and the discovery of the piezoelectric effect (the coupling of mechanical and electrical forces allowing the interpretation of ultrasound waves), the ability to use US for diagnostics was born. In 1942, Austrian Neurologist Karl Dussik used an “ultrasonic apparatus” to diagnose brain tumors. In 1948 George Ludwig, an American naval officer, first used US to diagnose gallstones. In 1958 Scottish physician Ian Donald pioneered the use of ultrasound for obstetrics. Through the 1950s US technology advanced, from large machines requiring submersion of the patient in fluid, to smaller devices, to modern handheld ultrasounds [8]. With the increasing access and availability, as well as the decreasing cost, US has spread across medical specialties. With tele-sonography and virtually guided sonograms, this market will only continue to grow [9].
Focused Assessment with Sonography for Trauma
Physical exam after trauma is unreliable, as 20–40 % of patients with intra-abdominal bleeding will have a normal exam [10, 11]. Prior to the use of FAST, diagnostic peritoneal lavage (DPL) or surgical exploration was the primary assessment of intra-abdominal bleeding. In most institutions, the FAST exam has essentially replaced the DPL [12]. In the current, 9th edition of ATLS, DPL has become an optional skill station [13], while ultrasound is considered an adjunct to the primary survey. Early investigators realized that fluid is easy to see on ultrasound and that FAST could be used to rapidly, noninvasively detect blood in the pericardium and abdomen [14–16].
The FAST has four views: subxyphoid (SX), right upper quadrant (RUQ), left upper quadrant (LUQ), and pelvic (P). The EFAST adds anterior lung windows to evaluate for PNX [17]. Some centers have added functional evaluation of the heart and the inferior vena cava (IVC) to the FAST [18, 19]. The FAST is a reliable and repeatable exam, with a compressed learning curve. While experience yields improved accuracy, the ability to perform an adequate exam is obtained after only a few exams [20, 21].
In hypotensive patients with blunt abdominal trauma or precordial wounds, FAST is 100 % specific and sensitive for blunt abdominal trauma and 100 % specific and 99.3 % sensitive for precordial wounds [14, 22]. In a blunt trauma patient with hypotension, a FAST showing fluid is an indication for operative exploration. Absence of fluid makes it unlikely intra-abdominal, thoracic, or pericardial bleeding is the cause of hypotension. For penetrating abdominal trauma, FAST is only 25–56 % sensitive in detecting injury [23]. Furthermore, in stable patients with blunt trauma, FAST will miss up to 30 % of injuries, as it misses isolated visceral injury without significant hemorrhage [24–26]. These patients should get further evaluation—usually a CT scan or serial abdominal exams.
In 2004, Kirkpatrick coined the term EFAST and found that the EFAST was comparable in specificity to CXR but had superior sensitivity (48.8 % vs. 20.9 %) in diagnosing PNX. Other series confirm that US is superior to CXR to diagnose PNX but can fail to detect small pneumothoraces [27, 28].
At the Shock Trauma Center, we perform FAST on almost all patients as a positive FAST in a stable patient can result in more rapid work-up and better triage. We also feel it is necessary screen a high volume of patients to maintain ultrasound skills for trainees.
Tips for Learning Ultrasound
Regardless of the exam being performed, the following tips are suggested:
1.
Getting to know your machine: This is the most important factor in safely and reliably using ultrasound.
2.
Clean the transducer and keyboard: Infection control and patient safety are key points that are often overlooked but are critical to patient safety.
3.
Turn the machine on: All machines will have an on/off or power button. It is useful to keep the machine plugged in during and between uses. Machines left on may run low on battery power, and start-up can take longer.
4.
Enter the patient data: Learn how to enter patient data and save the study.
5.
Select the transducer: The appropriate transducer for the desired exam should be selected.
6.
Select the exam type (presets): Generally the machine will default to the last exam. Most machines can be set to start in a particular exam type. Again, it is important to know your machine!
7.
