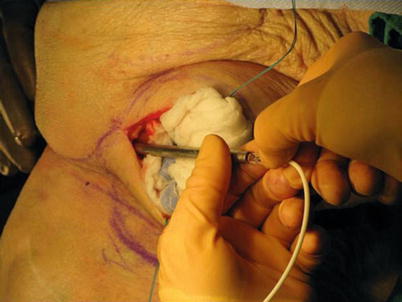
Fig. 39.1
Marking the skin for the tunneling course using the two-step technique
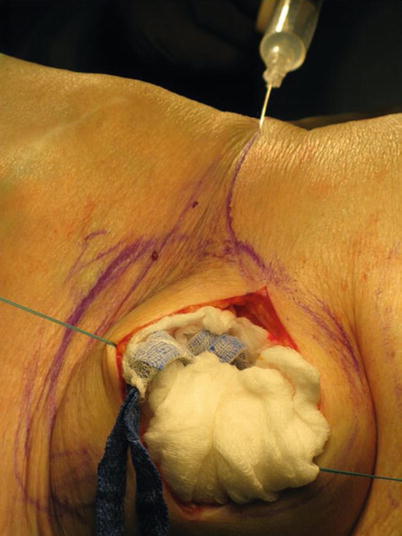
Fig. 39.2
Local anesthesia for tunneling
Once the patient has been properly anesthetized by using local anesthesia and intravenous sedation, or intrathecal analgesia, the physician is ready to tunnel. Conventional tunneling rods are of fairly large diameter and require passage over a distance that may lead to improper depth. This problem can be managed by bending the tunneling device to the contours of the body, or by making a two-pass tunneling approach. In this method, the physician makes an incision along the course of the tunneling path, tunnels to that incision, and then tunnels in a second step to complete the catheter pass. Figures 39.3 and 39.4 show the options for the one-pass and two-pass methods. Figure 39.5 demonstrates the placement of the catheter into the tunneling rod.
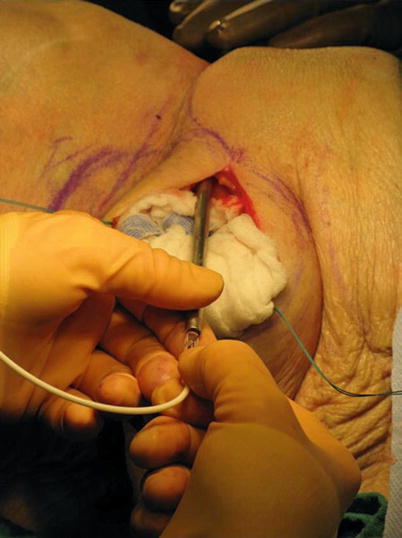


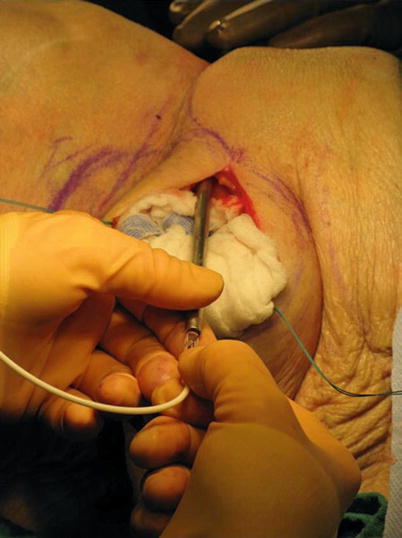
Fig. 39.3
Completion of step one with the tunneling rod in the spinal incision

Fig. 39.4
Two-pass tunneling approach

Fig. 39.5
Placement of the lead into the tunneling rod
During the course of tunneling, the physician should use palpation to determine that the tunneling rod is staying at proper depth. Ideally, the tunneling rod should be palpable in the subcutaneous tissue, deep enough to avoid invading the dermis, but superficial enough to avoid penetrating unintended structures (Figs. 39.6 and 39.7).
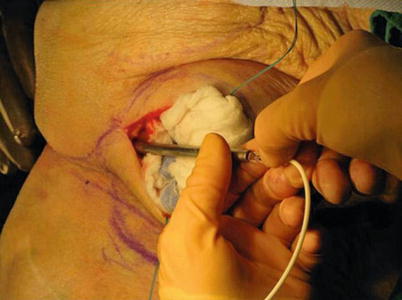

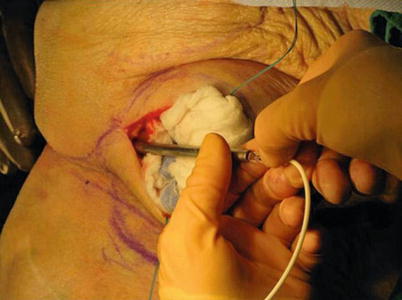
Fig. 39.6
The tunneling rod must stay in the proper tissue plane to ensure that the lead is not superficial, which can lead to erosion, or deep, which can result in patient injury

Fig. 39.7
The tunneling rod should be palpable as it is passed in the tissue to monitor depth
The physician may tunnel from the spinal incision to the pocket or from the opposite direction. Regardless of the direction chosen, the physician must be aware of the risk of injuring the catheter as it enters the spinal structures, and should be vigilant in avoiding the catheter on either entry or exit of the tissues with the rigid tunneling device. Once tunneling is completed, the catheter should be prepared in the pocket for attachment to the pump with proper trimming and confirmation of proper cerebral spinal flow (Fig. 39.8). To help avoid catheter migration, a strain relief loop should be created in the spinal incision prior to wound closure.