Find the gain and depth controls: Manipulating depth and gain to optimize images.
8.
Get your patience on: BE PATIENT! Even with the FAST exam, slow and steady scanning through more than one plane is very important.
Pathology in the FAST and EFAST
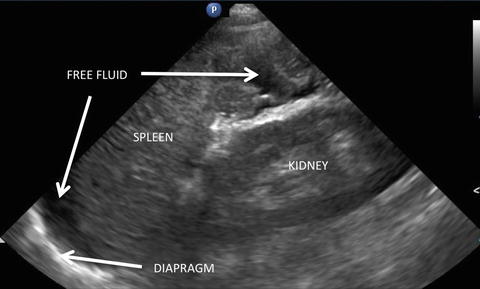
Diagnosis of Intra-abdominal Hemorrhage: Fluid will appear black and collect in dependent portions of the abdomen. It is assumed that “fluid” is blood in a trauma patient; however, it could be ascites, free bladder rupture, or bowel contents (Fig. 7.1). In addition, clotted blood is echogenic and can mimic the appearance of solid organs.


Fig. 7.1
FAST of RUQ with fluid in Morrison’s pouch.
Diagnosis of Pneumothorax: Diagnosis of a PNX has a steep but short learning curve. A normal lung on the contralateral side makes comparative diagnosis easier. US cannot penetrate air, so the finding is a loss of signal in the potential space between the parietal and visceral pleura of the chest. Normally, the parietal/pleural interface “slides,” creating a sparkle or dancing effect, termed sliding. Comet tails (also called b-lines) can also be seen. These hyperdense lines originate at the pleural interface and will flash intermittently from the pleural line, almost like a small flashlight. Comet tails (Fig. 7.2) are a reverberation artifact, likely arising from congested pulmonary vasculature in contact with the pleural interface, and can be a sign of pulmonary edema. If pleural surfaces are intact, transmitted cardiac pulsations can be seen on the left side. When a PNX is present, sliding, comet tails, and pulsations are lost. A lung point occurs when the transition from sliding to no sliding can be clearly seen; it is 100 % specific for the diagnosis of PNX [29]. Lack of lung sliding alone can be caused by other processes including pneumonia, bullous disease, and other pleural pathologies.
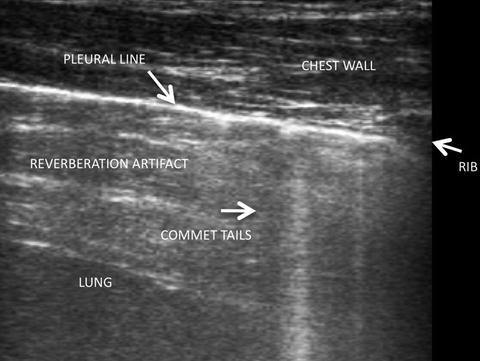
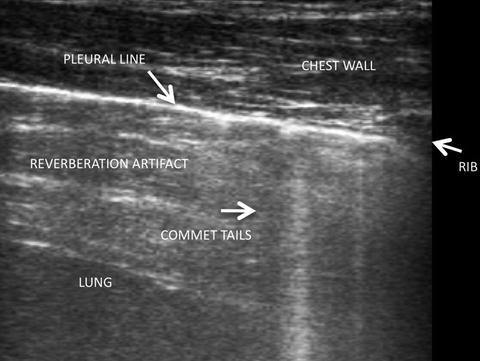
Fig. 7.2
Comet tails demonstrated across a fluid-filled lung.
M-mode can help confirm the PNX diagnosis and may be very helpful when initially learning to detect it, but the assessment can be entirely made from 2D imaging. On M-mode, a normal parietal/visceral interface will show the bright line of pleura with a smattering of signal returning to the probe from the lung parenchyma, called seashore sign. If air is present from a PNX, it will stop the signal, and instead of seashore sign, there will be a series of horizontal lines sometimes called barcode or stratosphere sign (Fig. 7.3).
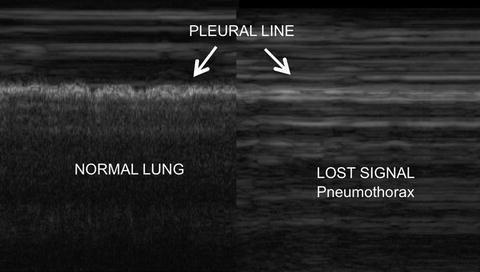
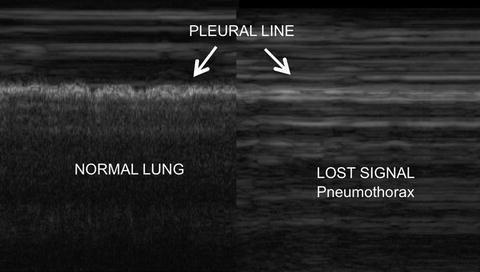
Fig. 7.3
Stratosphere sign (right) indicating loss of signal from pleural slide, pathognomonic for pneumothorax.
Summary of FAST (Fig. 7.4)
Fig. 7.4
Four transducer views on the FAST exam plus 2 views of the lungs added in the EFAST.
Classic FAST Windows
Get Clinical Tree app for offline access

1.
SX: The transducer is placed below the xyphoid, with the indicator to the right, and pointed to the left shoulder, attempting to look “under” the xyphoid to the heart.
Critical Image: In the space between the right ventricle and the liver, blood will appear as a black stripe below the pericardial bright white strip (Fig. 7.5).
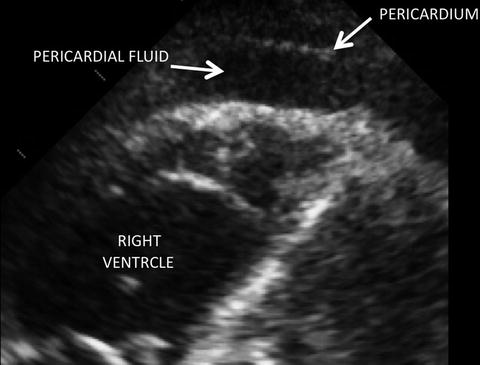
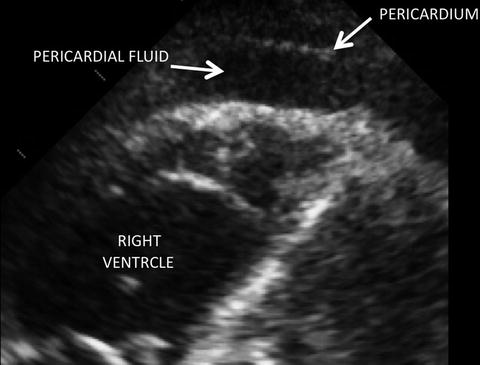
Fig. 7.5
A positive SX view on FAST. Note the fluid between the pericardium and ventricle.
PITFALL—in the case of penetrating cardiac trauma, blood can decompress into the chest rendering the pericardial window negative. In this case, thoracic ultrasound (or chest X-ray) will show a hemothorax. Suspicion of a cardiac injury must remain high.
2.
LUQ: The transducer is moved to the posterior axillary line, below the costal margin on the left side. It may be necessary to press your knuckles into the gurney and orient the transducer anteriorly, as the view can be very posterior. Start at the costophrenic angle and then move caudally until the kidney comes into view. The probe should be fanned across the entire kidney. The space between the spleen and diaphragm should be viewed to avoid missing fluid above it. A simple cephalic sweep allows visualization of the lung fields, but at times the probe needs to be moved to adequately visualize above the liver. Over one or two respiratory cycles, one can easily evaluate for fluid in the thoracic cavity.
Critical Image: Fluid will appear as a black stripe above the kidney, separating it from the spleen (Fig. 7.6). The area above the diaphragm fluid will appear as a dark collection above the diaphragm or in the most dependent part of the chest.